Published online Apr 7, 2020. doi: 10.3748/wjg.v26.i13.1394
Peer-review started: December 18, 2019
First decision: February 18, 2020
Revised: March 5, 2020
Accepted: March 10, 2020
Article in press: March 10, 2020
Published online: April 7, 2020
Processing time: 111 Days and 1.1 Hours
Colorectal cancer (CRC) is the third most common diagnosed malignancy among both sexes in the United States as well as in the European Union. While the incidence and mortality rates in western, high developed countries are declining, reflecting the success of screening programs and improved treatment regimen, a rise of the overall global CRC burden can be observed due to lifestyle changes paralleling an increasing human development index. Despite a growing insight into the biology of CRC and many therapeutic improvements in the recent decades, preclinical in vivo models are still indispensable for the development of new treatment approaches. Since the development of carcinogen-induced rodent models for CRC more than 80 years ago, a plethora of animal models has been established to study colon cancer biology. Despite tenuous invasiveness and metastatic behavior, these models are useful for chemoprevention studies and to evaluate colitis-related carcinogenesis. Genetically engineered mouse models (GEMM) mirror the pathogenesis of sporadic as well as inherited CRC depending on the specific molecular pathways activated or inhibited. Although the vast majority of CRC GEMM lack invasiveness, metastasis and tumor heterogeneity, they still have proven useful for examination of the tumor microenvironment as well as systemic immune responses; thus, supporting development of new therapeutic avenues. Induction of metastatic disease by orthotopic injection of CRC cell lines is possible, but the so generated models lack genetic diversity and the number of suited cell lines is very limited. Patient-derived xenografts, in contrast, maintain the pathological and molecular characteristics of the individual patient’s CRC after subcutaneous implantation into immunodeficient mice and are therefore most reliable for preclinical drug development – even in comparison to GEMM or cell line-based analyses. However, subcutaneous patient-derived xenograft models are less suitable for studying most aspects of the tumor microenvironment and anti-tumoral immune responses. The authors review the distinct mouse models of CRC with an emphasis on their clinical relevance and shed light on the latest developments in the field of preclinical CRC models.
Core tip: This review highlights the different approaches to model colorectal cancer in the mouse. Carcinogen-induced rodent models, genetically engineered mouse models, heterotopic and orthotopic models as well as patient-derived xenografts are discussed with an emphasis on their specific advantages and disadvantages. Moreover, the historical background of animal models for cancer research and the future perspectives of colorectal cancer research are reviewed as well.
- Citation: Bürtin F, Mullins CS, Linnebacher M. Mouse models of colorectal cancer: Past, present and future perspectives. World J Gastroenterol 2020; 26(13): 1394-1426
- URL: https://www.wjgnet.com/1007-9327/full/v26/i13/1394.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i13.1394
Colorectal cancer (CRC) is the third most common diagnosed malignancy among both sexes in the United States as well as in the European Union[1,2]. A decrease in the incidence and overall mortality of CRC in countries with a very high development index over the last decades can be attributed to an interplay of screening programs with detection of precancerous lesions or early stage cancers on the one hand[3,4], and improved therapeutic concepts leading to an increased stage adjusted survival for all stages of CRC on the other hand[5]. This development is in sharp contrast to countries with a rapidly growing high development index. Together with an increased CRC incidence and mortality this reflects an adoption of the so-called “western lifestyle” including the risk factors for CRC. While obesity, smoking and red meat consumption are significantly associated with an elevated CRC risk[6], physical activity, high vegetable, fruit and fiber intake as well as metronomic aspirin therapy, have shown to decrease CRC risk[7,8]. Besides these modifiable risk factors, a variety of genetic factors influences CRC risk. About 5% of CRC cases are caused by hereditary, highly penetrant cancer syndromes, like familial adenomatous polyposis (FAP) and Lynch syndrome (LS); whereas up to 20%-30% of cases are considered as “familial” due to different germline mutations of varying penetrance[9]. Since the discovery of the link between APC germline mutations and FAP[10], followed by the genetic pathology of LS in the early 1990s[11,12], a myriad of mutations contributing to CRC genesis has been identified, constantly reshaping the genomic landscape of the disease[13]. The ideal model of CRC should recapitulate the progress from a precancerous adenoma to an invasive carcinoma with metastatic potential and at the same time it has to reflect the inter-individual molecular diversity of the disease. Consequently, a single (mouse) model of CRC simply cannot match all of these requirements. In this review, we discuss the different mouse models of CRC with their distinct advantages and disadvantages with a focus on their translational and clinical relevance.
Carcinogen-induced models (CIM) in rodents look back on a long tradition but maintained their usefulness for certain applications to the present day. They provide a platform for dietary studies and give insights into the pathways of food-borne carcinogens and colitis-associated carcinogenesis. Administration of the chemical compounds is possible via ad libitum feeding, oral gavage, intraperitoneal/ subcutaneous (s.c.) or intramuscular injection, or enema.
In 1915, Yamagiwa et al[14] proofed the carcinogenic properties of coal tar by its repetitive application on the ears of rabbits. At about the same time, first researchers worked on colon carcinogenesis by applying chemical or radioactive substances[15-17]. In the 1960s, cycasin and its metabolite, methylazoxymethanol, have shown to induce cancers in rodents[18-20]. In the following years, the more chemically stable substances, azoxymethane (AOM) and its precursor molecule, 1,2-dimethylhydrazine as well as methylazoxymethyl acetate, were extensively used to induce colon carcinogenesis in mice and rats. All three compounds are metabolized to methylazoxyformaldehyde, which is able to alkylate the DNA bases guanine and thymine[21]. After being processed by Phase-II-reaction, it is secreted to the bile and exceeds its carcinogenic effect to the intestinal mucosa[22]. Interestingly, these compounds show different carcinogenic potential depending on the mouse strain, housing conditions and the way of administration[23-25]. Although most authors claim a certain organotropism for AOM and dimethylhydrazine, tumor formation happens mostly in the small intestine and relevant amounts of alkylated DNA adducts can be observed in the liver and the kidneys[26]. Moreover, intestinal carcinogenesis can be achieved by the oral or rectal application of the direct alkylating topic agents N-methyl-N-nitrosourea (MNU), 3,2’-dimethyl-4-aminobiphenyl and N-Methyl-N’-nitro-N-nitrosoguanidine of which the latter two are traditionally used in rats[27-29].
Other carcinogens gained attention in connection with the association between meat consumption and increased CRC risk[30]. Heterocyclic aromatic amines (HAA) form from the reaction between free amino acids, sugars and creatine at high temperatures during the cooking process of meat and fish[31], whereby 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) and 2-Amino-9H-pyrido[2,3-b]indole are the most abundant HAA in various foods[32]. PhIP is metabolized by the liver enzyme CYP1A2 to N2-Hydroxy-PhIP, which then, after sulfation or acetylation, forms activated esters capable of DNA adduct formation[33]. Detoxification of PhIP and its metabolites is driven by glutathione conjugation and glucuronidation[34,35]. Glucuronide conjugates are excreted through urine and bile[36]. In case of the latter, hydrolyzation by bacterial beta-glucuronidases in the intestines liberate reactive PhIP metabolites, which not only affect the intestinal mucosa, but undergo enterohepatic circulation[37]. Important to consider is, that the metabolism of PhIP in rodents results in less reactive metabolites than in humans, and its carcinogenic potential measured in animal studies might be even higher in humans[38]. Nakagama et al[39], by combining a high fat diet with PhIP intake, showed the tumor enhancing properties of this food borne agent simulating the carcinogenic effects of the s.c. “western diet”. Moreover, PhIP led to the formation of high-grade dysplasia and adenocarcinomas in a mouse model of chemical induced colitis[40]. Although other common foodborne HAAs have shown to induce dysplasia and carcinomas in rodents[41], they are rarely used for modelling colon carcinogenesis. Polycyclic aromatic hydrocarbons, as benzo[a] pyrene, may be used for chemoprevention studies but are insignificant for CRC modeling in general[42,43]. Dextran sodium sulfate (DSS) must also be mentioned when discussing chemical-induced CRC mouse models. Since the first report of an DSS-induced colitis model nearly 30 years ago[44], countless studies used DSS to simulate chronic inflammatory bowel diseases and we would recommend the reader to refer to excellent reviews discussing inflammatory bowel diseases and DSS[45]. As a sulfated polysaccharide, DSS directly damages the colonic epithelium resulting in an impairment of the mucosal barrier with consecutive entry of luminal bacteria and associated antigens into the mucosa, triggering inflammation[46]. Depending on the animal strain, DSS dosage and administration regimen, mice can develop acute and chronic colitis or even colitis-induced dysplastic lesions[47-50]. DSS in combination with carcinogenic compounds, primarily AOM, has been proven useful for the research of colitis-induced cancer[51]. By use of mice with germline Apc mutation (APCMin mice) for DSS treatment, the rate of dysplasia and carcinoma formation was further enhanced[52]. Cooper et al[53] reported an increased CRC incidence of 40% in APCMin mice after two cycles of 4% DSS treatment compared to untreated control animals and identified the loss of heterozygosity (LOH) of Apc as underlying cause.
Chemical-induced mouse models are not homogenous and possess specific advantages and disadvantages. They are by far the oldest method inducing CRC in animals and a multitude of studies has been traditionally carried out in rats and other rodents diminishing the comparability of older data with more recent results. Most models reflect very well the progression from aberrant crypt foci to adenomas to carcinomas of the human adenoma-carcinoma sequence[54]. Therefore, they are still useful to evaluate the influence of diet[55], dietary supplements[56,57], chemopreventive interventions[58,59] and the gut microbiome[60]. Especially the combination of DSS with carcinogenic agents provided many insights in the link between CRC and inflammation[61]. However, chemical-induced carcinomas rarely show invasive properties and local or distant metastases are usually absent. Albeit Yang et al[62] reported lymph node metastases in an intrarectal MNU-model, the use of shrews (phylogenetic unrelated to rodents) as test animals interdicts the comparison to rodent animal models. A further exception is the work of Derry et al[63], who could observe a relevant number of lung metastases in an AOM-induced mouse model, which is to our knowledge the only report of metastatic spread in a chemical-induced mouse model. Besides the lack of invasiveness, a lot of CIM show a high latency from the first application to tumor development. Depending on the carcinogen, dosing protocol and mouse strain, latencies from 24 to 50 wk were reported[64-66]. By combining the carcinogen with DSS, the time to tumor development can be notably shortened to 10-18 wk[23,67]. Although the minority of sporadic CRC patients show synchronous adenomas[68,69], nearly all CIM show a “carpeting” of the colonic mucosa with polyps[70]. Tumor formation is not restricted to the colon, but can be commonly observed in the whole gastrointestinal tract[71,72]. Moreover, MNU additionally induces leukemia and lung adenomas[73] and PhIP leads to formation of mammary and prostate neoplasia[74]. Another complexing aspect of CIM concerns the genetic aberrations associated with the adenoma-carcinoma sequence, i.e., the accumulation of mutations, predominantly affecting APC, KRAS and P53[75]. While the AOM model shows frequent Kras and β-catenin mutations, Apc and P53 are rarely affected[76-79]. In contrast PhIP, IQ and MNU lead to Apc mutations, but show no P53 or Kras mutations[21]. In general, the vast quantity of different dosing protocols, application forms and animal strains, makes direct comparisons and the selection of the right CIM difficult[54]. Another aspect, not to be neglected, is the agenda of animal welfare. Quite a few protocols lead to significant weight loss and diarrhea, which is, in combination with often long study durations, detrimental for the animal wellbeing[80].
With the knowledge explosion concerning the genetic pathways altered in CRC at the end of the 20th century, the scientific community demanded specific genetic mouse models to focus on certain molecular mechanisms of colorectal carcinogenesis.
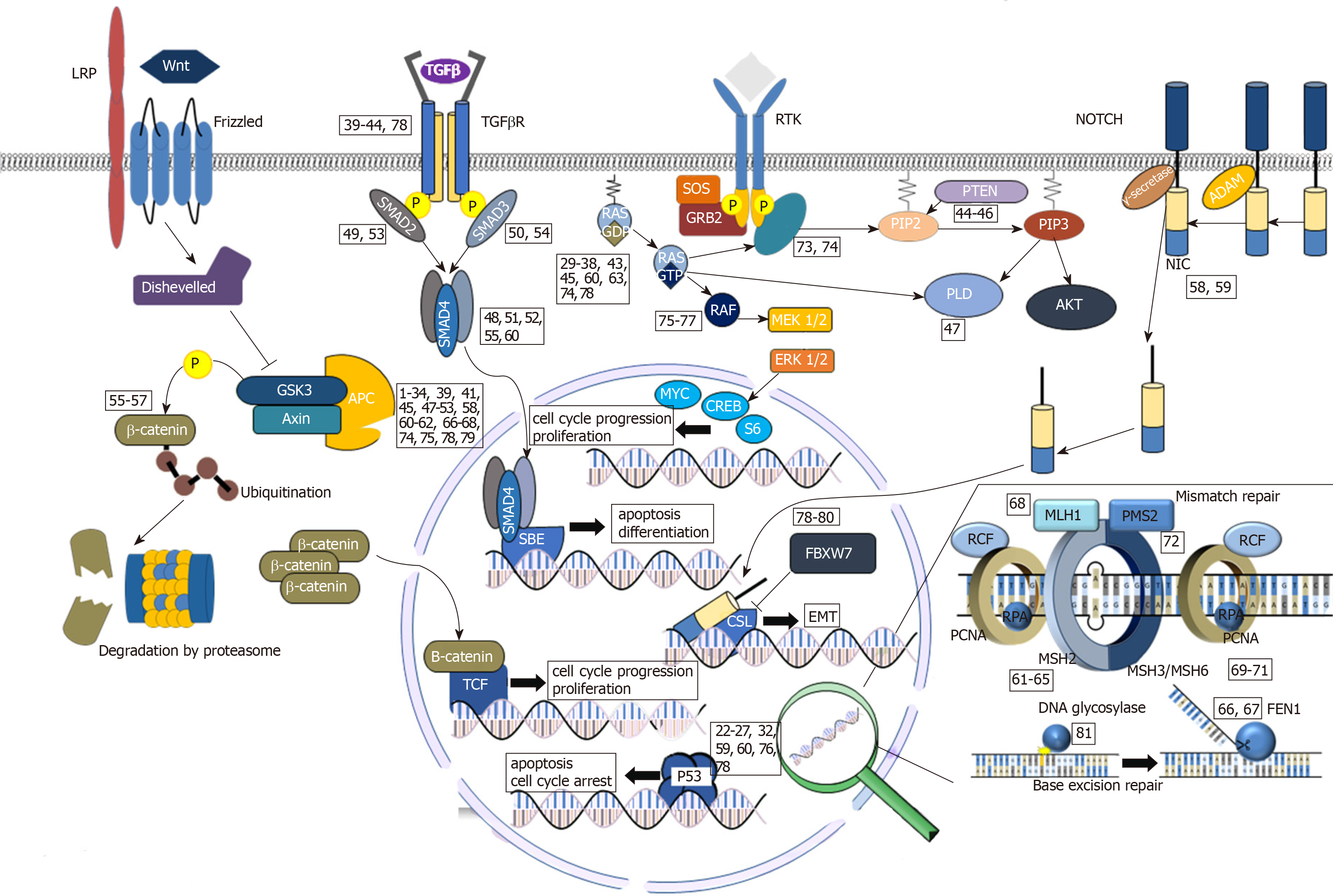
In the 1980s, the first genetically engineered mouse models (GEMM) of brain tumors, lymphoma, pancreatic cancer, breast cancer and osteosarcoma emerged[81-87]. Based on the groundbreaking work of Evans, Smithies and Capecchi[88] on gene targeting, the first tumor suppressor knock-out mouse models emerged in the early 1990s[89,90]. To circumvent the obstacle of frequent embryonic lethality caused by germline knock-outs of tumor suppressors, Cre-loxP mediated mouse models were designed to allow the tissue specific and conditional knock-out of tumor suppressor genes or activation of oncogenes, respectively[91-93]. Interestingly, the very first GEMM of CRC, the APCMin mouse, was created without sophisticated methods. Moser et al[94] showed, that the application of N-ethyl-N-nitrosourea leads to nonsense mutations in codon 380 of the Apc gene and subsequent breeding of these animals established the first model for multiple intestinal neoplasia. APCMin mice develop a large number of adenomas in the small intestine after 120-140 d due to LOH and show a high mortality with increasing age as a result of intestinal obstruction and anemia without progression to invasive carcinoma[95]. While these models contributed to the understanding of the early stages of FAP, they do not reflect the majority of spontaneous CRC[96]. Since a homozygous Apc mutation is lethal during embryonic development, breeding of homozygous APCMin mice is impossible[97]. However, additional treatment of APCMin mice with AOM or other carcinogenic compounds increases malignancy of the resulting tumors and simultaneously shortens the time to tumor development[98-100]. Till the present day, these models are in use for chemoprevention studies[101,102] and have enormously contributed to the understanding of the early tumor initiating events[103]. Interestingly, a change from C57BL/6 to a hybrid genetic background can extend the lifespan of APCMin mice beyond one year, resulting in a high proportion of invasive adenocarcinoma[104]. Sødring et al[105] changed the APCMin genetic background from C57BL/6 to A/J mice resulting in increased tumor formation in the colon, with a reasonable number of tumors progressing to carcinomas. Transgenic mice with alternative Apc mutations, like the APC+/1638 mouse[106,107], the APCΔ716 mouse[108] and the APCΔ242/+ mouse[109] vary in tumor count and histopathology. Tumor formation predominantly in the small intestine instead of the colon is the major flaw of most Apc-based mouse models. Colnot et al[110] designed the APCΔ14/+ mouse, which shows a more severe phenotype with invasion of the muscularis, an increased lethality and a higher colonic tumor burden compared to APCMin mice but unfavorably still shows relevant tumor development in the small intestine. Early attempts of combining Apc mutations with homozygous P53 knockouts yielded conflicting results, with either no increase[111,112], or a small increase of gastrointestinal malignancy[113]. The most likely explanation is that in human cancers P53 missense mutations frequently act in a dominant negative fashion, overruling the tumor-suppressive function of the wildtype allele[114,115]. In contrast, targeting Kras without tissue specific promoters leads either to embryogenic lethality[116] or few viable animals succumbing to rapidly developing lung tumors[117]. To avoid abundant distribution of mutations in the whole organism, transgene expression controlled by a tissue specific gene promotor, most commonly by application of the Cre-loxP-system[91], has proven to be extraordinarily useful. Many workgroups used Villin-Cre transgenes to restrict recombination of floxP-flanked genes to the epithelial cells of the small and large intestines either with a constitutive expression (Vil-Cre) or with a tamoxifen-inducible expression (Vil-Cre-ERT2)[118]. Another option of site-specific Cre expression is the fatty acid binding protein liver Cre transgene (Fabpl Cre), which can be combined with a tetracycline-inducible tet-on system[119]. Yet, both transgenes’ expression is not limited to the large intestine: While Villin-Cre is expressed in the epithelial cells of the whole intestines, Fabpl-Cre expression can be detected in the distal small intestine, cecum and colon[119,120]. Also, the AhCre strain, carrying Cre under control of the Cyp1A promotor, is commonly used for colon cancer models[121,122]. Here, Cre-expression is induced by β-naphthoflavone in the liver and intestines, but constitutive recombination can be observed in other tissues like the renal epithelium[123]. To achieve a more colon specific expression of Cre-recombinase, Hinoi et al[124] constructed a transgene of Cre and the promotor region of the CDX2 homeobox gene. By inserting a guanine repeat tract to this transgene (CDX2P9.5-G22Cre), stochastic activation of Cre-expression by means of spontaneous frameshift mutations leads to a mosaic-like recombination in the mucosa of the terminal ileum, cecum, and colon[125]. At last, carbonic anhydrase 1 promoter/enhancer-Cre recombinase transgene (CAC) facilitates recombination strictly limited to the large intestine[126]. Paralleling Cre-transgene implementation, others achieved spatiotemporal oncogene expression in the large intestine by delivering Cre by viral transfection via transanal injection, surgery or colonoscopy[127-129] leading to exquisite models of CRC with metastatic spread[130]. Supplied with this comprehensive genetic toolbox, a plethora of CRC mouse models were generated and used to evaluate the role of different mutations and their interplay. Among the non-hypermutated tumors, the most frequently mutated genes are APC, P53, KRAS, PIK3CA, FBXW7, SMAD4, and TCF7L2[13]. The role of Apc LOH as a driver mutation is highlighted in several mouse models. While generalized deletion of both Apc alleles (Apcflox/flox) leads to rapid death by disorder of cell differentiation[131], mice with a mosaic–like deletion of both Apc genes die rapidly from florid polyposis[125]. Depending on the type and modality of Apc mutation, heterozygotes develop adenomas or invasive adenocarcinomas[120,132,133]. Whilst mutated Kras alone is insufficient to induce colorectal tumorigenesis, it increases the susceptibility of the intestinal mucosa to chemical carcinogenesis[134] and leads to accelerated tumor formation in combination with Apc loss[122,135]. Nras mutation, in contrast, does not alter the effect of Apc loss[136]. In humans, P53 mutations are often associated with vascular and lymphatic invasion and advanced cancer stages[137,138]. In fact, the combination of Apc mutation with a dominant-negative P53 mutation leads to increased invasiveness of intestinal tumors with signs of epithelial to mesenchymal transition[139,140]. Also, loss of P53 in a constitutively active Notch signaling background leads to intestinal tumor formation and metastasis[141], whereas Notch signaling does not cooperate with the Wnt-pathway[142]. Nevertheless, Apc deficiency seems to represent a key prerequisite of cancer progression, since Apc restoration leads to spontaneous tumor regression of Kras-mutated, P53-deficient adenocarcinomas[143]. FBXW7 codes for the F-box/WD repeat-containing protein 7, the substrate receptor of a ubiquitin ligase, which degrades several proto-oncogenes like MYC, CCNE1, NOTCH1 and JUN and acts synergistically with P53 as haploinsufficient tumor suppressor[144-146]. Intestinal Fbxw7 deletion enhances tumor development in an ApcMin/+background[147] and a combined deletion of Fbxw7 and P53 results in highly aggressive intestinal cancers with metastatic spread to the lymph nodes and liver[148]. The PI3K/AKT- pathway is well known for its pro-oncogenic and anti-apoptotic signaling and PI3K mutations are common in CRC and many other human cancers[149]. As demonstrated by Leystra et al[150], the intestinal expression of a constitutively active Pi3k (PIK3ca) is a sufficient driver mutation to induce rapid tumorigenesis with invasion of adjacent organs and addition of PIK3ca to a homozygous loss of Apc, drives adenoma-to-carcinoma progression with metastatic spread[129]. Although loss of Pten, the counterpart of Pik3, does not affect intestinal cell proliferation; in the context of Apc deficiency or other mutations, it promotes cancer progression[151-153]. SMAD4 is considered as a tumor suppressor, similar to other constitutes of the TGFβ-pathway[154,155]. Since the genes Apc, Smad2 and Smad4 are all located on chromosome 18 in the mouse, they are suited to generate distinct cis- and trans compound heterozygotes by meiotic recombination. Compared to their single mutation littermates, mice with combined Apc and Smad4 mutations, show accelerated tumor development[156] and increased malignancy[157,158]. In contrast, compound heterozygotes of Apc and Smad2 mutations show no increased tumor development compared to littermates with a single Apc mutation[159]. Notably, homozygous Smad3 mutation leads to aggressive CRC with lymphatic spread and, upon Apc deficiency, drastically reduced life span[160,161]; but SMAD3 is rarely mutated in human CRC[162]. Findings from several CRC-GEMM highlight the role of TGFβ-signaling as a strong tumor suppressor, since Tgfβ[163-165], as well as Tgfβ-receptor 2[140,166,167] knockout, induce local invasion and metastatic spread. Regarding the role of TCF7L2 mutations in CRC, so far, no GEMM of CRC addressing this topic have been published. Besides the conventional adenoma-carcinoma sequence, the serrated pathway represents an alternative route of CRC development with distinct molecular and clinical features. The underlying BRAFV600E mutation occurs in 15%-20% of sporadic CRC, causes a constitutive activation of the MAPK/ERK pathway and is strongly associated with the CpG Island methylator phenotype and microsatellite instability (MSI) due to MLH-1 methylation[168-170]. BrafV600E causes crypt hyperplasia and combined with Apc or P53 mutations, as well as mutations affecting Ink4A/Arf, gives rise to invasive carcinomas[171-174]. Although not common in human CRC, mutation of the GSK3-β phosphorylation site causes degradation-resistant β-catenin[175,176], and has been remodeled in the mouse. GSK3β-resistant β-catenin increases proliferation of the intestinal epithelium and causes adenoma formation, but does not mediate malignant progression[177-179]. Paralleling the research on canonical cancer pathways, there has been reasonable effort to reproduce MSI, a hypermutable phenotype caused by malfunction of DNA mismatch repair (MMR) enzymes[180,181]. MSI-CRC can occur in the context of hereditary MMR gene mutations (LS) or can be detected in up to 15% of spontaneous CRC, caused by hypermethylation of MMR genes (spMSI)[182,183]. The constitutes of the MMR machinery have been extensively studied by somatic knockout models. Since the knockout of the MMR genes MLH1[184], MSH2[185,186], MSH6[187] and PMS2[188] predominantly cause hematopoietic malignancies with consecutive reduced lifespan in the mouse and consequently only a minor fraction of homozygotes develop intestinal neoplasia[189,190], these knockouts were frequently put in an APC deficient setting, to increase intestinal carcinogenesis[184,191,192]. Kucherlapati et al[193,194] demonstrated, that mutations of Fen1 and/ or Exo1, both cooperation partners of MMR enzymes, lead to similar patterns of MSI tumor development. However, MSI-high tumors rarely show activation of the Wnt-pathway and are typically chromosomal stable, whereas APC mutations are typically associated with a chromosomal instable phenotype[195,196]. Therefore, these models do not adequately recapitulate Lynch-type or spMSI tumors. To overcome the aforementioned obstacles, a floxed Msh2 allele was combined with either a LS related missense mutation (Msh2G674D) or an Msh2Δ7 null mutation in mice carrying a Villin-Cre transgene, leading to intestinal carcinogenesis and chemoresistance typical for MSI-high tumors[197]. An overview of the above addressed mutations can be found in Figure 1 and are summarized in Table 1.
| Link to Figure 1 | Ref. | Methods | Results |
| 1 | [127] | loxP flanked Apc exon 14 (Apc580S) | Adenoma formation in the distal rectum in most of the Apc580S homozygotes. 50% of animals show invasive adenocarcinoma after 1 yr without lymphatic or distant metastases |
| Colorectal tumor induction by rectal infection with Cre-delivering Adenovirus (AxSRαCre) | |||
| 2 | [109] | ApcΔ242/+ | Adenomas: Higher in numbers but smaller in size and no differences in histology compared to ApcMin/+ mice |
| 3 | [110] | ApcΔ14/+ | Shift of tumor distribution, more severe phenotype, invasion of muscularis propria, 50% dead after 12 mo |
| 4 | [120] | Fabpl-Cre; Apc15lox/+ | Increased survival due to lower number of tumors, but larger tumors predominantly in the colon, 91% at least low-grade adenoma, 50% carcinoma; invasiveness and metastases not reported |
| 5 | [108] | Apc+/Δ716 (C57BL/6J background) | Intestinal polyposis with emphasis on the small intestine |
| 6 | [126] | Cac; Apc580S/+ | Transgene expression limited to the large intestine. Adenoma formation without malignancy |
| 7 | [125] | CDX2P9.5-G22Cre | Frameshifted Cre-recombinase with a long guanine nucleotide tract under control of the homeobox promotor CDX2P9.5 leads to limited activation of Cre by spontaneous somatic mutations in the large intestine: Apcflox/flox homozygotes dye rapidly from florid polyposis of proximal colon and cecum |
| Apcflox/flox | |||
| 8 | [374] | Apc+/Δ716 Cdx2+/− | Increased adenoma formation in the colon, reduced number of polyps in the small intestine |
| 9 | [132] | Apc+/fle1−15; Villin-Cre mice (conditional) and ApcΔe1−15 constitutive null allele | More severe polyposis compared to ApcMin/+ mice |
| 10 | [375] | BubR1+/–ApcMin/+ | Increased tumor formation in the large intestine and higher malignancy through increased chromosomal instability (invasiveness and metastases not reported). Note, that BUBR1 mutations are uncommon in CRC[376] |
| 11 | [377] | ΔcyEphb2;ApcMin/+ | Reduced tumor formation in the small intestine, but large adenocarcinomas of the colorectum |
| Ephb3+/-;ApcMin/+ | |||
| Ephb3-/-;ApcMin/+ | |||
| 12 | [133] | CDX2P-CreERT2Apcflox/flox | Tamoxifen inducible Apc-knockout in the distal intestine |
| 13 | [378] | long living ApcMin/+ mice | Some adenomas progress to adenocarcinomas |
| 14 | [104] | C57BL/6J ApcMin/+ × SWR/J or C57BR/cdcJ | Hybrid ApcMin/+ mice survive longer due to decreased adenoma frequency. After one-year high amount of invasive adenocarcinomas. 3% metastasis to lymph nodes |
| 15 | [105] | Change of the ApcMin/+ genetic background from C57Bl6/J to A/J mice | Increased tumor formation in the intestine. 50% adenocarcinomas in the small intestine and 20% in the colon |
| 16 | [131] | AhCre+; Apcflox/flox | β-naphthoflavone-inducible Cyp1A promoter Cre-transgene (AhCre). Rapid death upon induction due to disruption of intestinal architecture |
| 17 | [98] | ApcMin/+ + AOM | 6-fold increase of colonic tumor formation compared to ApcMin/+ mice |
| 18 | [379] | ApcMin/+ + AOM | Increased incidence of colonic adenocarcinomas |
| 19 | [52] | ApcMin/+ + DSS | High incidence of well differentiated colonic carcinomas |
| 20 | [380] | ApcMin/+ + PhIP | 2- to 3-fold increase of tumor formation compared to ApcMin/+ mice |
| 21 | [99] | ApcMin/+ + AOM + DSS | Mainly small intestinal tumor formation |
| 22 | [111] | ApcMin/+P53-/- | No increased adenoma formation or malignancy compared to ApcMin/+ 53-/+ - and ApcMin/+P53+/+ -mice |
| 23 | [112] | ApcMin/+P53-/- | No increased malignancy or adenoma formation compared to ApcMin/+ mice |
| 24 | [381] | ApcMin/+P53-/- | Slight, but not significant, increase in malignancy |
| 25 | [113] | ApcMin/+Mom1R/RP53−/− | P53 deficiency increases intestinal adenoma multiplicity and malignancy |
| ApcMin/+Mom1R/SP53−/− | |||
| 26 | [139] | ApcΔ716Trp53+/LSL•R270HVillin-CreER | Homozygotes die rapidly from lymphoma while heterozygous P53R270H leads to invasive adenocarcinomas with features of EMT |
| ApcΔ716Trp53LSL•R270H/LSL•R270HVillin-CreER | |||
| 27 | [128] | Deletion of Apc and P53 by viral delivery of corresponding sgRNA into Rosa26LSL-Cas9-eGFP/+; VillinCreER | In vivo editing of Apc alone or in combination with P53 via Cre mediated Cas9-expression and provision of sgRNA by viral infection of the colonic epithelium leads to tumor formation without metastatic properties |
| 28 | [382] | Fabpl:Cre+/oTdgflox/-ApcMin/+ | TDG knockout increases adenoma formation, no carcinomas |
| 29 | [122] | AhCre+/T; Kras+/LSLV12 | Cytochrome p450 mediated Cre expression in the liver and intestine induced by β-naphthoflavone (AhCre). KrasV12 mutation does not alter the intestinal epithelium, but combined with APC-loss, accelerates tumorigenesis in the intestine. 17% of the tumors are invasive adenocarcinomas |
| AhCre+/T; Kras+/LSLV12, Apc+/fl | |||
| 30 | [383] | CDX2P9.5-G22Cre; Apcflox/flox; LSL-KrasG12D | Severe debilities in mice with reduced weight and lifespan and anal bulging. Kras mutation does not increase malignancy |
| 31 | [136] | Fapbl-Cre; Apc2lox14/+; KrasLSL-G12D/+ | KrasG12D, but not NrasG12D drives colon cancer progression. Nras indistinct from ApcMin/+ mice |
| Fapbl-Cre; Apc2lox14/+; NrasLSL-G12D/+ | |||
| 32 | [143] | shApc/KrasG12D/P53fl/fl/Lgr5 | Mice with inducible and reversible Apc deletion via short hairpin RNA show duodenal and colonic tumor formation. Additional, conditional mutations drive cancer progression, but upon Apc restoration by withdrawal of doxycycline rapid tumor regression can be induced |
| 33 | [130,384] | ApcCKO/LSL-Kras | Cre-mediated knockout of Apc and KrasG12D activation by surgical application of AdenoCre to the colonic epithelium leads to adenocarcinomas with 20% liver metastases after 20 weeks |
| 34 | [385] | Apc+/580S, Kras+/LSL, CAC+ | Only adenomas |
| 35 | [116] | CMV-cre × LSL- KrasG12D | Germline embryonic expression of an endogenous KrasG12D allele is uniformly lethal. Diffuse colonic hyper- and dysplasia |
| LSL-KrasG12D; Fabpl-Cre | |||
| 36 | [117] | Kras+/V12 × CMV-Cre+/T | High embryonic lethality; adult animals succumb to pulmonary neoplasia, no phenotypic changes in the intestine |
| 37 | [134] | LSL-KrasG12D/Villin-cre +AOM | Increased number of microadenomas in the proximal colon |
| 38 | [198] | Villin-Cre/K-rasG12Dint/Ink4a/Arf−/− | Within 12 wk progression to invasive adenocarcinomas (79%) with 60% lung metastases |
| 39 | [165] | ApcΔ716 Tgfbr2flox/flox; villin-CreER | Disruption of TGFβ-signaling leads to locally invasive adenocarcinomas |
| 40 | [164] | AOM-treatment of Fabpl4xat-132Cre; Tgfbr2flx/flx mice | Higher incidence of colonic adenomas and adenocarcinomas |
| 41 | [167] | Villin-Cre; Apc1638N/wt; Tgfbr2flx/flx | Compared to Apc1638N/wt similar tumor incidence but increased progression to locally invasive adenocarcinoma |
| 42 | [163] | Tgfb1−/−Rag2−/− | Rapid formation of adenomas and adenocarcinomas |
| 43 | [166] | LSL-KrasG12D/wt; Villin-Cre; Tgfbr2E2flx/E2flx | Wnt-independent induction of invasive carcinomas in the intestine with 15% distant metastases |
| 44 | [153] | Villin-Cre; Ptenflx/flx; Tgfbr2flx/flx | Mice with inactivation of TGFβR2 combined with loss of PTEN show high number of mucinous adenocarcinomas throughout the intestine. 8% show distant metastases (not Wnt, but deregulation of CDK inhibitor expression). Pten loss without mutation has no effect |
| 45 | [152] | Villin-CreERT; Apcfl/+; Ptenfl/fl; KrasLSL/+ | Villin-CreERT; Apcfl/+; Ptenfl/fl; KrasLSL/+ mice show rapid morbidity due to invasive small intestinal tumors |
| 46 | [151] | AhCre; Ptenf/f | PTEN is dispensable in the intestinal epithelium, but increases tumorigenesis in the context of APC deficiency |
| 47 | [386] | ApcMin/+Pld1−/− vs ApcMin/+Pld1+/+ +AOM/DSS | Pld1-knockout/suppression leads to decreased tumor burden |
| 48 | [157] | Dpc4+/-: Apc+/Δ716 | Dpc4 and ApcΔ716 cis-compound heterozygote mice show adenoma to carcinoma progression in the small intestine and colon with submucosal infiltration |
| 49 | [159] | Smad2+/-; Apc+/Δ716 | Combination of Apc mutation and loss of Smad2 leads to no changes in tumor size or properties compared to Apc+/Δ716 mice |
| 50 | [161] | ApcMin/+; Smad3−/− | Reduced lifespan of 2 months due to rapid tumor development in the distal colon with mixed histology but no metastases |
| 51 | [156] | Apc+/1638N/Smad4+/E6sad (cis and trans) | Smad4 mutation leads to intestinal tumors without malignant properties. Both mutations lead to high tumor burden in the upper GI (cis>trans); some show invasion of the submucosa |
| 52 | [387] | cis-Apc+/-/Smad4+/- Mmp7−/− | Mmp7 knockout reduces tumor size but does not affect invasiveness |
| 53 | [388] | Smad2+/-; Apc580D/+ (cis) | Larger tumors, higher incidence of malignant phenotype (compared to Apc580D/+mice) |
| 54 | [160] | Smad3-/- (129/Sv genetic background) | Adenocarcinomas of the intestine with penetration of the whole intestinal wall and lymphatic spread. Lower tumor burden in C57/BL6 × 129/Sv Smad3-/- hybrids. Note, that Smad3 mutations occur only in 2% of CRC (Fleming et al[162], 2013) |
| 55 | [179] | Smad4f/f;Catnblox(ex3)/+;Lgr5-CreERT2-IRES-GFP | Mosaic Cre-expression leads to adenoma formation |
| 56 | [178] | Catnb+/lox(ex3): Krt1-19+/creCatnb+/lox(ex3): Tg·Fabplcre | Constitutional Cre-mediated excision of ß-catenin phosphorylation site leads to a plethora of small intestine adenomas |
| 57 | [177] | Villin-creERT2/CatnbloxEx3/WT | Expression of GSK3β-resistant β-catenin leads to substitution of enterocytes by highly proliferative crypt stem cells (rapid death) |
| 58 | [142] | Nicd/Apc+/1638N | NOTCH-signaling does not influence adenoma formation |
| 59 | [141] | Nicd/P53−/− | Villin-CreERT2 tamoxifen-dependent P53 deletion in constitutively active NOTCH-signaling background leads to intestinal tumor formation and metastasis |
| 60 | [158] | Car1CreER/+; Apcfl/fl; KrasLSL–G12D/+; P53KO; Smad4fl/fl | Rapid tumor formation in cecum and proximal colon, but high mortality in triple and quadruple mutants |
| 61 | [192] | Msh2Δ7N/Δ7N /Apc+/1638N. Msh2Δ7N/Δ7N /ApcMin/+ | Rapid tumor formation in the small intestine, early death (2-3 months), more tumors in Msh2Δ7N/Δ7N /ApcMin/+ |
| 62 | [191] | ApcMin/+/Msh2+/+; ApcMin/+/Msh2+/-; ApcMin/+/Msh2-/- | Accelerated tumor formation in the small intestine in MSH2-deficient mice. Mice homozygous for Msh2-/- dye rapidly from lymphomas |
| 63 | [389] | KrasV12/Cre/Msh2−/− | β-naphthoflavone inducible Kras mutation (AhCre+/T, Kras+/LSLV12) combined with homozygous Msh2-knockout leads to increased number of intestinal adenomas. No carcinomas, relevant number of thymic lymphomas |
| 64 | [197] | VCMsh2LoxP/LoxP | Villin-controlled Cre-expression leads to intestinal MMR-deficiency, similar to Lynch syndrome. 50% of tumors in the small intestine are malignant. A high proportion of carcinomas in VCMsh2LoxP/null mice are resistant to cisplatin and FOLFOX |
| VCMsh2LoxP/G674D | |||
| VCMsh2LoxP/null | |||
| 65 | [185,186] | Msh2-/- | Death due to lymphoma |
| 66 | [194] | Apc1638N/+ Exo1 +/− Fen1+/− | Increased tumor multiplicity and incidence, higher progression to malignancy, high incidence of hematopoietic cancers |
| 67 | [193] | Fen1null/Apc1638N | Increased malignancy of intestinal tumors compared to Apc1638N mice through MSI |
| 68 | [184] | Mlh1-/-/Apc1638N | Increased tumor incidence and multiplicity, 30% adenocarcinomas, reduced lifespan of 3.3 mo. High amount of extraintestinal tumors |
| 69 | [187] | Msh6-/+ | Reduced life span in hetero- and homozygotes due to lymphomas and gastrointestinal tumors. Tumors show no signs of MSI |
| Msh6-/- | |||
| 70 | [390] | Msh3−/−; Msh6−/− | Decreased life span, death due to intestinal adenocarcinomas or lymphomas |
| 71 | [190] | Msh6TD/TD; Msh6TD/+ | B or T cell non-Hodgkin lymphomas, adenomas of the small intestine, basal cell carcinomas |
| 72 | [388] | Pms2-/-; Pms1-/- | Pms2-deficient mice develop lymphomas and sarcomas, but no intestinal tumors; Pms1 deficiency does not cause tumor development |
| 73 | [150] | Fc+; Pik3ca*+ (FVB/N-Tg(Fabp1-Cre)1Jig; Gt(ROSA)26Sortm7(Pik3ca*,EGFP)Rsky | Constitutively active PI3K causes mucinous adenocarcinomas of the proximal colon with infiltration of the whole intestinal wall |
| 74 | [129] | Apcfl/fl KrasG12D/+ Pik3cap110*+ Cre-Adenovirus via coloscopic injection | Additional driver mutations do not increase tumor proliferation, but cause progression to adenocarcinoma and metastatic disease |
| 75 | [172] | ApcCKO/CKO; BrafCA/+, AdenoCre delivery via colonoscopy | Cre-mediated Apc-knockout combined with latent BrafV600E cause neoplasia of the distal colon (50% adenocarcinomas) |
| 76 | [174] | Villin-Cre;BrafLSL-V637E/+ | Some invasive adenocarcinomas (13%), dominant negative P53 mutation leads to 60% cancers with 2% metastases. Also, p16ink4a mutation causes carcinomas in a Braf mutational background |
| Villin-Cre;BrafLSL-V637E/+;P53LSL-R172H/+ | |||
| Villin-Cre;BrafLSL-V637E/+;p16Ink4∗ | |||
| 77 | [171] | Braf+/LSL-V600E; AhCreERT+/o x | CypA1-promotor-driven, tamoxifen-inducible Cre-recombinase facilitates BrafV600E expression in the small intestine with consecutive crypt hyperplasia. Repression of p16Ink4A leads to tumor formation in various tissues and decreased survival (6 wk) |
| Cdkn2a (Ink4a/ArfΔEx2,3) = VE;Cdkn2aΔEx2,3/ΔEx2,3 | |||
| 78 | [140] | ApcΔ716 (A), Kras+/LSL-G12D (K), Tgfbr2flox/flox (T), Trp53+/LSL-R270H (P), Fbxw7flox/flox (F), and Villin-CreER | Kras mutation increases multiplicity of tumors, whilst P53 gain-of-function mutation and Tgfβr-knockout leads to invasiveness, no spontaneous metastases |
| 79 | [147] | ApcMin/+; Fbw7ΔG | Reduced survival for Fbw7 deficient mice, also in heterozygous setting |
| 80 | [148] | Fbw7flox/flox; P53flox/flox; Villin-Cre | Aggressive carcinomas with metastatic spread to lymph nodes and liver |
| 81 | [391] | Mutyh-/- | Spontaneous adenoma and adenocarcinoma development in the intestine; predominantly in the upper small intestine. Tumorigenesis increased by oxidative stress (KBrO3) |
In summary, GEMM have contributed enormously to the understanding of the molecular processes of CRC initiation, progression and crosstalk of common cancer-associated pathways. Besides the models for spontaneous CRC and common cancer syndromes, like Familiar Adenomatius Polyposis and LS, several models recapitulate metastatic disease, either as “classic” GEMM[141,148,166,198] or upon viral Cre delivery[129,130]. Yet, these models have several limitations. First of all, cancer development is a stepwise process with an initial driver mutation and subsequent acquisition of further mutations[199], and thus can only be partly reflected in tumor mouse models by the combination of a constitutively active with an inducible mutation[172]. Roper et al[128] recently demonstrated in vivo genome editing of Apc and P53 by viral delivery of the correspondent sgRNA in mice expressing CRISPR-Cas9 under the control of a Villin-Cre transgene. Second, the number of combined mutations is limited in the mouse, since the resulting phenotype shows often a drastically reduced lifespan[152]. Triple mutant (Car1CreER/+; Apcfl/fl; KrasLSL–G12D/+) and quadruple mutant mice (Car1CreER/+; Apcfl/fl; KrasLSL–G12D/+; P53KO; Smad4fl/fl) showed a reduced lifespan of merely one month. Moreover, GEMM are time consuming and expensive, since breeding of the transgenic mice often takes multiple generations and requires careful interbreeding to yield the desired alterations. In terms of animal welfare, it should be noted that the breeding process yields many “reject” mice, which are neither used for further breeding nor for research. Also, the construct of the transgene, or the viral vector, respectively, is complicated. While GEMM represent a valuable tool for basic research, their use for preclinical studies is limited due to a lack of genetic heterogeneity on the one hand, and discrepancies to the human tumor development on the other hand. On a final note, it should be added, that GEMM of CRC can be applied the other way round: Mice harboring mutagenic SB transposons were crossed to mice expressing SB transposase under control of a Villin-Cre-transgene, to generate mice, that develop intestinal lesions due to random insertional mutagenesis and can be screened for unknown CRC driver mutations[200]. Moreover, by combining this approach with well-known driver mutations, new pathway-associated mutations could be identified[201,202].
Transplant mouse models can be classified in various ways: Syngeneic tumor transplantation is characterized by tumor tissue or cancer cell line engraftment within the same mouse strain; whereas xenogeneic grafts are derived from a different mouse strain or human donors. Additionally, it can be distinguished between heterotopic and orthotopic models. As cancer grafts, tumor cells, organoids and tumor tissue pieces can be employed. In 1876, Novinsky successfully transferred tumors (likely canine venereal sarcomas) from one dog to another in two independent trials[203]. Shortly thereafter, Hanau[204] and Morau (reviewed in[205]) reported independently the successful passaging of epithelial rodent tumors. Around the turn of the century, several transplantable rodent tumors, mostly of a sarcomatoid phenotype, were established[206]. Later, the discovery of the human leukocyte antigens and oncogenic viruses elucidated the results of the earlier transplantation studies[207,208]. Toolan pioneered in the xenograft field by attenuating graft rejection through X-radiation and cortisone treatment[209,210].
A fundamental prerequisite for the successful engraftment of xenogeneic tissue in mice is the impairment of the host immune system. A detailed explanation of the development and sophistication of immunocompromised mice would fill several pages and is exquisitely reviewed elsewhere[211]. In short, with the discovery of “nude” mice (recessive mutation of FOXN1 leading to hairlessness and athymia)[212] and the subsequent breeding of NMRInu/nu mice, xenotransplantation was possible for the first time without additional immunoablative treatment[213]. A more immunodeficient animal strain, C:B:-17 scid, carrying a homozygous mutation of the Prkdc gene resulting in a lack of functional B and T lymphocytes, was established by Bosma et al[214] in 1983. To overcome NK cell function, SCID mice were crossed with non-obese diabetic mice (NOD)[215] by several workgroups generating NOD/LtSz‐scid[216], NOD/LtSz-scid β2mnull[217] and NOD/Shi-SCID mice[218]. However, the life span of NOD/SCID mice is limited by the development of thymic lymphomas[219] and they show relevant “immune leakiness” caused by spontaneous rearrangement of T and B cell receptors[220,221]. Lastly, to abolish NK cell activity completely, deficiency of the IL-2 receptor subunit gamma (IL2Rγ) and the Janus kinase 3 (Jak3) were introduced to NOD/SCID mice generating the commonly used strains NOG (NOD/SCID/ IL2Rγtm1Sug)[222], NSG (NOD/SCID/IL2Rγtm1Wjl)[223] and NOJ (NOD/SCID/Jak3null)[224]. Since the DNA-dependent protein kinase catalytic subunit, encoded by the Prkdc gene, is also responsible for DNA repair, SCID mice are very sensitive for radiation and DNA-damaging agents. Therefore, Shultz et al[225] developed the more robust, but equal immunodeficient NOD/LtSz-Rag1nullPfpnull strain. Since then, many more immunodeficient strains, with in part different genetic backgrounds, have been developed[211,226]. In general, it can be noted, that the more severe immunodeficient the host, the higher are the engraftment rates. Nevertheless the NMRInu/nu strain is still of high relevance for xenografting: The strain is less prone to opportunistic infections[227], more tolerant for chemotherapeutic agents and shows reasonable engraftment rates for primary patient-derived xenografts (PDX) and good engraftment rates for subsequent mouse to mouse passaging[228,229]. An economical plus is that this mouse strain is the least expensive immunodeficient one. It is mandatory to house immunodeficient mice in a specific pathogen free environment, using sterile techniques and microisolator caging. For syngeneic mouse models, viz. transplantation of cell or organoids from mice, exact strain conformity of donor and recipient mouse must be guaranteed, since even closely related substrains can differ genetically[230].
The advantages of s.c. tumor engraftments are glaring: They require nominal surgical skills, allow high throughput of samples due to time efficacy and tumor growth can be monitored by the naked eye. Early s.c. models of solid tumors were mostly carried out by injection of a tumor cell suspension into the mouse flank. Although some of these models correctly predicted clinical response for specific cancer entities and therapeutics[231] large drug screens revealed that these models are of rather modest value for the prediction of clinical response in humans[232-235]. Moreover, the resulting tumors from a homogenous cell suspension do not reflect the intratumor-heterogeneity and an adequate tumor microenvironment is also absent[236]. Especially established CRC cell lines show low genetic diversity due to high passage and selective pressure[237]. On a site note, one of the most cited CRC cell lines, HCT116, was established almost 40 years ago; enough time for mislabeling, cross-contaminations and high passage selection[238,239]. While tumor cell lines in general remain a cornerstone of cancer research[240,241], their heterotopic in vivo application creates no scientific added value. The creation of a s.c. tumor graft as intermediate step for subsequent orthotopic transplantation can be considered as an exception. Even though these cell-derived grafts are frequently referred to as PDX in the literature, we believe that this term should be avoided and “cell line-derived xenograft - CDX” is more reasonable. The implantation of tumor cells or tumor pieces under the renal capsule follows the rational that the high vascularized environment propagates better engraftment[242,243] and was historically used for the subrenal capsule assay[244]. While this model might be advantageous for some cancers[245], we see no advantage for CRC engraftment over the s.c. PDX model, a fortiori comparing practical effort, monitoring of tumor growth and animal welfare. Intravenous injection of cell suspension is often used to simulate hematogenous dissemination of tumor cells[246,247], but circumvents crucial steps of metastasis, namely degradation of the surrounding tissue and lymphatic and/or vascular invasion[248]. Thus, the same applies to the splenic injection of tumor cells to generate liver metastasis[249,250] or the intraperitoneal injection to simulate peritoneal carcinosis[251].
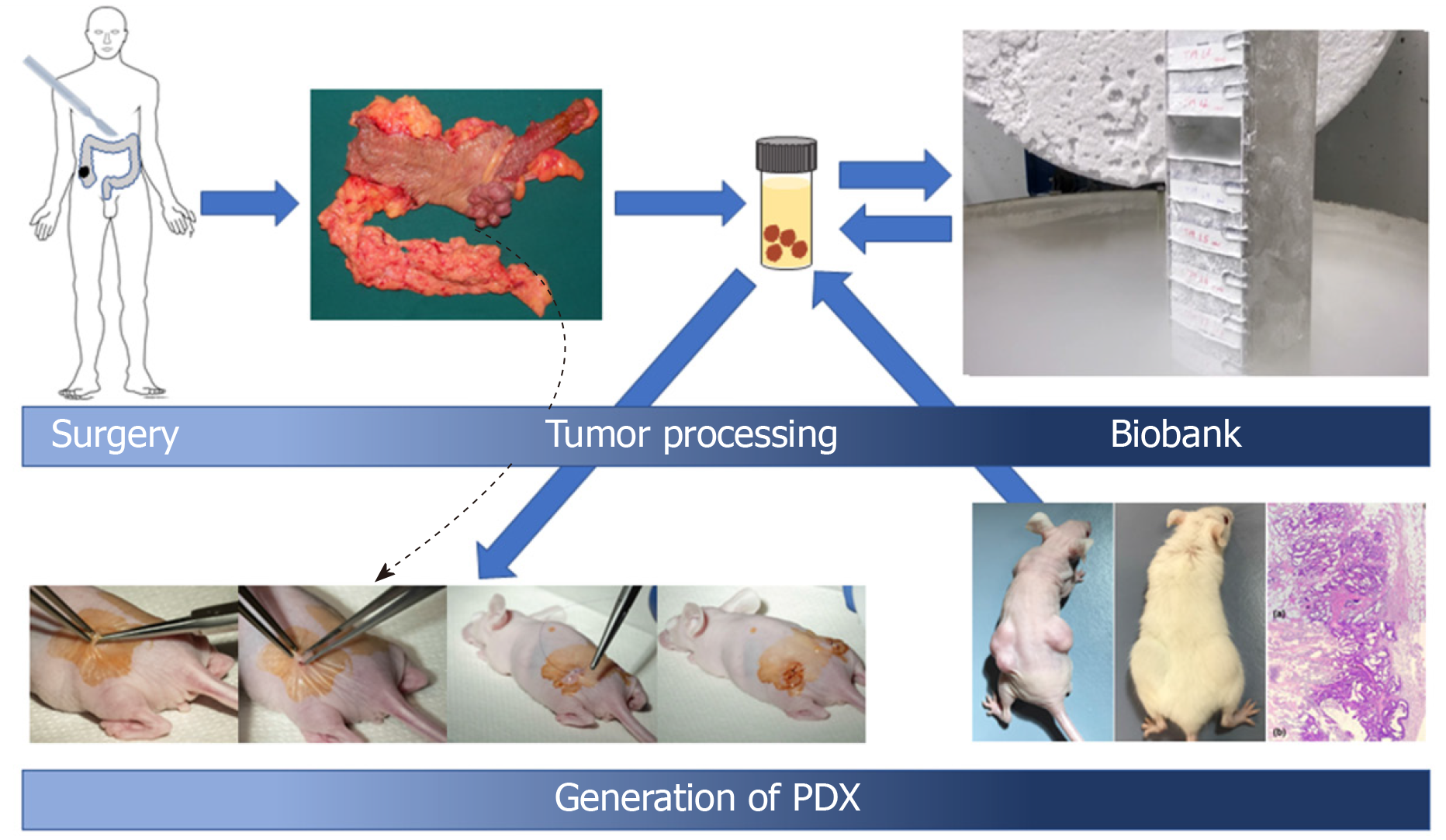
PDX differ greatly from the aforementioned heterotopic tumor models. They are established by the s.c. implantation of a tumor piece from a surgical resection or biopsy into the flanks of immunocompromised mice; with lower tumor take rates for biopsy samples[237]. Tissue can either be implanted directly after resection or cryopreserved in fetal calf serum containing 10% DMSO for implantation at a later time[229]. Incubation of the tissue in Matrigel® prior to tumor implantation, significantly increases engraftment rates[228]. In order to obtain sufficient tumor tissue for larger scale studies, the resulting tumor can be fragmented and re-grafted subsequently. In recent years, our workgroup focused on the build-up of a large CRC biobank consisting of more than 140 PDX-models (general procedure is presented in Figure 2). This PDX panel reflects adequately the clinical and molecular heterogeneity of the patient population undergoing surgical resection of primary or metastatic CRC[252]. It is well accepted that PDX closely recapitulate the histology of the original “donor” tumor over several passages[253-255] and are also genetically stable[256,257]. However, Ben-David et al[258] demonstrated recently that changes in copy number alterations occurred in early passages of PDX tumors compared with both the P0 PDX and the donor tumor. A common criticism in heterotopic mouse models is related to the absence of tumor-stroma interaction or the “tumor microenvironment”[259]. While this is true for immune cells, the stromal component remains intact in PDX[255]. Although the human stromal compounds (fibroblasts, blood vessels etc.) are quickly and steadily replaced by their murine counterparts, the overall architecture of the tumor remains unaffected in the majority of cases[260,261]. Moreover, these murine stroma cells adopt and maintain a human-like metabolic phenotype[262]. These features indicate that PDX are indeed good and valuable models for preclinical testing of conventional and novel anticancer agents in the era of personalized cancer therapy[263,264]. A proof of concept study with advanced refractory cancers demonstrated that drug responses measured in a PDX model, can be used for successful clinical decision making[265]. A PDX model of CRC metastases closely resembled the efficacy of cetuximab and identified druggable targets in resistant tumors[266]. Moreover, a PDX clinical trial approach (one animal per model per treatment) reflects well the heterogeneity of the patient population and allows testing of new drugs and combinatorial regimen[267]. A large study with over 1000 PDX models confirmed the consistency between clinical and PDX clinical trial drug response[268]. The ultimate goal of precision medicine would comprise of the profound genetic and functional characterization of a given tumor to identify relevant drug targets and subsequent validation of potential therapies with aid of a PDX bearing “avatar” mouse to provide the most efficient treatment for the individual patient[264,269]. Currently, several clinical trials following this approach for colorectal[270,271] and pancreatic cancer are recruiting[272]. Yet, a median duration of 12.2 mo until PDX model establishment[237] remains an unsolved issue for patients urgently in need for treatment. When it comes to drug testing, it should be considered, that immunotherapy approaches can only be restrictedly evaluated in immunodeficient host mice. A further disadvantage of PDX models is a potential selection for more aggressive tumors. The data concerning the association between successful PDX engraftment and clinical or molecular features is in part conflicting. While we and others could not find significant associations between tumor grading and PDX engraftment[237,252], a Korean study observed significant correlations with tumor staging and grading[273]. A smaller study with a high PDX establishment rate found a significant correlation of PDX success with positive nodal status and grading[274], while Julien et al[275] only found significances for the combination of a positive nodal status with an elevated carcinoembryonic antigen level. Moreover, we observed a significant correlation between PDX engraftment and molecular features like KRAS and BRAF mutations as well as MSI[252]. Apart from the tumor biology, choice of the host mouse strain, repeated attempts of engraftment, quantity and quality of the resected tissue as well as previous treatment of the patient are additional factors influencing the success of model establishment. Collins et al[276] recently reported PDX engraftment rates varying from 14 to 100% with a median PDX establishment rate of 68% reviewing 14 CRC-PDX studies. Compared to establishment rates for primary CRC cell lines of about 10%, the PDX is clearly superior[252,277]. A selection bias relating to cancer biology can be diminished by increasing the number of enrolled patients and molecular characterization of the individual PDX. In fact, a very recent PDX study found an underrepresentation of the consensus molecular subtype number 2, due to worse engraftment[278]. Another crucial pitfall of the PDX model is the development of EBV-associated lymphomas at the implantation site, which can mimic successful engraftment[279]. Depending on the mouse strain and cancer entity, between 2.3% (colorectal) and 75% (prostate cancer) of primary engrafted bona fide xenografts turn out to be human de-novo lymphomas[280-284]. Since this condition is more frequently reported in NSG and comparable strains, development of de-novo lymphoma in NMRInu/nu mice might be hindered by high NK cell activity[285]. Thus, after successful engraftment of a PDX in NSG mice, we conduct the subsequent passaging in NMRInu/nu mice and xenograft histology is frequently evaluated by an experienced pathologist. Interestingly, Butler et al[286] significantly reduced the frequency of lymphomas in an ovaria cancer PDX model by a unique dosage of rituximab during implantation. Additionally, PDX serve not only in the field of therapy development; they are also a vital tool for the maintenance of a healthy biobank, allowing the establishment of secondary cell lines and supply sufficient tumor samples for the exchange with other work groups[252].
In summary, we consider the PDX model as keystone of cancer research, holding great potential in the developing field of precision medicine for CRC.
Orthotopic CRC models are implemented to overcome the drawbacks of heterotopic models, videlicet lack of an adequate tumor microenvironment and metastatic behavior.
At the beginning of the 1980s, the first orthotopic engraftments of CRC cell lines was reported by Snipes[287], demonstrating the feasibility of an intramural cell injection causing locally invasive cancer growth. A few years later, Bresalier et al[288] demonstrated that the orthotopic injection of human CRC cells causes metastases in the liver. In 1991, Fu et al[289] successfully engrafted 13 patient-derived tumors by removing the serosa and sewing the tumor pieces to the cecal wall. Beside the local tumor outgrowth, lymph node and liver metastases were reported for a few mice. Since the murine cecum is relatively large compared to its human counterpart and readily accessible by laparotomy, it rapidly became the favored site for orthotopical engraftment by different approaches. Many authors generated a s.c. cell graft in a donor mouse, of which a small piece was sewed to the cecum after damaging the serosa[290-292]. Several varieties of this technique can be found in the literature: While some authors removed the mucosa and sewed the tumor pieces onto the cecal wall[293,294], others formed a subserosal tunnel for tumor inoculation, which was afterwards closed by a suture[295] or surrounded the tumor piece with a “pouch” formed by a serosal duplicature[296]. Others reported the technically more challenging subserosal injection of a cell suspension into the cecal wall[297]. The cell injection method is often referred to as subserosal[298], while other work groups describe a submucosal injection[299]; both frequently with Matrigel® addition to the cell suspension to avoid cell spillage[300]. Considering the gauntness of the cecal wall, we will here refer to both techniques as “intracecal” injection. The possibility of a “preconditioning” via s.c. PDX has also been described for the cell injection approach[301]. Beside the cecum, other colonic sites like the descending colon can be accessed for cell injection[302,303]. Despite frequent metastases, some aspects of these techniques may be viewed critically. First, given the fact that CRC arise from the mucosa, these models cannot be considered as genuine orthotopic and also the injection approach might mimic an advanced CRC. Second, they allow the contact of cancerous tissue with the abdominal cavity, hence it cannot be ruled out that some of the metastases are the result of intraabdominal cell spillage. Moreover, these approaches require the opening of the abdomen and can cause inflammation and morbidity. Nevertheless, the cecal orthotopic model is frequently applied, especially for basic research to identify the underlying mechanisms of metastatic progression, since it can render metastatic, end stage disease within a few weeks[304]. The upregulation of genes associated with advanced CRC, could also be observed in liver metastasis from an orthotopic model[290,305]. The orthotopic approach allows to elucidate the role of certain molecular pathways by direct comparison of the metastatic properties of a given cell with their genetically engineered counterpart[306-310]. The additional transfection of these cells with a reporter, like GFP, DsRed or luciferase, allows monitoring of tumor progress by in vivo imaging[311-313]. The orthotopic approach can be used in transgenic mice to clarify the role of distinct molecules[314] or certain cell types[315]. To further stress the functionality of stromal components, a co-injection of tumor cells and stromal cells is feasible[316-318]. By using NSG mice, the efficiency of an immune cell-based therapy can be tested in the context of such an orthotopic model[319]. Furthermore, circulating tumor cells (CTC) can be isolated from murine blood[320]. In addition to the above discussed surgical approaches, there are less invasive concepts that do not require surgery and diminish the risk of intraabdominal cell spillage. Kashtan et al[321] demonstrated the successful engraftment of murine tumor cells by submucosal injection in the distal rectum in 1992 and this approach was adapted by several work groups[322-324]. To reach more proximal parts of the rectum or the descending colon, submucosal cell application can be performed via small endoscopic instruments[325,326]. Depending on the cell line, liver metastases have been observed[327]. Lastly, tumor cells can be inoculated in the colon mucosa by the acid enema approach described by Kishimoto et al[328]; a true orthotopic model with intramucosal tumor development and liver metastases. In brief, the mucosa is damaged by 4% acetic acid enema and after neutralization with PBS, a tumor cell suspension is instilled and the anus temporaryly sealed. Hite et al[329] subjected all three orthotopic models (intracecal injection, transanal submucosal injection and acid enema) to a direct comparison. They found the submucosal injection to be the most efficient in tumor formation and metastatic behavior and at the same time well tolerated by the animals. In contrast, the acid enema approach showed the lowest tumor formation frequency but a considerable mortality of 15%. Enquist et al[312] pursued a different concept by sewing a tumor piece directly to the mucosa by creating an artificial rectal prolapse. They were able to engraft pieces from transgenic ApcMin/+;KrasLSLG12D/+;Villin-Cre adenomas in the colon of syngeneic animals and a small subset of these tumors progressed to carcinomas. More strikingly, they managed also to transfer s.c. human PDX to the colons of NSG mice reflecting stage-dependent biological behavior as lymph node metastases could be observed for stage III PDX[312].
Today, orthotopic models are copiously used for the in vivo validation of new therapeutic compounds and as a proof-of-principle approach[330-333]. However, their clinical relevance is limited by the common use of similar, poorly differentiated cell lines. The orthotopic PDX model is promising, but its tumor take rate is not higher as in the s.c. PDX model. A very recently published, “crossover” concept comprising the s.c. engraftment of a PDX, followed by enzymatic disintegration of the PDX to a cell suspension and subsequent orthotopic injection into the rectal submucosa yielded an engraftment rate of 70% for s.c. PDX and 46% for the orthotopic model. Moreover, a metastatic spread was observed for 60% of the tumors successfully engrafted orthotopically[334].
The increasing field of precision medicine has a growing need for highly translational cancer models. Conversely, the increasingly negative public perception of animal studies constrains the scientific community to further stress the 3R-principle (replacement, reduction and refinement) in cancer research[335]. Aside from the improvement of in vivo models, this implies the refinement of in vitro methods as well.
Humanized mice are severely immunocompromised mice, which can be reconstituted with various types of human bone marrow-derived cells or CD34+ hematopoietic stem cells[336,337]. Since human stem and progenitor cells can be attained from umbilical cord blood or from peripheral drawn blood samples after GM-CSF treatment and cultured in vitro[338], these cells can be transferred to sub-lethally irradiated NSG mice. Morton et al[339] observed that PDX of head and neck cancer engrafted into these, so called “Xact mice”, are infiltrated with human B and T lymphocytes. Many transgenic mice further support engraftment with CD34+ stem cells by overexpression of human interleukins and signaling molecules. Thus NBSGW[340], hIL2-NOG[341], NSG-SGM3[342] and SRG-15 mice[343] have been introduced recently and antitumor effects against PDX of different cancers could be observed[341,343]. These models hold great promise for the research of CRC immunotherapy, especially for highly immunogenic hypermutated CRC. Capasso et al[344] showed very recently that check point inhibition with nivolumab leads to growth inhibition of human MSI-H PDX thereby accurately reflecting the clinical response of this CRC subtype. In contrast, no sustainable growth inhibition was observed in MSS tumors or MSI-H tumors in “standard” NSG mice[344,345].
Although patient-derived cell cultures are a valuable tool for high-throughput drug screenings, they exhibit considerable shortcomings[346]. First, the establishment rate of primary patient-derived CRC cells with conventional 2D culturing methods approximates some 10%[252,275], although higher success rates of 40% and more can be found in the literature[347,348]. Second, conventional 2D cultures change the biological properties of cells, possibly altering drug response in vitro[349]. Cell polarization, lack of stroma and abundance of growth factors, nutrients and oxygen are factors that might change the behavior of tumor cells[350]. In recent years, more complex cell culturing methods have emerged. CRC cells, cultured in an extracellular matrix form three dimensional spheres, so called spheroids, that differ in their biological properties from 2D cultured cells[351]. In contrast, organoids are three dimensional structures, derived from intact tumor pieces or tumor stem cells cultured in an extracellular matrix scaffold[352]. Patient-derived organoids (PDO), quite similar to PDX, recapitulate closely the histological and genetic properties of their parental tumors. Moreover, high rates of successful establishment have been reported[353] and reliable drug response prediction seems possible[354-356]. PDOs can be implanted s.c. or orthotopically into mice, resulting in PDO xenografts (PDOX)[264,354,357]. Furthermore, the Clevers group pioneered in the inauguration of non-malignant intestinal organoids exploiting the stem cell niche in vitro[358]. These organoids can be modified in vitro to exhibit malignant properties and used to enlighten the role of cancer-driving pathways by in vivo engraftment[359,360]. The available data strongly suggests, that PDOs reflect more faithfully the biological virtue and drug response of the parental tumor compared to conventional 2D cell cultures[352]. The circumstance, that organoids can be derived from CTC, could render them an excellent tool for the preclinical testing of patients with advanced stage cancer that do not undergo surgery[361]. Additionally, CTC reflect genetic changes associated with acquired drug resistance during chemotherapy[362]. Further steps to a reduction of animal experiments imply the faithful remodeling of the host organism in vitro. Several research groups created a “cancer on a chip” model that combines the advances of 3D cell culture connected with artificial organs that resemble the most common organs of metastatic spread[363]. Miller and Shuler introduced a “body on a chip model” with 14 artificial organs, which could be modified for cancer research[364]. At last, the widely acknowledged work of Guinney et al[365] regarding the consensus molecular subtypes of CRC draw great attention to the value of computed models in cancer science and the capabilities of bioinformatic research. Retrospective analysis of clinical trial samples partly demonstrated the association of drug response with molecular subtypes[366]. The constantly growing knowledge of cancer pathways and their crosstalk on the one hand, and the increased inter-individual complexity of tumors on the other hand, call for a method to integrate and interpret the overwhelming amount of data[367]. In silico methods, like data mining, pattern recognition, machine learning and network approaches, are able to predict the behavior of “virtual” HCT116 cells[368], can reveal genetic patterns associated with survival[369], can be used to detect new biomarkers[370], allow the identification of unknown driver mutations[371] and potential preclinical compounds[372]. Yet, in silico models often lack explanatory power and need careful interpretation by bioinformaticians. Their ability to correctly predict treatment response for an individual patient to a new compound is still a long way off[373].
We kindly thank Jenny Burmeister, graphical assistant, for the supply with excellent pictures.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and Hepatology
Country of origin: Germany
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li Y, Lin JM, Huang ZH S-Editor: Dou Y L-Editor: A E-Editor: Ma YJ
| 1. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13300] [Cited by in RCA: 15471] [Article Influence: 2578.5] [Reference Citation Analysis (2)] |
| 2. | Ferlay J, Colombet M, Soerjomataram I, Dyba T, Randi G, Bettio M, Gavin A, Visser O, Bray F. Cancer incidence and mortality patterns in Europe: Estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer. 2018;103:356-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1625] [Cited by in RCA: 1660] [Article Influence: 237.1] [Reference Citation Analysis (0)] |
| 3. | Mengual-Ballester M, Pellicer-Franco E, Valero-Navarro G, Soria-Aledo V, García-Marín JA, Aguayo-Albasini JL. Increased survival and decreased recurrence in colorectal cancer patients diagnosed in a screening programme. Cancer Epidemiol. 2016;43:70-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Hübner J, Lewin P, Pritzkuleit R, Eisemann N, Maier W, Katalinic A. Colorectal cancer screening by colonoscopy and trends in disease-specific mortality: a population-based ecological study of 358 German districts. Int J Colorectal Dis. 2019;34:599-605. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Kawabata-Shoda E, Charvat H, Ikeda A, Inoue M, Sawada N, Iwasaki M, Sasazuki S, Shimazu T, Yamaji T, Kimura H, Masuda S, Tsugane S. Trends in cancer prognosis in a population-based cohort survey: can recent advances in cancer therapy affect the prognosis? Cancer Epidemiol. 2015;39:97-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Johnson CM, Wei C, Ensor JE, Smolenski DJ, Amos CI, Levin B, Berry DA. Meta-analyses of colorectal cancer risk factors. Cancer Causes Control. 2013;24:1207-1222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 399] [Cited by in RCA: 523] [Article Influence: 43.6] [Reference Citation Analysis (0)] |
| 7. | Waluga M, Zorniak M, Fichna J, Kukla M, Hartleb M. Pharmacological and dietary factors in prevention of colorectal cancer. J Physiol Pharmacol. 2018;69. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 8. | Cole BF, Logan RF, Halabi S, Benamouzig R, Sandler RS, Grainge MJ, Chaussade S, Baron JA. Aspirin for the chemoprevention of colorectal adenomas: meta-analysis of the randomized trials. J Natl Cancer Inst. 2009;101:256-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 358] [Article Influence: 22.4] [Reference Citation Analysis (0)] |
| 9. | Jasperson KW, Tuohy TM, Neklason DW, Burt RW. Hereditary and familial colon cancer. Gastroenterology. 2010;138:2044-2058. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 945] [Cited by in RCA: 857] [Article Influence: 57.1] [Reference Citation Analysis (0)] |
| 10. | Bodmer WF, Bailey CJ, Bodmer J, Bussey HJ, Ellis A, Gorman P, Lucibello FC, Murday VA, Rider SH, Scambler P. Localization of the gene for familial adenomatous polyposis on chromosome 5. Nature. 1987;328:614-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 981] [Cited by in RCA: 877] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 11. | Peltomäki P, Aaltonen LA, Sistonen P, Pylkkänen L, Mecklin JP, Järvinen H, Green JS, Jass JR, Weber JL, Leach FS. Genetic mapping of a locus predisposing to human colorectal cancer. Science. 1993;260:810-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 599] [Cited by in RCA: 536] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 12. | Lindblom A, Tannergård P, Werelius B, Nordenskjöld M. Genetic mapping of a second locus predisposing to hereditary non-polyposis colon cancer. Nat Genet. 1993;5:279-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 289] [Cited by in RCA: 269] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 13. | Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature. 2012;487:330-337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6773] [Cited by in RCA: 6673] [Article Influence: 513.3] [Reference Citation Analysis (0)] |
| 14. | Yamagiwa K, Ichikawa K. Experimental study of the pathogenesis of carcinoma. CA Cancer J Clin. 1977;27:174-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Lorenz E, Steward HL. Intestinal Carcinoma and Other Lesions in Mice Following Oral Administration of 1,2,5,6-Dibenzanthracene and 20-Methylcholanthrene. J Natl Cancer Inst. 1940;1:17-41. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 16. | Druckrey H, Küpfmüller K. Quantitative Analyse der Krebsentstehung. Zeitschrift für Naturforschung B. 1948;3:254–266. [RCA] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 131] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 17. | Lisco H, Finkel MP, Brues AM. Carcinogenic properties of radioactive fission products and of plutonium. Radiology. 1947;49:361-363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Laqueur GL. Carcinogenic Effects of Cycad Meal and Cycasin, Methylazoxymethanol Glycoside, in Rats and Effects of Cycasin in Germfree Rats. Fed Proc. 1964;23:1386-1388. [PubMed] |
| 19. | Morgan RW, Hoffmann GR. Cycasin and its mutagenic metabolites. Mutat Res. 1983;114:19-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 19] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 20. | Druckrey H, Preussmann R, Ivanković S, Schmidt CH, So BT, Thomas C. [Carcinogenic effect of azoethane and azoxyethane on rats]. Z Krebsforsch. 1965;67:31-45. [PubMed] |
| 21. | Rosenberg DW, Giardina C, Tanaka T. Mouse models for the study of colon carcinogenesis. Carcinogenesis. 2009;30:183-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 297] [Article Influence: 17.5] [Reference Citation Analysis (0)] |
| 22. | Fiala ES, Stathopoulos C. Metabolism of methylazoxymethanol acetate in the F344 rat and strain-2 guinea pig and its inhibition by pyrazole and disulfiram. J Cancer Res Clin Oncol. 1984;108:129-134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Suzuki R, Kohno H, Sugie S, Nakagama H, Tanaka T. Strain differences in the susceptibility to azoxymethane and dextran sodium sulfate-induced colon carcinogenesis in mice. Carcinogenesis. 2006;27:162-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 176] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 24. | Turusov VS, Lanko NS, Krutovskikh VA, Parfenov YD. Strain differences in susceptibility of female mice to 1,2-dimethylhydrazine. Carcinogenesis. 1982;3:603-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Izumi K, Otsuka H, Furuya K, Akagi A. Carcinogenicity of 1,2-dimethylhydrazine dihydrochloride in BALB/c mice. Influence of the route of administration and dosage. Virchows Arch A Pathol Anat Histol. 1979;384:263-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 26. | Sohn OS, Fiala ES, Requeijo SP, Weisburger JH, Gonzalez FJ. Differential effects of CYP2E1 status on the metabolic activation of the colon carcinogens azoxymethane and methylazoxymethanol. Cancer Res. 2001;61:8435-8440. [PubMed] |
| 27. | Narisawa T, Wong CQ, Maronpot RR, Weisburger JH. Large bowel carcinogenesis in mice and rats by several intrarectal doses of methylnitrosourea and negative effect of nitrite plus methylurea. Cancer Res. 1976;36:505-510. [PubMed] |
| 28. | Reddy BS, Ohmori T. Effect of intestinal microflora and dietary fat on 3,2'-dimethyl-4-aminobiphenyl-induced colon carcinogenesis in F344 rats. Cancer Res. 1981;41:1363-1367. [PubMed] |
| 29. | Sugimura T, Terada M. Experimental chemical carcinogenesis in the stomach and colon. Jpn J Clin Oncol. 1998;28:163-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 30. | Bouvard V, Loomis D, Guyton KZ, Grosse Y, Ghissassi FE, Benbrahim-Tallaa L, Guha N, Mattock H, Straif K; International Agency for Research on Cancer Monograph Working Group. Carcinogenicity of consumption of red and processed meat. Lancet Oncol. 2015;16:1599-1600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1181] [Cited by in RCA: 1085] [Article Influence: 108.5] [Reference Citation Analysis (0)] |
| 31. | Jägerstad M, Skog K. Genotoxicity of heat-processed foods. Mutat Res. 2005;574:156-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 181] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 32. | Turesky RJ. Formation and biochemistry of carcinogenic heterocyclic aromatic amines in cooked meats. Toxicol Lett. 2007;168:219-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 132] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 33. | Cheung C, Ma X, Krausz KW, Kimura S, Feigenbaum L, Dalton TP, Nebert DW, Idle JR, Gonzalez FJ. Differential metabolism of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) in mice humanized for CYP1A1 and CYP1A2. Chem Res Toxicol. 2005;18:1471-1478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 80] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 34. | Kaderlik KR, Mulder GJ, Shaddock JG, Casciano DA, Teitel CH, Kadlubar FF. Effect of glutathione depletion and inhibition of glucuronidation and sulfation on 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) metabolism, PhIP-DNA adduct formation and unscheduled DNA synthesis in primary rat hepatocytes. Carcinogenesis. 1994;15:1711-1716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 41] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 35. | Alexander J, Wallin H, Rossland OJ, Solberg KE, Holme JA, Becher G, Andersson R, Grivas S. Formation of a glutathione conjugate and a semistable transportable glucuronide conjugate of N2-oxidized species of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) in rat liver. Carcinogenesis. 1991;12:2239-2245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 51] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 36. | Malfatti MA, Kulp KS, Knize MG, Davis C, Massengill JP, Williams S, Nowell S, MacLeod S, Dingley KH, Turteltaub KW, Lang NP, Felton JS. The identification of [2-(14)C]2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine metabolites in humans. Carcinogenesis. 1999;20:705-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 73] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Zhang J, Lacroix C, Wortmann E, Ruscheweyh HJ, Sunagawa S, Sturla SJ, Schwab C. Gut microbial beta-glucuronidase and glycerol/diol dehydratase activity contribute to dietary heterocyclic amine biotransformation. BMC Microbiol. 2019;19:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 38. | Frandsen H. Biomonitoring of urinary metabolites of 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP) following human consumption of cooked chicken. Food Chem Toxicol. 2008;46:3200-3205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 39. | Nakagama H, Ochiai M, Ubagai T, Tajima R, Fujiwara K, Sugimura T, Nagao M. A rat colon cancer model induced by 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine, PhIP. Mutat Res. 2002;506-507:137-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 40. | Chen JX, Wang H, Liu A, Zhang L, Reuhl K, Yang CS. From the Cover: PhIP/DSS-Induced Colon Carcinogenesis in CYP1A-Humanized Mice and the Possible Role of Lgr5+ Stem Cells. Toxicol Sci. 2017;155:224-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 41. | Sugimura T, Wakabayashi K, Nakagama H, Nagao M. Heterocyclic amines: Mutagens/carcinogens produced during cooking of meat and fish. Cancer Sci. 2004;95:290-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 513] [Cited by in RCA: 459] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 42. | Huderson AC, Myers JN, Niaz MS, Washington MK, Ramesh A. Chemoprevention of benzo(a)pyrene-induced colon polyps in ApcMin mice by resveratrol. J Nutr Biochem. 2013;24:713-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 43. | Diggs DL, Harris KL, Rekhadevi PV, Ramesh A. Tumor microsomal metabolism of the food toxicant, benzo(a)pyrene, in ApcMin mouse model of colon cancer. Tumour Biol. 2012;33:1255-1260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 44. | Okayasu I, Hatakeyama S, Yamada M, Ohkusa T, Inagaki Y, Nakaya R. A novel method in the induction of reliable experimental acute and chronic ulcerative colitis in mice. Gastroenterology. 1990;98:694-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1733] [Cited by in RCA: 1823] [Article Influence: 52.1] [Reference Citation Analysis (8)] |
| 45. | Kawada M, Arihiro A, Mizoguchi E. Insights from advances in research of chemically induced experimental models of human inflammatory bowel disease. World J Gastroenterol. 2007;13:5581-5593. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 128] [Cited by in RCA: 141] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 46. | Eichele DD, Kharbanda KK. Dextran sodium sulfate colitis murine model: An indispensable tool for advancing our understanding of inflammatory bowel diseases pathogenesis. World J Gastroenterol. 2017;23:6016-6029. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 621] [Cited by in RCA: 581] [Article Influence: 72.6] [Reference Citation Analysis (15)] |
| 47. | Munyaka PM, Rabbi MF, Khafipour E, Ghia JE. Acute dextran sulfate sodium (DSS)-induced colitis promotes gut microbial dysbiosis in mice. J Basic Microbiol. 2016;56:986-998. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 191] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 48. | He X, Wei Z, Wang J, Kou J, Liu W, Fu Y, Yang Z. Alpinetin attenuates inflammatory responses by suppressing TLR4 and NLRP3 signaling pathways in DSS-induced acute colitis. Sci Rep. 2016;6:28370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 124] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 49. | Dieleman LA, Palmen MJ, Akol H, Bloemena E, Peña AS, Meuwissen SG, Van Rees EP. Chronic experimental colitis induced by dextran sulphate sodium (DSS) is characterized by Th1 and Th2 cytokines. Clin Exp Immunol. 1998;114:385-391. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 747] [Cited by in RCA: 926] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 50. | Hoffmann M, Schwertassek U, Seydel A, Weber K, Falk W, Hauschildt S, Lehmann J. A refined and translationally relevant model of chronic DSS colitis in BALB/c mice. Lab Anim. 2018;52:240-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 51. | Sussman DA, Santaolalla R, Strobel S, Dheer R, Abreu MT. Cancer in inflammatory bowel disease: lessons from animal models. Curr Opin Gastroenterol. 2012;28:327-333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 52. | Tanaka T, Kohno H, Suzuki R, Hata K, Sugie S, Niho N, Sakano K, Takahashi M, Wakabayashi K. Dextran sodium sulfate strongly promotes colorectal carcinogenesis in Apc(Min/+) mice: inflammatory stimuli by dextran sodium sulfate results in development of multiple colonic neoplasms. Int J Cancer. 2006;118:25-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 124] [Cited by in RCA: 130] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 53. | Cooper HS, Everley L, Chang WC, Pfeiffer G, Lee B, Murthy S, Clapper ML. The role of mutant Apc in the development of dysplasia and cancer in the mouse model of dextran sulfate sodium-induced colitis. Gastroenterology. 2001;121:1407-1416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 76] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 54. | De Robertis M, Massi E, Poeta ML, Carotti S, Morini S, Cecchetelli L, Signori E, Fazio VM. The AOM/DSS murine model for the study of colon carcinogenesis: From pathways to diagnosis and therapy studies. J Carcinog. 2011;10:9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 326] [Cited by in RCA: 419] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 55. | Velázquez KT, Enos RT, Carson MS, Cranford TL, Bader JE, Chatzistamou I, Singh UP, Nagarkatti PS, Nagarkatti M, Davis JM, Carson JA, Murphy EA. Weight loss following diet-induced obesity does not alter colon tumorigenesis in the AOM mouse model. Am J Physiol Gastrointest Liver Physiol. 2016;311:G699-G712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (1)] |
| 56. | Cuellar-Nuñez ML, Luzardo-Ocampo I, Campos-Vega R, Gallegos-Corona MA, González de Mejía E, Loarca-Piña G. Physicochemical and nutraceutical properties of moringa (Moringa oleifera) leaves and their effects in an in vivo AOM/DSS-induced colorectal carcinogenesis model. Food Res Int. 2018;105:159-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 57. | Canene-Adams K, Sfanos KS, Liang CT, Yegnasubramanian S, Nelson WG, Brayton C, De Marzo AM. Dietary chemoprevention of PhIP induced carcinogenesis in male Fischer 344 rats with tomato and broccoli. PLoS One. 2013;8:e79842. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 58. | Chen JX, Liu A, Lee MJ, Wang H, Yu S, Chi E, Reuhl K, Suh N, Yang CS. δ- and γ-tocopherols inhibit phIP/DSS-induced colon carcinogenesis by protection against early cellular and DNA damages. Mol Carcinog. 2017;56:172-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 59. | Bi W, Liu H, Shen J, Zhang LH, Li P, Peng B, Cao L, Zhang P, He C, Xiao P. Chemopreventive effects of Ku-jin tea against AOM-induced precancerous colorectal lesions in rats and metabolomic analysis. Sci Rep. 2017;7:15893. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 60. | Sun MC, Zhang FC, Yin X, Cheng BJ, Zhao CH, Wang YL, Zhang ZZ, Hao HW, Zhang TH, Ye HQ. Lactobacillus reuteri F-9-35 Prevents DSS-Induced Colitis by Inhibiting Proinflammatory Gene Expression and Restoring the Gut Microbiota in Mice. J Food Sci. 2018;83:2645-2652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 63] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 61. | Snider AJ, Bialkowska AB, Ghaleb AM, Yang VW, Obeid LM, Hannun YA. Murine Model for Colitis-Associated Cancer of the Colon. Methods Mol Biol. 2016;1438:245-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 84] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 62. | Yang J, Shikata N, Mizuoka H, Tsubura A. Colon carcinogenesis in shrews by intrarectal infusion of N-methyl-N-nitrosourea. Cancer Lett. 1996;110:105-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 63. | Derry MM, Raina K, Agarwal R, Agarwal C. Characterization of azoxymethane-induced colon tumor metastasis to lung in a mouse model relevant to human sporadic colorectal cancer and evaluation of grape seed extract efficacy. Exp Toxicol Pathol. 2014;66:235-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 64. | Papanikolaou A, Wang QS, Papanikolaou D, Whiteley HE, Rosenberg DW. Sequential and morphological analyses of aberrant crypt foci formation in mice of differing susceptibility to azoxymethane-induced colon carcinogenesis. Carcinogenesis. 2000;21:1567-1572. [PubMed] |
| 65. | Nambiar PR, Girnun G, Lillo NA, Guda K, Whiteley HE, Rosenberg DW. Preliminary analysis of azoxymethane induced colon tumors in inbred mice commonly used as transgenic/knockout progenitors. Int J Oncol. 2003;22:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 66. | Clapp NK, Henke MA, London JF, Shock TL. Enhancement of 1,2-dimethylhydrazine-induced large bowel tumorigenesis in Balb/c mice by corn, soybean, and wheat brans. Nutr Cancer. 1984;6:77-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 67. | Neufert C, Becker C, Neurath MF. An inducible mouse model of colon carcinogenesis for the analysis of sporadic and inflammation-driven tumor progression. Nat Protoc. 2007;2:1998-2004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 460] [Cited by in RCA: 556] [Article Influence: 30.9] [Reference Citation Analysis (0)] |
| 68. | Piñol V, Andreu M, Castells A, Payá A, Bessa X, Jover R; Gastrointestinal Oncology Group of the Spanish Gastroenterological Association. Synchronous colorectal neoplasms in patients with colorectal cancer: predisposing individual and familial factors. Dis Colon Rectum. 2004;47:1192-1200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 69. | Marqués-Lespier JM, Soto-Salgado M, González-Pons M, Méndez V, Freyre K, Beltrán C, Pericchi LR, Cruz-Correa M. Prevalence of Synchronous Oligopolyposis in Incident Colorectal Cancer: A Population-Based Study. P R Health Sci J. 2018;37:39-45. [PubMed] |
| 70. | Thaker AI, Shaker A, Rao MS, Ciorba MA. Modeling colitis-associated cancer with azoxymethane (AOM) and dextran sulfate sodium (DSS). J Vis Exp. 2012;(67). [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 96] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 71. | Matsumoto K, Iwase T, Hirono I, Nishida Y, Iwahori Y, Hori T, Asamoto M, Takasuka N, Kim DJ, Ushijima T, Nagao M, Tsuda H. Demonstration of ras and p53 gene mutations in carcinomas in the forestomach and intestine and soft tissue sarcomas induced by N-methyl-N-nitrosourea in the rat. Jpn J Cancer Res. 1997;88:129-136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 72. | Nordlinger B, Panis Y, Puts JP, Herve JP, Delelo R, Ballet F. Experimental model of colon cancer: recurrences after surgery alone or associated with intraperitoneal 5-fluorouracil chemotherapy. Dis Colon Rectum. 1991;34:658-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 73. | Narisawa T, Weisburger JH. Colon cancer induction in mice by intrarectal instillation of N-methylnitosorurea (38498). Proc Soc Exp Biol Med. 1975;148:166-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 21] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 74. | Hasegawa R, Sano M, Tamano S, Imaida K, Shirai T, Nagao M, Sugimura T, Ito N. Dose-dependence of 2-amino-1-methyl-6-phenylimidazo[4,5-b]-pyridine (PhIP) carcinogenicity in rats. Carcinogenesis. 1993;14:2553-2557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 98] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 75. | Leslie A, Carey FA, Pratt NR, Steele RJ. The colorectal adenoma-carcinoma sequence. Br J Surg. 2002;89:845-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 439] [Cited by in RCA: 462] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 76. | Jacoby RF, Llor X, Teng BB, Davidson NO, Brasitus TA. Mutations in the K-ras oncogene induced by 1,2-dimethylhydrazine in preneoplastic and neoplastic rat colonic mucosa. J Clin Invest. 1991;87:624-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 87] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 77. | De Filippo C, Caderni G, Bazzicalupo M, Briani C, Giannini A, Fazi M, Dolara P. Mutations of the Apc gene in experimental colorectal carcinogenesis induced by azoxymethane in F344 rats. Br J Cancer. 1998;77:2148-2151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 78. | Aaltonen LA, Peltomäki P, Leach FS, Sistonen P, Pylkkänen L, Mecklin JP, Järvinen H, Powell SM, Jen J, Hamilton SR. Clues to the pathogenesis of familial colorectal cancer. Science. 1993;260:812-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1810] [Cited by in RCA: 1814] [Article Influence: 56.7] [Reference Citation Analysis (0)] |
| 79. | Pan Q, Lou X, Zhang J, Zhu Y, Li F, Shan Q, Chen X, Xie Y, Su S, Wei H, Lin L, Wu L, Liu S. Genomic variants in mouse model induced by azoxymethane and dextran sodium sulfate improperly mimic human colorectal cancer. Sci Rep. 2017;7:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 80. | Cheung C, Loy S, Li GX, Liu AB, Yang CS. Rapid induction of colon carcinogenesis in CYP1A-humanized mice by 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine and dextran sodium sulfate. Carcinogenesis. 2011;32:233-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 81. | Brinster RL, Chen HY, Messing A, van Dyke T, Levine AJ, Palmiter RD. Transgenic mice harboring SV40 T-antigen genes develop characteristic brain tumors. Cell. 1984;37:367-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 339] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 82. | Adams JM, Harris AW, Pinkert CA, Corcoran LM, Alexander WS, Cory S, Palmiter RD, Brinster RL. The c-myc oncogene driven by immunoglobulin enhancers induces lymphoid malignancy in transgenic mice. Nature. 1985;318:533-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1329] [Cited by in RCA: 1356] [Article Influence: 33.9] [Reference Citation Analysis (0)] |
| 83. | Ornitz DM, Palmiter RD, Messing A, Hammer RE, Pinkert CA, Brinster RL. Elastase I promoter directs expression of human growth hormone and SV40 T antigen genes to pancreatic acinar cells in transgenic mice. Cold Spring Harb Symp Quant Biol. 1985;50:399-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 83] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 84. | Quaife CJ, Pinkert CA, Ornitz DM, Palmiter RD, Brinster RL. Pancreatic neoplasia induced by ras expression in acinar cells of transgenic mice. Cell. 1987;48:1023-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 174] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 85. | Stewart TA, Pattengale PK, Leder P. Spontaneous mammary adenocarcinomas in transgenic mice that carry and express MTV/myc fusion genes. Cell. 1984;38:627-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 629] [Cited by in RCA: 612] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 86. | Rüther U, Garber C, Komitowski D, Müller R, Wagner EF. Deregulated c-fos expression interferes with normal bone development in transgenic mice. Nature. 1987;325:412-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 261] [Cited by in RCA: 239] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 87. | Hanahan D. Heritable formation of pancreatic beta-cell tumours in transgenic mice expressing recombinant insulin/simian virus 40 oncogenes. Nature. 1985;315:115-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 957] [Cited by in RCA: 986] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 88. | Schäfer C. Nobel Price for Medicine 2007. Knockout mice are revolutionizing genetics. Ophthalmologe. 2007;104:1080-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 89. | Jacks T, Fazeli A, Schmitt EM, Bronson RT, Goodell MA, Weinberg RA. Effects of an Rb mutation in the mouse. Nature. 1992;359:295-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1284] [Cited by in RCA: 1295] [Article Influence: 39.2] [Reference Citation Analysis (0)] |
| 90. | Donehower LA, Harvey M, Slagle BL, McArthur MJ, Montgomery CA, Butel JS, Bradley A. Mice deficient for p53 are developmentally normal but susceptible to spontaneous tumours. Nature. 1992;356:215-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3399] [Cited by in RCA: 3403] [Article Influence: 103.1] [Reference Citation Analysis (0)] |
| 91. | Lakso M, Sauer B, Mosinger B, Lee EJ, Manning RW, Yu SH, Mulder KL, Westphal H. Targeted oncogene activation by site-specific recombination in transgenic mice. Proc Natl Acad Sci USA. 1992;89:6232-6236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 456] [Cited by in RCA: 484] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 92. | Meuwissen R, Linn SC, van der Valk M, Mooi WJ, Berns A. Mouse model for lung tumorigenesis through Cre/lox controlled sporadic activation of the K-Ras oncogene. Oncogene. 2001;20:6551-6558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 140] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 93. | Hingorani SR, Petricoin EF, Maitra A, Rajapakse V, King C, Jacobetz MA, Ross S, Conrads TP, Veenstra TD, Hitt BA, Kawaguchi Y, Johann D, Liotta LA, Crawford HC, Putt ME, Jacks T, Wright CV, Hruban RH, Lowy AM, Tuveson DA. Preinvasive and invasive ductal pancreatic cancer and its early detection in the mouse. Cancer Cell. 2003;4:437-450. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1827] [Cited by in RCA: 1905] [Article Influence: 86.6] [Reference Citation Analysis (0)] |
| 94. | Moser AR, Pitot HC, Dove WF. A dominant mutation that predisposes to multiple intestinal neoplasia in the mouse. Science. 1990;247:322-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1131] [Cited by in RCA: 1160] [Article Influence: 33.1] [Reference Citation Analysis (0)] |
| 95. | Shoemaker AR, Gould KA, Luongo C, Moser AR, Dove WF. Studies of neoplasia in the Min mouse. Biochim Biophys Acta. 1997;1332:F25-F48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 62] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 96. | Yamada Y, Mori H. Multistep carcinogenesis of the colon in Apc(Min/+) mouse. Cancer Sci. 2007;98:6-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 115] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 97. | Moser AR, Shoemaker AR, Connelly CS, Clipson L, Gould KA, Luongo C, Dove WF, Siggers PH, Gardner RL. Homozygosity for the Min allele of Apc results in disruption of mouse development prior to gastrulation. Dev Dyn. 1995;203:422-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 113] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 98. | Møllersen L, Paulsen JE, Alexander J. Loss of heterozygosity and nonsense mutation in Apc in azoxymethane-induced colonic tumours in min mice. Anticancer Res. 2004;24:2595-2599. [PubMed] |
| 99. | Ju J, Nolan B, Cheh M, Bose M, Lin Y, Wagner GC, Yang CS. Voluntary exercise inhibits intestinal tumorigenesis in Apc(Min/+) mice and azoxymethane/dextran sulfate sodium-treated mice. BMC Cancer. 2008;8:316. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 100. | Tanaka T, Suzuki R, Kohno H, Sugie S, Takahashi M, Wakabayashi K. Colonic adenocarcinomas rapidly induced by the combined treatment with 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine and dextran sodium sulfate in male ICR mice possess beta-catenin gene mutations and increases immunoreactivity for beta-catenin, cyclooxygenase-2 and inducible nitric oxide synthase. Carcinogenesis. 2005;26:229-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 75] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 101. | Jin D, Liu T, Dong W, Zhang Y, Wang S, Xie R, Wang B, Cao H. Dietary feeding of freeze-dried whole cranberry inhibits intestinal tumor development in Apcmin/+ mice. Oncotarget. 2017;8:97787-97800. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 102. | Ni Y, Wong VH, Tai WC, Li J, Wong WY, Lee MM, Fong FL, El-Nezami H, Panagiotou G. A metagenomic study of the preventive effect of Lactobacillus rhamnosus GG on intestinal polyp formation in ApcMin/+ mice. J Appl Microbiol. 2017;122:770-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 103. | Zhang L, Shay JW. Multiple Roles of APC and its Therapeutic Implications in Colorectal Cancer. J Natl Cancer Inst. 2017;109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 283] [Article Influence: 35.4] [Reference Citation Analysis (0)] |
| 104. | Halberg RB, Waggoner J, Rasmussen K, White A, Clipson L, Prunuske AJ, Bacher JW, Sullivan R, Washington MK, Pitot HC, Petrini JH, Albertson DG, Dove WF. Long-lived Min mice develop advanced intestinal cancers through a genetically conservative pathway. Cancer Res. 2009;69:5768-5775. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 105. | Sødring M, Gunnes G, Paulsen JE. Spontaneous initiation, promotion and progression of colorectal cancer in the novel A/J Min/+ mouse. Int J Cancer. 2016;138:1936-1946. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 106. | Fodde R, Edelmann W, Yang K, van Leeuwen C, Carlson C, Renault B, Breukel C, Alt E, Lipkin M, Khan PM. A targeted chain-termination mutation in the mouse Apc gene results in multiple intestinal tumors. Proc Natl Acad Sci USA. 1994;91:8969-8973. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 388] [Cited by in RCA: 379] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 107. | Smits R, Kartheuser A, Jagmohan-Changur S, Leblanc V, Breukel C, de Vries A, van Kranen H, van Krieken JH, Williamson S, Edelmann W, Kucherlapati R, KhanPM, Fodde R. Loss of Apc and the entire chromosome 18 but absence of mutations at the Ras and Tp53 genes in intestinal tumors from Apc1638N, a mouse model for Apc-driven carcinogenesis. Carcinogenesis. 1997;18:321-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 75] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 108. | Oshima M, Oshima H, Kitagawa K, Kobayashi M, Itakura C, Taketo M. Loss of Apc heterozygosity and abnormal tissue building in nascent intestinal polyps in mice carrying a truncated Apc gene. Proc Natl Acad Sci USA. 1995;92:4482-4486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 409] [Cited by in RCA: 412] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 109. | Crist RC, Roth JJ, Baran AA, McEntee BJ, Siracusa LD, Buchberg AM. The armadillo repeat domain of Apc suppresses intestinal tumorigenesis. Mamm Genome. 2010;21:450-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 110. | Colnot S, Niwa-Kawakita M, Hamard G, Godard C, Le Plenier S, Houbron C, Romagnolo B, Berrebi D, Giovannini M, Perret C. Colorectal cancers in a new mouse model of familial adenomatous polyposis: influence of genetic and environmental modifiers. Lab Invest. 2004;84:1619-1630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 144] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 111. | Fazeli A, Steen RG, Dickinson SL, Bautista D, Dietrich WF, Bronson RT, Bresalier RS, Lander ES, Costa J, Weinberg RA. Effects of p53 mutations on apoptosis in mouse intestinal and human colonic adenomas. Proc Natl Acad Sci USA. 1997;94:10199-10204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 112. | Clarke AR, Cummings MC, Harrison DJ. Interaction between murine germline mutations in p53 and APC predisposes to pancreatic neoplasia but not to increased intestinal malignancy. Oncogene. 1995;11:1913-1920. [PubMed] |
| 113. | Halberg RB, Katzung DS, Hoff PD, Moser AR, Cole CE, Lubet RA, Donehower LA, Jacoby RF, Dove WF. Tumorigenesis in the multiple intestinal neoplasia mouse: redundancy of negative regulators and specificity of modifiers. Proc Natl Acad Sci USA. 2000;97:3461-3466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 72] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 114. | Maslon MM, Hupp TR. Drug discovery and mutant p53. Trends Cell Biol. 2010;20:542-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 115. | Billant O, Léon A, Le Guellec S, Friocourt G, Blondel M, Voisset C. The dominant-negative interplay between p53, p63 and p73: A family affair. Oncotarget. 2016;7:69549-69564. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 116. | Tuveson DA, Shaw AT, Willis NA, Silver DP, Jackson EL, Chang S, Mercer KL, Grochow R, Hock H, Crowley D, Hingorani SR, Zaks T, King C, Jacobetz MA, Wang L, Bronson RT, Orkin SH, DePinho RA, Jacks T. Endogenous oncogenic K-ras(G12D) stimulates proliferation and widespread neoplastic and developmental defects. Cancer Cell. 2004;5:375-387. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 608] [Cited by in RCA: 636] [Article Influence: 30.3] [Reference Citation Analysis (0)] |
| 117. | Guerra C, Mijimolle N, Dhawahir A, Dubus P, Barradas M, Serrano M, Campuzano V, Barbacid M. Tumor induction by an endogenous K-ras oncogene is highly dependent on cellular context. Cancer Cell. 2003;4:111-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 450] [Cited by in RCA: 461] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 118. | el Marjou F, Janssen KP, Chang BH, Li M, Hindie V, Chan L, Louvard D, Chambon P, Metzger D, Robine S. Tissue-specific and inducible Cre-mediated recombination in the gut epithelium. Genesis. 2004;39:186-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 738] [Cited by in RCA: 862] [Article Influence: 43.1] [Reference Citation Analysis (0)] |
| 119. | Saam JR, Gordon JI. Inducible gene knockouts in the small intestinal and colonic epithelium. J Biol Chem. 1999;274:38071-38082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 160] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 120. | Robanus-Maandag EC, Koelink PJ, Breukel C, Salvatori DC, Jagmohan-Changur SC, Bosch CA, Verspaget HW, Devilee P, Fodde R, Smits R. A new conditional Apc-mutant mouse model for colorectal cancer. Carcinogenesis. 2010;31:946-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 121. | Ireland H, Kemp R, Houghton C, Howard L, Clarke AR, Sansom OJ, Winton DJ. Inducible Cre-mediated control of gene expression in the murine gastrointestinal tract: effect of loss of beta-catenin. Gastroenterology. 2004;126:1236-1246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 283] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 122. | Sansom OJ, Meniel V, Wilkins JA, Cole AM, Oien KA, Marsh V, Jamieson TJ, Guerra C, Ashton GH, Barbacid M, Clarke AR. Loss of Apc allows phenotypic manifestation of the transforming properties of an endogenous K-ras oncogene in vivo. Proc Natl Acad Sci USA. 2006;103:14122-14127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 167] [Cited by in RCA: 166] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 123. | Sansom OJ, Griffiths DF, Reed KR, Winton DJ, Clarke AR. Apc deficiency predisposes to renal carcinoma in the mouse. Oncogene. 2005;24:8205-8210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 124. | Hinoi T, Akyol A, Theisen BK, Ferguson DO, Greenson JK, Williams BO, Cho KR, Fearon ER. Mouse model of colonic adenoma-carcinoma progression based on somatic Apc inactivation. Cancer Res. 2007;67:9721-9730. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 215] [Cited by in RCA: 259] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 125. | Akyol A, Hinoi T, Feng Y, Bommer GT, Glaser TM, Fearon ER. Generating somatic mosaicism with a Cre recombinase-microsatellite sequence transgene. Nat Methods. 2008;5:231-233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 126. | Xue Y, Johnson R, Desmet M, Snyder PW, Fleet JC. Generation of a transgenic mouse for colorectal cancer research with intestinal cre expression limited to the large intestine. Mol Cancer Res. 2010;8:1095-1104. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 127. | Shibata H, Toyama K, Shioya H, Ito M, Hirota M, Hasegawa S, Matsumoto H, Takano H, Akiyama T, Toyoshima K, Kanamaru R, Kanegae Y, Saito I, Nakamura Y, Shiba K, Noda T. Rapid colorectal adenoma formation initiated by conditional targeting of the Apc gene. Science. 1997;278:120-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 472] [Cited by in RCA: 475] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 128. | Roper J, Tammela T, Cetinbas NM, Akkad A, Roghanian A, Rickelt S, Almeqdadi M, Wu K, Oberli MA, Sánchez-Rivera FJ, Park YK, Liang X, Eng G, Taylor MS, Azimi R, Kedrin D, Neupane R, Beyaz S, Sicinska ET, Suarez Y, Yoo J, Chen L, Zukerberg L, Katajisto P, Deshpande V, Bass AJ, Tsichlis PN, Lees J, Langer R, Hynes RO, Chen J, Bhutkar A, Jacks T, Yilmaz ÖH. In vivo genome editing and organoid transplantation models of colorectal cancer and metastasis. Nat Biotechnol. 2017;35:569-576. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 254] [Cited by in RCA: 257] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 129. | Hadac JN, Leystra AA, Paul Olson TJ, Maher ME, Payne SN, Yueh AE, Schwartz AR, Albrecht DM, Clipson L, Pasch CA, Matkowskyj KA, Halberg RB, Deming DA. Colon Tumors with the Simultaneous Induction of Driver Mutations in APC, KRAS, and PIK3CA Still Progress through the Adenoma-to-carcinoma Sequence. Cancer Prev Res (Phila). 2015;8:952-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 130. | Hung KE, Maricevich MA, Richard LG, Chen WY, Richardson MP, Kunin A, Bronson RT, Mahmood U, Kucherlapati R. Development of a mouse model for sporadic and metastatic colon tumors and its use in assessing drug treatment. Proc Natl Acad Sci USA. 2010;107:1565-1570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 165] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 131. | Sansom OJ, Reed KR, Hayes AJ, Ireland H, Brinkmann H, Newton IP, Batlle E, Simon-Assmann P, Clevers H, Nathke IS, Clarke AR, Winton DJ. Loss of Apc in vivo immediately perturbs Wnt signaling, differentiation, and migration. Genes Dev. 2004;18:1385-1390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 615] [Cited by in RCA: 632] [Article Influence: 30.1] [Reference Citation Analysis (0)] |
| 132. | Cheung AF, Carter AM, Kostova KK, Woodruff JF, Crowley D, Bronson RT, Haigis KM, Jacks T. Complete deletion of Apc results in severe polyposis in mice. Oncogene. 2010;29:1857-1864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 133. | Feng Y, Sentani K, Wiese A, Sands E, Green M, Bommer GT, Cho KR, Fearon ER. Sox9 induction, ectopic Paneth cells, and mitotic spindle axis defects in mouse colon adenomatous epithelium arising from conditional biallelic Apc inactivation. Am J Pathol. 2013;183:493-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 134. | Calcagno SR, Li S, Colon M, Kreinest PA, Thompson EA, Fields AP, Murray NR. Oncogenic K-ras promotes early carcinogenesis in the mouse proximal colon. Int J Cancer. 2008;122:2462-2470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 59] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 135. | Luo F, Brooks DG, Ye H, Hamoudi R, Poulogiannis G, Patek CE, Winton DJ, Arends MJ. Mutated K-ras(Asp12) promotes tumourigenesis in Apc(Min) mice more in the large than the small intestines, with synergistic effects between K-ras and Wnt pathways. Int J Exp Pathol. 2009;90:558-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 136. | Haigis KM, Kendall KR, Wang Y, Cheung A, Haigis MC, Glickman JN, Niwa-Kawakita M, Sweet-Cordero A, Sebolt-Leopold J, Shannon KM, Settleman J, Giovannini M, Jacks T. Differential effects of oncogenic K-Ras and N-Ras on proliferation, differentiation and tumor progression in the colon. Nat Genet. 2008;40:600-608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 497] [Cited by in RCA: 468] [Article Influence: 27.5] [Reference Citation Analysis (1)] |
| 137. | Russo A, Bazan V, Iacopetta B, Kerr D, Soussi T, Gebbia N; TP53-CRC Collaborative Study Group. The TP53 colorectal cancer international collaborative study on the prognostic and predictive significance of p53 mutation: influence of tumor site, type of mutation, and adjuvant treatment. J Clin Oncol. 2005;23:7518-7528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 297] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 138. | Iacopetta B, Russo A, Bazan V, Dardanoni G, Gebbia N, Soussi T, Kerr D, Elsaleh H, Soong R, Kandioler D, Janschek E, Kappel S, Lung M, Leung CS, Ko JM, Yuen S, Ho J, Leung SY, Crapez E, Duffour J, Ychou M, Leahy DT, O'Donoghue DP, Agnese V, Cascio S, Di Fede G, Chieco-Bianchi L, Bertorelle R, Belluco C, Giaretti W, Castagnola P, Ricevuto E, Ficorella C, Bosari S, Arizzi CD, Miyaki M, Onda M, Kampman E, Diergaarde B, Royds J, Lothe RA, Diep CB, Meling GI, Ostrowski J, Trzeciak L, Guzinska-Ustymowicz K, Zalewski B, Capellá GM, Moreno V, Peinado MA, Lönnroth C, Lundholm K, Sun XF, Jansson A, Bouzourene H, Hsieh LL, Tang R, Smith DR, Allen-Mersh TG, Khan ZA, Shorthouse AJ, Silverman ML, Kato S, Ishioka C; TP53-CRC Collaborative Group. Functional categories of TP53 mutation in colorectal cancer: results of an International Collaborative Study. Ann Oncol. 2006;17:842-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 85] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 139. | Nakayama M, Sakai E, Echizen K, Yamada Y, Oshima H, Han TS, Ohki R, Fujii S, Ochiai A, Robine S, Voon DC, Tanaka T, Taketo MM, Oshima M. Intestinal cancer progression by mutant p53 through the acquisition of invasiveness associated with complex glandular formation. Oncogene. 2017;36:5885-5896. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 54] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 140. | Sakai E, Nakayama M, Oshima H, Kouyama Y, Niida A, Fujii S, Ochiai A, Nakayama KI, Mimori K, Suzuki Y, Hong CP, Ock CY, Kim SJ, Oshima M. Combined Mutation of Apc, Kras, and Tgfbr2 Effectively Drives Metastasis of Intestinal Cancer. Cancer Res. 2018;78:1334-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 102] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 141. | Chanrion M, Kuperstein I, Barrière C, El Marjou F, Cohen D, Vignjevic D, Stimmer L, Paul-Gilloteaux P, Bièche I, Tavares Sdos R, Boccia GF, Cacheux W, Meseure D, Fre S, Martignetti L, Legoix-Né P, Girard E, Fetler L, Barillot E, Louvard D, Zinovyev A, Robine S. Concomitant Notch activation and p53 deletion trigger epithelial-to-mesenchymal transition and metastasis in mouse gut. Nat Commun. 2014;5:5005. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 111] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 142. | Fre S, Pallavi SK, Huyghe M, Laé M, Janssen KP, Robine S, Artavanis-Tsakonas S, Louvard D. Notch and Wnt signals cooperatively control cell proliferation and tumorigenesis in the intestine. Proc Natl Acad Sci USA. 2009;106:6309-6314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 245] [Cited by in RCA: 265] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 143. | Dow LE, O'Rourke KP, Simon J, Tschaharganeh DF, van Es JH, Clevers H, Lowe SW. Apc Restoration Promotes Cellular Differentiation and Reestablishes Crypt Homeostasis in Colorectal Cancer. Cell. 2015;161:1539-1552. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 324] [Cited by in RCA: 412] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 144. | Mao JH, Perez-Losada J, Wu D, Delrosario R, Tsunematsu R, Nakayama KI, Brown K, Bryson S, Balmain A. Fbxw7/Cdc4 is a p53-dependent, haploinsufficient tumour suppressor gene. Nature. 2004;432:775-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 323] [Cited by in RCA: 319] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 145. | Welcker M, Clurman BE. FBW7 ubiquitin ligase: a tumour suppressor at the crossroads of cell division, growth and differentiation. Nat Rev Cancer. 2008;8:83-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 811] [Cited by in RCA: 873] [Article Influence: 51.4] [Reference Citation Analysis (0)] |
| 146. | Babaei-Jadidi R, Li N, Saadeddin A, Spencer-Dene B, Jandke A, Muhammad B, Ibrahim EE, Muraleedharan R, Abuzinadah M, Davis H, Lewis A, Watson S, Behrens A, Tomlinson I, Nateri AS. FBXW7 influences murine intestinal homeostasis and cancer, targeting Notch, Jun, and DEK for degradation. J Exp Med. 2011;208:295-312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 135] [Cited by in RCA: 149] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 147. | Sancho R, Jandke A, Davis H, Diefenbacher ME, Tomlinson I, Behrens A. F-box and WD repeat domain-containing 7 regulates intestinal cell lineage commitment and is a haploinsufficient tumor suppressor. Gastroenterology. 2010;139:929-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 107] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 148. | Grim JE, Knoblaugh SE, Guthrie KA, Hagar A, Swanger J, Hespelt J, Delrow JJ, Small T, Grady WM, Nakayama KI, Clurman BE. Fbw7 and p53 cooperatively suppress advanced and chromosomally unstable intestinal cancer. Mol Cell Biol. 2012;32:2160-2167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 68] [Article Influence: 5.2] [Reference Citation Analysis (1)] |
| 149. | Faes S, Dormond O. PI3K and AKT: Unfaithful Partners in Cancer. Int J Mol Sci. 2015;16:21138-21152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 195] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 150. | Leystra AA, Deming DA, Zahm CD, Farhoud M, Olson TJ, Hadac JN, Nettekoven LA, Albrecht DM, Clipson L, Sullivan R, Washington MK, Torrealba JR, Weichert JP, Halberg RB. Mice expressing activated PI3K rapidly develop advanced colon cancer. Cancer Res. 2012;72:2931-2936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 50] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 151. | Marsh V, Winton DJ, Williams GT, Dubois N, Trumpp A, Sansom OJ, Clarke AR. Epithelial Pten is dispensable for intestinal homeostasis but suppresses adenoma development and progression after Apc mutation. Nat Genet. 2008;40:1436-1444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 90] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 152. | Davies EJ, Marsh Durban V, Meniel V, Williams GT, Clarke AR. PTEN loss and KRAS activation leads to the formation of serrated adenomas and metastatic carcinoma in the mouse intestine. J Pathol. 2014;233:27-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (2)] |
| 153. | Yu M, Trobridge P, Wang Y, Kanngurn S, Morris SM, Knoblaugh S, Grady WM. Inactivation of TGF-β signaling and loss of PTEN cooperate to induce colon cancer in vivo. Oncogene. 2014;33:1538-1547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 154. | Syed V. TGF-β Signaling in Cancer. J Cell Biochem. 2016;117:1279-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 355] [Article Influence: 39.4] [Reference Citation Analysis (0)] |
| 155. | Nagaraj NS, Datta PK. Targeting the transforming growth factor-beta signaling pathway in human cancer. Expert Opin Investig Drugs. 2010;19:77-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 214] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 156. | Alberici P, Jagmohan-Changur S, De Pater E, Van Der Valk M, Smits R, Hohenstein P, Fodde R. Smad4 haploinsufficiency in mouse models for intestinal cancer. Oncogene. 2006;25:1841-1851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 157. | Takaku K, Oshima M, Miyoshi H, Matsui M, Seldin MF, Taketo MM. Intestinal tumorigenesis in compound mutant mice of both Dpc4 (Smad4) and Apc genes. Cell. 1998;92:645-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 446] [Cited by in RCA: 433] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 158. | Tetteh PW, Kretzschmar K, Begthel H, van den Born M, Korving J, Morsink F, Farin H, van Es JH, Offerhaus GJ, Clevers H. Generation of an inducible colon-specific Cre enzyme mouse line for colon cancer research. Proc Natl Acad Sci USA. 2016;113:11859-11864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 159. | Takaku K, Wrana JL, Robertson EJ, Taketo MM. No effects of Smad2 (madh2) null mutation on malignant progression of intestinal polyps in Apc(delta716) knockout mice. Cancer Res. 2002;62:4558-4561. [PubMed] |
| 160. | Zhu Y, Richardson JA, Parada LF, Graff JM. Smad3 mutant mice develop metastatic colorectal cancer. Cell. 1998;94:703-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 510] [Cited by in RCA: 485] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 161. | Sodir NM, Chen X, Park R, Nickel AE, Conti PS, Moats R, Bading JR, Shibata D, Laird PW. Smad3 deficiency promotes tumorigenesis in the distal colon of ApcMin/+ mice. Cancer Res. 2006;66:8430-8438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 72] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 162. | Fleming NI, Jorissen RN, Mouradov D, Christie M, Sakthianandeswaren A, Palmieri M, Day F, Li S, Tsui C, Lipton L, Desai J, Jones IT, McLaughlin S, Ward RL, Hawkins NJ, Ruszkiewicz AR, Moore J, Zhu HJ, Mariadason JM, Burgess AW, Busam D, Zhao Q, Strausberg RL, Gibbs P, Sieber OM. SMAD2, SMAD3 and SMAD4 mutations in colorectal cancer. Cancer Res. 2013;73:725-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 194] [Cited by in RCA: 261] [Article Influence: 20.1] [Reference Citation Analysis (0)] |
| 163. | Engle SJ, Hoying JB, Boivin GP, Ormsby I, Gartside PS, Doetschman T. Transforming growth factor beta1 suppresses nonmetastatic colon cancer at an early stage of tumorigenesis. Cancer Res. 1999;59:3379-3386. [PubMed] |
| 164. | Biswas S, Guix M, Rinehart C, Dugger TC, Chytil A, Moses HL, Freeman ML, Arteaga CL. Inhibition of TGF-beta with neutralizing antibodies prevents radiation-induced acceleration of metastatic cancer progression. J Clin Invest. 2007;117:1305-1313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 289] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 165. | Oshima H, Nakayama M, Han TS, Naoi K, Ju X, Maeda Y, Robine S, Tsuchiya K, Sato T, Sato H, Taketo MM, Oshima M. Suppressing TGFβ signaling in regenerating epithelia in an inflammatory microenvironment is sufficient to cause invasive intestinal cancer. Cancer Res. 2015;75:766-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 81] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 166. | Trobridge P, Knoblaugh S, Washington MK, Munoz NM, Tsuchiya KD, Rojas A, Song X, Ulrich CM, Sasazuki T, Shirasawa S, Grady WM. TGF-beta receptor inactivation and mutant Kras induce intestinal neoplasms in mice via a beta-catenin-independent pathway. Gastroenterology. 2009;136:1680-8.e7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 82] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 167. | Muñoz NM, Upton M, Rojas A, Washington MK, Lin L, Chytil A, Sozmen EG, Madison BB, Pozzi A, Moon RT, Moses HL, Grady WM. Transforming growth factor beta receptor type II inactivation induces the malignant transformation of intestinal neoplasms initiated by Apc mutation. Cancer Res. 2006;66:9837-9844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 137] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 168. | Rajagopalan H, Bardelli A, Lengauer C, Kinzler KW, Vogelstein B, Velculescu VE. Tumorigenesis: RAF/RAS oncogenes and mismatch-repair status. Nature. 2002;418:934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 938] [Cited by in RCA: 952] [Article Influence: 41.4] [Reference Citation Analysis (0)] |
| 169. | Hinoue T, Weisenberger DJ, Lange CP, Shen H, Byun HM, Van Den Berg D, Malik S, Pan F, Noushmehr H, van Dijk CM, Tollenaar RA, Laird PW. Genome-scale analysis of aberrant DNA methylation in colorectal cancer. Genome Res. 2012;22:271-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 455] [Cited by in RCA: 488] [Article Influence: 34.9] [Reference Citation Analysis (0)] |
| 170. | Bond CE, Whitehall VLJ. How the BRAF V600E Mutation Defines a Distinct Subgroup of Colorectal Cancer: Molecular and Clinical Implications. Gastroenterol Res Pract. 2018;2018:9250757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 171. | Carragher LA, Snell KR, Giblett SM, Aldridge VS, Patel B, Cook SJ, Winton DJ, Marais R, Pritchard CA. V600EBraf induces gastrointestinal crypt senescence and promotes tumour progression through enhanced CpG methylation of p16INK4a. EMBO Mol Med. 2010;2:458-471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 117] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 172. | Coffee EM, Faber AC, Roper J, Sinnamon MJ, Goel G, Keung L, Wang WV, Vecchione L, de Vriendt V, Weinstein BJ, Bronson RT, Tejpar S, Xavier RJ, Engelman JA, Martin ES, Hung KE. Concomitant BRAF and PI3K/mTOR blockade is required for effective treatment of BRAF(V600E) colorectal cancer. Clin Cancer Res. 2013;19:2688-2698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 72] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 173. | Anderson RL, Balasas T, Callaghan J, Coombes RC, Evans J, Hall JA, Kinrade S, Jones D, Jones PS, Jones R, Marshall JF, Panico MB, Shaw JA, Steeg PS, Sullivan M, Tong W, Westwell AD, Ritchie JWA; Cancer Research UK and Cancer Therapeutics CRC Australia Metastasis Working Group. A framework for the development of effective anti-metastatic agents. Nat Rev Clin Oncol. 2019;16:185-204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 204] [Cited by in RCA: 235] [Article Influence: 39.2] [Reference Citation Analysis (0)] |
| 174. | Rad R, Cadiñanos J, Rad L, Varela I, Strong A, Kriegl L, Constantino-Casas F, Eser S, Hieber M, Seidler B, Price S, Fraga MF, Calvanese V, Hoffman G, Ponstingl H, Schneider G, Yusa K, Grove C, Schmid RM, Wang W, Vassiliou G, Kirchner T, McDermott U, Liu P, Saur D, Bradley A. A genetic progression model of Braf(V600E)-induced intestinal tumorigenesis reveals targets for therapeutic intervention. Cancer Cell. 2013;24:15-29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 170] [Cited by in RCA: 172] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 175. | Anwar M, Kochhar R, Singh R, Bhatia A, Vaiphei K, Mahmood A, Mahmood S. Frequent activation of the β-catenin gene in sporadic colorectal carcinomas: A mutational & expression analysis. Mol Carcinog. 2016;55:1627-1638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 176. | Abdelmaksoud-Damak R, Miladi-Abdennadher I, Triki M, Khabir A, Charfi S, Ayadi L, Frikha M, Sellami-Boudawara T, Mokdad-Gargouri R. Expression and mutation pattern of β-catenin and adenomatous polyposis coli in colorectal cancer patients. Arch Med Res. 2015;46:54-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 177. | Schwitalla S, Fingerle AA, Cammareri P, Nebelsiek T, Göktuna SI, Ziegler PK, Canli O, Heijmans J, Huels DJ, Moreaux G, Rupec RA, Gerhard M, Schmid R, Barker N, Clevers H, Lang R, Neumann J, Kirchner T, Taketo MM, van den Brink GR, Sansom OJ, Arkan MC, Greten FR. Intestinal tumorigenesis initiated by dedifferentiation and acquisition of stem-cell-like properties. Cell. 2013;152:25-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 821] [Cited by in RCA: 832] [Article Influence: 69.3] [Reference Citation Analysis (0)] |
| 178. | Harada N, Tamai Y, Ishikawa T, Sauer B, Takaku K, Oshima M, Taketo MM. Intestinal polyposis in mice with a dominant stable mutation of the beta-catenin gene. EMBO J. 1999;18:5931-5942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 958] [Cited by in RCA: 1006] [Article Influence: 38.7] [Reference Citation Analysis (0)] |
| 179. | Perekatt AO, Shah PP, Cheung S, Jariwala N, Wu A, Gandhi V, Kumar N, Feng Q, Patel N, Chen L, Joshi S, Zhou A, Taketo MM, Xing J, White E, Gao N, Gatza ML, Verzi MP. SMAD4 Suppresses WNT-Driven Dedifferentiation and Oncogenesis in the Differentiated Gut Epithelium. Cancer Res. 2018;78:4878-4890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 59] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 180. | Ionov Y, Peinado MA, Malkhosyan S, Shibata D, Perucho M. Ubiquitous somatic mutations in simple repeated sequences reveal a new mechanism for colonic carcinogenesis. Nature. 1993;363:558-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1824] [Cited by in RCA: 1797] [Article Influence: 56.2] [Reference Citation Analysis (0)] |
| 181. | Thibodeau SN, Bren G, Schaid D. Microsatellite instability in cancer of the proximal colon. Science. 1993;260:816-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2062] [Cited by in RCA: 2059] [Article Influence: 64.3] [Reference Citation Analysis (0)] |
| 182. | Peltomäki P, Lothe RA, Aaltonen LA, Pylkkänen L, Nyström-Lahti M, Seruca R, David L, Holm R, Ryberg D, Haugen A. Microsatellite instability is associated with tumors that characterize the hereditary non-polyposis colorectal carcinoma syndrome. Cancer Res. 1993;53:5853-5855. [PubMed] |
| 183. | Yamamoto H, Imai K. Microsatellite instability: an update. Arch Toxicol. 2015;89:899-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 159] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 184. | Edelmann W, Yang K, Kuraguchi M, Heyer J, Lia M, Kneitz B, Fan K, Brown AM, Lipkin M, Kucherlapati R. Tumorigenesis in Mlh1 and Mlh1/Apc1638N mutant mice. Cancer Res. 1999;59:1301-1307. [PubMed] |
| 185. | Reitmair AH, Schmits R, Ewel A, Bapat B, Redston M, Mitri A, Waterhouse P, Mittrücker HW, Wakeham A, Liu B. MSH2 deficient mice are viable and susceptible to lymphoid tumours. Nat Genet. 1995;11:64-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 282] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 186. | de Wind N, Dekker M, Berns A, Radman M, te Riele H. Inactivation of the mouse Msh2 gene results in mismatch repair deficiency, methylation tolerance, hyperrecombination, and predisposition to cancer. Cell. 1995;82:321-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 593] [Cited by in RCA: 599] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 187. | Edelmann W, Yang K, Umar A, Heyer J, Lau K, Fan K, Liedtke W, Cohen PE, Kane MF, Lipford JR, Yu N, Crouse GF, Pollard JW, Kunkel T, Lipkin M, Kolodner R, Kucherlapati R. Mutation in the mismatch repair gene Msh6 causes cancer susceptibility. Cell. 1997;91:467-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 258] [Cited by in RCA: 259] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 188. | Prolla TA, Baker SM, Harris AC, Tsao JL, Yao X, Bronner CE, Zheng B, Gordon M, Reneker J, Arnheim N, Shibata D, Bradley A, Liskay RM. Tumour susceptibility and spontaneous mutation in mice deficient in Mlh1, Pms1 and Pms2 DNA mismatch repair. Nat Genet. 1998;18:276-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 266] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 189. | Baker SM, Plug AW, Prolla TA, Bronner CE, Harris AC, Yao X, Christie DM, Monell C, Arnheim N, Bradley A, Ashley T, Liskay RM. Involvement of mouse Mlh1 in DNA mismatch repair and meiotic crossing over. Nat Genet. 1996;13:336-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 599] [Cited by in RCA: 613] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 190. | Yang G, Scherer SJ, Shell SS, Yang K, Kim M, Lipkin M, Kucherlapati R, Kolodner RD, Edelmann W. Dominant effects of an Msh6 missense mutation on DNA repair and cancer susceptibility. Cancer Cell. 2004;6:139-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 124] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 191. | Reitmair AH, Cai JC, Bjerknes M, Redston M, Cheng H, Pind MT, Hay K, Mitri A, Bapat BV, Mak TW, Gallinger S. MSH2 deficiency contributes to accelerated APC-mediated intestinal tumorigenesis. Cancer Res. 1996;56:2922-2926. [PubMed] |
| 192. | Smits R, Hofland N, Edelmann W, Geugien M, Jagmohan-Changur S, Albuquerque C, Breukel C, Kucherlapati R, Kielman MF, Fodde R. Somatic Apc mutations are selected upon their capacity to inactivate the beta-catenin downregulating activity. Genes Chromosomes Cancer. 2000;29:229-239. [PubMed] |
| 193. | Kucherlapati M, Yang K, Kuraguchi M, Zhao J, Lia M, Heyer J, Kane MF, Fan K, Russell R, Brown AM, Kneitz B, Edelmann W, Kolodner RD, Lipkin M, Kucherlapati R. Haploinsufficiency of Flap endonuclease (Fen1) leads to rapid tumor progression. Proc Natl Acad Sci USA. 2002;99:9924-9929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 195] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 194. | Kucherlapati M, Nguyen A, Kuraguchi M, Yang K, Fan K, Bronson R, Wei K, Lipkin M, Edelmann W, Kucherlapati R. Tumor progression in Apc(1638N) mice with Exo1 and Fen1 deficiencies. Oncogene. 2007;26:6297-6306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 195. | Panarelli NC, Vaughn CP, Samowitz WS, Yantiss RK. Sporadic microsatellite instability-high colon cancers rarely display immunohistochemical evidence of Wnt signaling activation. Am J Surg Pathol. 2015;39:313-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 196. | Marisa L, de Reyniès A, Duval A, Selves J, Gaub MP, Vescovo L, Etienne-Grimaldi MC, Schiappa R, Guenot D, Ayadi M, Kirzin S, Chazal M, Fléjou JF, Benchimol D, Berger A, Lagarde A, Pencreach E, Piard F, Elias D, Parc Y, Olschwang S, Milano G, Laurent-Puig P, Boige V. Gene expression classification of colon cancer into molecular subtypes: characterization, validation, and prognostic value. PLoS Med. 2013;10:e1001453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 871] [Cited by in RCA: 1058] [Article Influence: 88.2] [Reference Citation Analysis (0)] |
| 197. | Kucherlapati MH, Lee K, Nguyen AA, Clark AB, Hou H, Rosulek A, Li H, Yang K, Fan K, Lipkin M, Bronson RT, Jelicks L, Kunkel TA, Kucherlapati R, Edelmann W. An Msh2 conditional knockout mouse for studying intestinal cancer and testing anticancer agents. Gastroenterology. 2010;138:993-1002.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 91] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 198. | Bennecke M, Kriegl L, Bajbouj M, Retzlaff K, Robine S, Jung A, Arkan MC, Kirchner T, Greten FR. Ink4a/Arf and oncogene-induced senescence prevent tumor progression during alternative colorectal tumorigenesis. Cancer Cell. 2010;18:135-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 152] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 199. | Huang D, Sun W, Zhou Y, Li P, Chen F, Chen H, Xia D, Xu E, Lai M, Wu Y, Zhang H. Mutations of key driver genes in colorectal cancer progression and metastasis. Cancer Metastasis Rev. 2018;37:173-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 212] [Article Influence: 35.3] [Reference Citation Analysis (0)] |
| 200. | Starr TK, Allaei R, Silverstein KA, Staggs RA, Sarver AL, Bergemann TL, Gupta M, O'Sullivan MG, Matise I, Dupuy AJ, Collier LS, Powers S, Oberg AL, Asmann YW, Thibodeau SN, Tessarollo L, Copeland NG, Jenkins NA, Cormier RT, Largaespada DA. A transposon-based genetic screen in mice identifies genes altered in colorectal cancer. Science. 2009;323:1747-1750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 298] [Cited by in RCA: 290] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 201. | Takeda H, Wei Z, Koso H, Rust AG, Yew CC, Mann MB, Ward JM, Adams DJ, Copeland NG, Jenkins NA. Transposon mutagenesis identifies genes and evolutionary forces driving gastrointestinal tract tumor progression. Nat Genet. 2015;47:142-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 94] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 202. | Morris SM, Davison J, Carter KT, O'Leary RM, Trobridge P, Knoblaugh SE, Myeroff LL, Markowitz SD, Brett BT, Scheetz TE, Dupuy AJ, Starr TK, Grady WM. Transposon mutagenesis identifies candidate genes that cooperate with loss of transforming growth factor-beta signaling in mouse intestinal neoplasms. Int J Cancer. 2017;140:853-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 203. | Shabad LM. Mstislav Novinsky, pioneer of tumour transplantation. Cancer Lett. 1976;2:1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 204. | Hanau A. Erfolgreiche Übertragung von Carcinom. Fortschr d Med. 1889;7:321. |
| 205. | Triolo VA. Nineteenth century foundations of cancer research. Origins of experimental research. Cancer Res. 1964;24:4-27. [PubMed] |
| 206. | DeVita VT, Chu E. A history of cancer chemotherapy. Cancer Res. 2008;68:8643-8653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 975] [Cited by in RCA: 1115] [Article Influence: 65.6] [Reference Citation Analysis (0)] |
| 207. | Thorsby E. A short history of HLA. Tissue Antigens. 2009;74:101-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 94] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 208. | Wyke JA. Oncogenic viruses. J Pathol. 1981;135:39-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 6] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 209. | TOOLAN HW. Successful subcutaneous growth and transplantation of human tumors in X-irradiated laboratory animals. Proc Soc Exp Biol Med. 1951;77:572-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 48] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 210. | TOOLAN HW. Transplantable human neoplasms maintained in cortisone-treated laboratory animals: H.S. No. 1; H.Ep. No. 1; H.Ep. No. 2; H.Ep. No. 3; and H.Emb.Rh. No. 1. Cancer Res. 1954;14:660-666. [PubMed] |
| 211. | Yong KSM, Her Z, Chen Q. Humanized Mice as Unique Tools for Human-Specific Studies. Arch Immunol Ther Exp (Warsz). 2018;66:245-266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 77] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 212. | Flanagan SP. 'Nude', a new hairless gene with pleiotropic effects in the mouse. Genet Res. 1966;8:295-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 563] [Cited by in RCA: 524] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 213. | Rygaard J, Povlsen CO. Heterotransplantation of a human malignant tumour to "Nude" mice. Acta Pathol Microbiol Scand. 1969;77:758-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 475] [Cited by in RCA: 418] [Article Influence: 26.1] [Reference Citation Analysis (0)] |
| 214. | Bosma GC, Custer RP, Bosma MJ. A severe combined immunodeficiency mutation in the mouse. Nature. 1983;301:527-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1545] [Cited by in RCA: 1586] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 215. | Makino S, Kunimoto K, Muraoka Y, Mizushima Y, Katagiri K, Tochino Y. Breeding of a non-obese, diabetic strain of mice. Jikken Dobutsu. 1980;29:1-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 540] [Cited by in RCA: 679] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 216. | Greiner DL, Shultz LD, Yates J, Appel MC, Perdrizet G, Hesselton RM, Schweitzer I, Beamer WG, Shultz KL, Pelsue SC. Improved engraftment of human spleen cells in NOD/LtSz-scid/scid mice as compared with C.B-17-scid/scid mice. Am J Pathol. 1995;146:888-902. [PubMed] |
| 217. | Christianson SW, Greiner DL, Hesselton RA, Leif JH, Wagar EJ, Schweitzer IB, Rajan TV, Gott B, Roopenian DC, Shultz LD. Enhanced human CD4+ T cell engraftment in beta2-microglobulin-deficient NOD-scid mice. J Immunol. 1997;158:3578-3586. [PubMed] |
| 218. | Ueda T, Tsuji K, Yoshino H, Ebihara Y, Yagasaki H, Hisakawa H, Mitsui T, Manabe A, Tanaka R, Kobayashi K, Ito M, Yasukawa K, Nakahata T. Expansion of human NOD/SCID-repopulating cells by stem cell factor, Flk2/Flt3 ligand, thrombopoietin, IL-6, and soluble IL-6 receptor. J Clin Invest. 2000;105:1013-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 224] [Cited by in RCA: 224] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 219. | Santagostino SF, Arbona RJR, Nashat MA, White JR, Monette S. Pathology of Aging in NOD scid gamma Female Mice. Vet Pathol. 2017;54:855-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 220. | Nonoyama S, Smith FO, Bernstein ID, Ochs HD. Strain-dependent leakiness of mice with severe combined immune deficiency. J Immunol. 1993;150:3817-3824. [PubMed] |
| 221. | Shultz LD, Ishikawa F, Greiner DL. Humanized mice in translational biomedical research. Nat Rev Immunol. 2007;7:118-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 968] [Cited by in RCA: 1013] [Article Influence: 56.3] [Reference Citation Analysis (0)] |
| 222. | Ito M, Hiramatsu H, Kobayashi K, Suzue K, Kawahata M, Hioki K, Ueyama Y, Koyanagi Y, Sugamura K, Tsuji K, Heike T, Nakahata T. NOD/SCID/gamma(c)(null) mouse: an excellent recipient mouse model for engraftment of human cells. Blood. 2002;100:3175-3182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1108] [Cited by in RCA: 1140] [Article Influence: 49.6] [Reference Citation Analysis (0)] |
| 223. | Shultz LD, Lyons BL, Burzenski LM, Gott B, Chen X, Chaleff S, Kotb M, Gillies SD, King M, Mangada J, Greiner DL, Handgretinger R. Human lymphoid and myeloid cell development in NOD/LtSz-scid IL2R gamma null mice engrafted with mobilized human hemopoietic stem cells. J Immunol. 2005;174:6477-6489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1201] [Cited by in RCA: 1343] [Article Influence: 67.2] [Reference Citation Analysis (0)] |
| 224. | Suzuki K, Nakajima H, Saito Y, Saito T, Leonard WJ, Iwamoto I. Janus kinase 3 (Jak3) is essential for common cytokine receptor gamma chain (gamma(c))-dependent signaling: comparative analysis of gamma(c), Jak3, and gamma(c) and Jak3 double-deficient mice. Int Immunol. 2000;12:123-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 112] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 225. | Shultz LD, Banuelos S, Lyons B, Samuels R, Burzenski L, Gott B, Lang P, Leif J, Appel M, Rossini A, Greiner DL. NOD/LtSz-Rag1nullPfpnull mice: a new model system with increased levels of human peripheral leukocyte and hematopoietic stem-cell engraftment. Transplantation. 2003;76:1036-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 54] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 226. | Pearson T, Greiner DL, Shultz LD. Creation of "humanized" mice to study human immunity. Curr Protoc Immunol. 2008;Chapter 15:Unit 15.21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 116] [Cited by in RCA: 145] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 227. | Foreman O, Kavirayani AM, Griffey SM, Reader R, Shultz LD. Opportunistic bacterial infections in breeding colonies of the NSG mouse strain. Vet Pathol. 2011;48:495-499. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 228. | Gock M, Kühn F, Mullins CS, Krohn M, Prall F, Klar E, Linnebacher M. Tumor Take Rate Optimization for Colorectal Carcinoma Patient-Derived Xenograft Models. Biomed Res Int. 2016;2016:1715053. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 229. | Linnebacher M, Maletzki C, Ostwald C, Klier U, Krohn M, Klar E, Prall F. Cryopreservation of human colorectal carcinomas prior to xenografting. BMC Cancer. 2010;10:362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 64] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 230. | Simon MM, Greenaway S, White JK, Fuchs H, Gailus-Durner V, Wells S, Sorg T, Wong K, Bedu E, Cartwright EJ, Dacquin R, Djebali S, Estabel J, Graw J, Ingham NJ, Jackson IJ, Lengeling A, Mandillo S, Marvel J, Meziane H, Preitner F, Puk O, Roux M, Adams DJ, Atkins S, Ayadi A, Becker L, Blake A, Brooker D, Cater H, Champy MF, Combe R, Danecek P, di Fenza A, Gates H, Gerdin AK, Golini E, Hancock JM, Hans W, Hölter SM, Hough T, Jurdic P, Keane TM, Morgan H, Müller W, Neff F, Nicholson G, Pasche B, Roberson LA, Rozman J, Sanderson M, Santos L, Selloum M, Shannon C, Southwell A, Tocchini-Valentini GP, Vancollie VE, Westerberg H, Wurst W, Zi M, Yalcin B, Ramirez-Solis R, Steel KP, Mallon AM, de Angelis MH, Herault Y, Brown SD. A comparative phenotypic and genomic analysis of C57BL/6J and C57BL/6N mouse strains. Genome Biol. 2013;14:R82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 355] [Cited by in RCA: 393] [Article Influence: 32.8] [Reference Citation Analysis (0)] |
| 231. | Houghton PJ, Morton CL, Tucker C, Payne D, Favours E, Cole C, Gorlick R, Kolb EA, Zhang W, Lock R, Carol H, Tajbakhsh M, Reynolds CP, Maris JM, Courtright J, Keir ST, Friedman HS, Stopford C, Zeidner J, Wu J, Liu T, Billups CA, Khan J, Ansher S, Zhang J, Smith MA. The pediatric preclinical testing program: description of models and early testing results. Pediatr Blood Cancer. 2007;49:928-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 377] [Cited by in RCA: 382] [Article Influence: 21.2] [Reference Citation Analysis (0)] |
| 232. | Johnson JI, Decker S, Zaharevitz D, Rubinstein LV, Venditti JM, Schepartz S, Kalyandrug S, Christian M, Arbuck S, Hollingshead M, Sausville EA. Relationships between drug activity in NCI preclinical in vitro and in vivo models and early clinical trials. Br J Cancer. 2001;84:1424-1431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 624] [Cited by in RCA: 615] [Article Influence: 25.6] [Reference Citation Analysis (0)] |
| 233. | Talmadge JE, Singh RK, Fidler IJ, Raz A. Murine models to evaluate novel and conventional therapeutic strategies for cancer. Am J Pathol. 2007;170:793-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 373] [Cited by in RCA: 341] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 234. | Boven E, Winograd B, Berger DP, Dumont MP, Braakhuis BJ, Fodstad O, Langdon S, Fiebig HH. Phase II preclinical drug screening in human tumor xenografts: a first European multicenter collaborative study. Cancer Res. 1992;52:5940-5947. [PubMed] |
| 235. | Voskoglou-Nomikos T, Pater JL, Seymour L. Clinical predictive value of the in vitro cell line, human xenograft, and mouse allograft preclinical cancer models. Clin Cancer Res. 2003;9:4227-4239. [PubMed] |
| 236. | Golovko D, Kedrin D, Yilmaz ÖH, Roper J. Colorectal cancer models for novel drug discovery. Expert Opin Drug Discov. 2015;10:1217-1229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 37] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 237. | Katsiampoura A, Raghav K, Jiang ZQ, Menter DG, Varkaris A, Morelli MP, Manuel S, Wu J, Sorokin AV, Rizi BS, Bristow C, Tian F, Airhart S, Cheng M, Broom BM, Morris J, Overman MJ, Powis G, Kopetz S. Modeling of Patient-Derived Xenografts in Colorectal Cancer. Mol Cancer Ther. 2017;16:1435-1442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 238. | Brattain MG, Fine WD, Khaled FM, Thompson J, Brattain DE. Heterogeneity of malignant cells from a human colonic carcinoma. Cancer Res. 1981;41:1751-1756. [PubMed] |
| 239. | Horbach SPJM, Halffman W. The ghosts of HeLa: How cell line misidentification contaminates the scientific literature. PLoS One. 2017;12:e0186281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 101] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 240. | Mouradov D, Sloggett C, Jorissen RN, Love CG, Li S, Burgess AW, Arango D, Strausberg RL, Buchanan D, Wormald S, O'Connor L, Wilding JL, Bicknell D, Tomlinson IP, Bodmer WF, Mariadason JM, Sieber OM. Colorectal cancer cell lines are representative models of the main molecular subtypes of primary cancer. Cancer Res. 2014;74:3238-3247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 294] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 241. | Wilding JL, Bodmer WF. Cancer cell lines for drug discovery and development. Cancer Res. 2014;74:2377-2384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 305] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 242. | Tanaka Y, Wu AY, Ikekawa N, Iseki K, Kawai M, Kobayashi Y. Inhibition of HT-29 human colon cancer growth under the renal capsule of severe combined immunodeficient mice by an analogue of 1,25-dihydroxyvitamin D3, DD-003. Cancer Res. 1994;54:5148-5153. [PubMed] |
| 243. | Lawrentschuk N, Rigopoulos A, Lee FT, Davis ID, Scott AM, Bolton DM. Xenografting tumour beneath the renal capsule using modern surgical equipment. Eur Surg Res. 2006;38:340-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 244. | Edelstein MB. The subrenal capsule assay: a critical commentary. Eur J Cancer Clin Oncol. 1986;22:757-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 245. | Wang Y, Wang JX, Xue H, Lin D, Dong X, Gout PW, Gao X, Pang J. Subrenal capsule grafting technology in human cancer modeling and translational cancer research. Differentiation. 2016;91:15-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 246. | Li C, Wang J, Kong J, Tang J, Wu Y, Xu E, Zhang H, Lai M. GDF15 promotes EMT and metastasis in colorectal cancer. Oncotarget. 2016;7:860-872. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 90] [Cited by in RCA: 121] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 247. | Murdocca M, Capuano R, Pucci S, Cicconi R, Polidoro C, Catini A, Martinelli E, Paolesse R, Orlandi A, Mango R, Novelli G, Di Natale C, Sangiuolo F. Targeting LOX-1 Inhibits Colorectal Cancer Metastasis in an Animal Model. Front Oncol. 2019;9:927. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 248. | Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646-674. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51728] [Cited by in RCA: 47136] [Article Influence: 3366.9] [Reference Citation Analysis (5)] |
| 249. | Brand MI, Casillas S, Dietz DW, Milsom JW, Vladisavljevic A. Development of a reliable colorectal cancer liver metastasis model. J Surg Res. 1996;63:425-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 250. | Fleten KG, Bakke KM, Mælandsmo GM, Abildgaard A, Redalen KR, Flatmark K. Use of non-invasive imaging to monitor response to aflibercept treatment in murine models of colorectal cancer liver metastases. Clin Exp Metastasis. 2017;34:51-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 251. | Li Z, Wang J, Zhou T, Ye X. Establishment of a colorectal cancer nude mouse visualization model of HIF-1α overexpression. Oncol Lett. 2016;11:2725-2732. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 252. | Mullins CS, Micheel B, Matschos S, Leuchter M, Bürtin F, Krohn M, Hühns M, Klar E, Prall F, Linnebacher M. Integrated Biobanking and Tumor Model Establishment of Human Colorectal Carcinoma Provides Excellent Tools for Preclinical Research. Cancers (Basel). 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 253. | Prall F, Maletzki C, Hühns M, Krohn M, Linnebacher M. Colorectal carcinoma tumour budding and podia formation in the xenograft microenvironment. PLoS One. 2017;12:e0186271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 254. | Guenot D, Guérin E, Aguillon-Romain S, Pencreach E, Schneider A, Neuville A, Chenard MP, Duluc I, Du Manoir S, Brigand C, Oudet P, Kedinger M, Gaub MP. Primary tumour genetic alterations and intra-tumoral heterogeneity are maintained in xenografts of human colon cancers showing chromosome instability. J Pathol. 2006;208:643-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 255. | Burgenske DM, Monsma DJ, Dylewski D, Scott SB, Sayfie AD, Kim DG, Luchtefeld M, Martin KR, Stephenson P, Hostetter G, Dujovny N, MacKeigan JP. Establishment of genetically diverse patient-derived xenografts of colorectal cancer. Am J Cancer Res. 2014;4:824-837. [PubMed] |
| 256. | Mattie M, Christensen A, Chang MS, Yeh W, Said S, Shostak Y, Capo L, Verlinsky A, An Z, Joseph I, Zhang Y, Kumar-Ganesan S, Morrison K, Stover D, Challita-Eid P. Molecular characterization of patient-derived human pancreatic tumor xenograft models for preclinical and translational development of cancer therapeutics. Neoplasia. 2013;15:1138-1150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 257. | Cho YB, Hong HK, Choi YL, Oh E, Joo KM, Jin J, Nam DH, Ko YH, Lee WY. Colorectal cancer patient-derived xenografted tumors maintain characteristic features of the original tumors. J Surg Res. 2014;187:502-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 258. | Ben-David U, Ha G, Tseng YY, Greenwald NF, Oh C, Shih J, McFarland JM, Wong B, Boehm JS, Beroukhim R, Golub TR. Patient-derived xenografts undergo mouse-specific tumor evolution. Nat Genet. 2017;49:1567-1575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 419] [Cited by in RCA: 548] [Article Influence: 68.5] [Reference Citation Analysis (0)] |
| 259. | Sebolt-Leopold JS. Development of Preclinical Models to Understand and Treat Colorectal Cancer. Clin Colon Rectal Surg. 2018;31:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 260. | Moro M, Bertolini G, Tortoreto M, Pastorino U, Sozzi G, Roz L. Patient-derived xenografts of non small cell lung cancer: resurgence of an old model for investigation of modern concepts of tailored therapy and cancer stem cells. J Biomed Biotechnol. 2012;2012:568567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 53] [Cited by in RCA: 69] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 261. | Hylander BL, Punt N, Tang H, Hillman J, Vaughan M, Bshara W, Pitoniak R, Repasky EA. Origin of the vasculature supporting growth of primary patient tumor xenografts. J Transl Med. 2013;11:110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 59] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 262. | Blomme A, Van Simaeys G, Doumont G, Costanza B, Bellier J, Otaka Y, Sherer F, Lovinfosse P, Boutry S, Palacios AP, De Pauw E, Hirano T, Yokobori T, Hustinx R, Bellahcène A, Delvenne P, Detry O, Goldman S, Nishiyama M, Castronovo V, Turtoi A. Murine stroma adopts a human-like metabolic phenotype in the PDX model of colorectal cancer and liver metastases. Oncogene. 2018;37:1237-1250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 57] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 263. | Lazzari L, Corti G, Picco G, Isella C, Montone M, Arcella P, Durinikova E, Zanella ER, Novara L, Barbosa F, Cassingena A, Cancelliere C, Medico E, Sartore-Bianchi A, Siena S, Garnett MJ, Bertotti A, Trusolino L, Di Nicolantonio F, Linnebacher M, Bardelli A, Arena S. Patient-Derived Xenografts and Matched Cell Lines Identify Pharmacogenomic Vulnerabilities in Colorectal Cancer. Clin Cancer Res. 2019;25:6243-6259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 264. | Pauli C, Hopkins BD, Prandi D, Shaw R, Fedrizzi T, Sboner A, Sailer V, Augello M, Puca L, Rosati R, McNary TJ, Churakova Y, Cheung C, Triscott J, Pisapia D, Rao R, Mosquera JM, Robinson B, Faltas BM, Emerling BE, Gadi VK, Bernard B, Elemento O, Beltran H, Demichelis F, Kemp CJ, Grandori C, Cantley LC, Rubin MA. Personalized In Vitro and In Vivo Cancer Models to Guide Precision Medicine. Cancer Discov. 2017;7:462-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 675] [Cited by in RCA: 711] [Article Influence: 88.9] [Reference Citation Analysis (0)] |
| 265. | Hidalgo M, Bruckheimer E, Rajeshkumar NV, Garrido-Laguna I, De Oliveira E, Rubio-Viqueira B, Strawn S, Wick MJ, Martell J, Sidransky D. A pilot clinical study of treatment guided by personalized tumorgrafts in patients with advanced cancer. Mol Cancer Ther. 2011;10:1311-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 320] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 266. | Bertotti A, Migliardi G, Galimi F, Sassi F, Torti D, Isella C, Corà D, Di Nicolantonio F, Buscarino M, Petti C, Ribero D, Russolillo N, Muratore A, Massucco P, Pisacane A, Molinaro L, Valtorta E, Sartore-Bianchi A, Risio M, Capussotti L, Gambacorta M, Siena S, Medico E, Sapino A, Marsoni S, Comoglio PM, Bardelli A, Trusolino L. A molecularly annotated platform of patient-derived xenografts ("xenopatients") identifies HER2 as an effective therapeutic target in cetuximab-resistant colorectal cancer. Cancer Discov. 2011;1:508-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 645] [Cited by in RCA: 736] [Article Influence: 52.6] [Reference Citation Analysis (0)] |
| 267. | Migliardi G, Sassi F, Torti D, Galimi F, Zanella ER, Buscarino M, Ribero D, Muratore A, Massucco P, Pisacane A, Risio M, Capussotti L, Marsoni S, Di Nicolantonio F, Bardelli A, Comoglio PM, Trusolino L, Bertotti A. Inhibition of MEK and PI3K/mTOR suppresses tumor growth but does not cause tumor regression in patient-derived xenografts of RAS-mutant colorectal carcinomas. Clin Cancer Res. 2012;18:2515-2525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 160] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 268. | Gao H, Korn JM, Ferretti S, Monahan JE, Wang Y, Singh M, Zhang C, Schnell C, Yang G, Zhang Y, Balbin OA, Barbe S, Cai H, Casey F, Chatterjee S, Chiang DY, Chuai S, Cogan SM, Collins SD, Dammassa E, Ebel N, Embry M, Green J, Kauffmann A, Kowal C, Leary RJ, Lehar J, Liang Y, Loo A, Lorenzana E, Robert McDonald E, McLaughlin ME, Merkin J, Meyer R, Naylor TL, Patawaran M, Reddy A, Röelli C, Ruddy DA, Salangsang F, Santacroce F, Singh AP, Tang Y, Tinetto W, Tobler S, Velazquez R, Venkatesan K, Von Arx F, Wang HQ, Wang Z, Wiesmann M, Wyss D, Xu F, Bitter H, Atadja P, Lees E, Hofmann F, Li E, Keen N, Cozens R, Jensen MR, Pryer NK, Williams JA, Sellers WR. High-throughput screening using patient-derived tumor xenografts to predict clinical trial drug response. Nat Med. 2015;21:1318-1325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 828] [Cited by in RCA: 997] [Article Influence: 99.7] [Reference Citation Analysis (0)] |
| 269. | Witkiewicz AK, Balaji U, Eslinger C, McMillan E, Conway W, Posner B, Mills GB, O'Reilly EM, Knudsen ES. Integrated Patient-Derived Models Delineate Individualized Therapeutic Vulnerabilities of Pancreatic Cancer. Cell Rep. 2016;16:2017-2031. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 270. | Cescon D. Personalized Patient Derived Xenograft (pPDX) Modeling to Test Drug Response in Matching Host (REFLECT). [accessed 2019 Oct 25]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: https://clinicaltrials.gov/ct2/show/record/NCT02732860 ClinicalTrials.gov Identifier: NCT02732860. |
| 271. | Heinemann V. Optimization of Individualized Therapy for CRCs With Secondary RESISTance Towards Anti-EGFR Targeted Therapy Using an Avatar Model. [accessed 2019 Oct 25]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: https://clinicaltrials.gov/ct2/show/NCT03263663 ClinicalTrials.gov Identifier: NCT03263663. |
| 272. | Perea S, Sarno F. Personalised Therapy for Metastatic ADPC Determined by Genetic Testing and Avatar Model Generation (AVATAR). [accessed 2019 Oct 25]. In: ClinicalTrials.gov [Internet]. Bethesda (MD): U.S. National Library of Medicine. Available from: https://clinicaltrials.gov/ct2/show/NCT02795650 ClinicalTrials.gov Identifier: NCT02795650. |
| 273. | Oh BY, Lee WY, Jung S, Hong HK, Nam DH, Park YA, Huh JW, Yun SH, Kim HC, Chun HK, Cho YB. Correlation between tumor engraftment in patient-derived xenograft models and clinical outcomes in colorectal cancer patients. Oncotarget. 2015;6:16059-16068. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 274. | Puig I, Chicote I, Tenbaum SP, Arqués O, Herance JR, Gispert JD, Jimenez J, Landolfi S, Caci K, Allende H, Mendizabal L, Moreno D, Charco R, Espín E, Prat A, Elez ME, Argilés G, Vivancos A, Tabernero J, Rojas S, Palmer HG. A personalized preclinical model to evaluate the metastatic potential of patient-derived colon cancer initiating cells. Clin Cancer Res. 2013;19:6787-6801. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 74] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 275. | Julien S, Merino-Trigo A, Lacroix L, Pocard M, Goéré D, Mariani P, Landron S, Bigot L, Nemati F, Dartigues P, Weiswald LB, Lantuas D, Morgand L, Pham E, Gonin P, Dangles-Marie V, Job B, Dessen P, Bruno A, Pierré A, De Thé H, Soliman H, Nunes M, Lardier G, Calvet L, Demers B, Prévost G, Vrignaud P, Roman-Roman S, Duchamp O, Berthet C. Characterization of a large panel of patient-derived tumor xenografts representing the clinical heterogeneity of human colorectal cancer. Clin Cancer Res. 2012;18:5314-5328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 281] [Article Influence: 21.6] [Reference Citation Analysis (0)] |
| 276. | Collins AT, Lang SH. A systematic review of the validity of patient derived xenograft (PDX) models: the implications for translational research and personalised medicine. PeerJ. 2018;6:e5981. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 277. | Dangles-Marie V, Pocard M, Richon S, Weiswald LB, Assayag F, Saulnier P, Judde JG, Janneau JL, Auger N, Validire P, Dutrillaux B, Praz F, Bellet D, Poupon MF. Establishment of human colon cancer cell lines from fresh tumors versus xenografts: comparison of success rate and cell line features. Cancer Res. 2007;67:398-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 135] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 278. | Prasetyanti PR, van Hooff SR, van Herwaarden T, de Vries N, Kalloe K, Rodermond H, van Leersum R, de Jong JH, Franitza M, Nürnberg P, Todaro M, Stassi G, Medema JP. Capturing colorectal cancer inter-tumor heterogeneity in patient-derived xenograft (PDX) models. Int J Cancer. 2019;144:366-371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 279. | Wetterauer C, Vlajnic T, Schüler J, Gsponer JR, Thalmann GN, Cecchini M, Schneider J, Zellweger T, Pueschel H, Bachmann A, Ruiz C, Dirnhofer S, Bubendorf L, Rentsch CA. Early development of human lymphomas in a prostate cancer xenograft program using triple knock-out immunocompromised mice. Prostate. 2015;75:585-592. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 280. | Zhang L, Liu Y, Wang X, Tang Z, Li S, Hu Y, Zong X, Wu X, Bu Z, Wu A, Li Z, Li Z, Huang X, Jia L, Kang Q, Liu Y, Sutton D, Wang L, Luo L, Ji J. The extent of inflammatory infiltration in primary cancer tissues is associated with lymphomagenesis in immunodeficient mice. Sci Rep. 2015;5:9447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 281. | Bondarenko G, Ugolkov A, Rohan S, Kulesza P, Dubrovskyi O, Gursel D, Mathews J, O'Halloran TV, Wei JJ, Mazar AP. Patient-Derived Tumor Xenografts Are Susceptible to Formation of Human Lymphocytic Tumors. Neoplasia. 2015;17:735-741. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 79] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 282. | Chen K, Ahmed S, Adeyi O, Dick JE, Ghanekar A. Human solid tumor xenografts in immunodeficient mice are vulnerable to lymphomagenesis associated with Epstein-Barr virus. PLoS One. 2012;7:e39294. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 63] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 283. | Taurozzi AJ, Beekharry R, Wantoch M, Labarthe MC, Walker HF, Seed RI, Simms M, Rodrigues G, Bradford J, van der Horst G, van der Pluijm G, Collins AT. Spontaneous development of Epstein-Barr Virus associated human lymphomas in a prostate cancer xenograft program. PLoS One. 2017;12:e0188228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 284. | John T, Yanagawa N, Kohler D, Craddock KJ, Bandarchi-Chamkhaleh B, Pintilie M, Sykes J, To C, Li M, Panchal D, Chen W, Shepherd FA, Tsao MS. Characterization of lymphomas developing in immunodeficient mice implanted with primary human non-small cell lung cancer. J Thorac Oncol. 2012;7:1101-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 285. | McCormick KH, Giovanella BC, Klein G, Nilsson K, Stehlin JS. Diploid human lymphoblastoid and Burkitt lymphoma cell lines: susceptibility to murine NK cells and heterotransplantation to nude mice. Int J Cancer. 1981;28:455-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 286. | Butler KA, Hou X, Becker MA, Zanfagnin V, Enderica-Gonzalez S, Visscher D, Kalli KR, Tienchaianada P, Haluska P, Weroha SJ. Prevention of Human Lymphoproliferative Tumor Formation in Ovarian Cancer Patient-Derived Xenografts. Neoplasia. 2017;19:628-636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 49] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 287. | Snipes RL. Anatomy of the cecum of the laboratory mouse and rat. Anat Embryol (Berl). 1981;162:455-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 34] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 288. | Bresalier RS, Raper SE, Hujanen ES, Kim YS. A new animal model for human colon cancer metastasis. Int J Cancer. 1987;39:625-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 79] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 289. | Fu XY, Besterman JM, Monosov A, Hoffman RM. Models of human metastatic colon cancer in nude mice orthotopically constructed by using histologically intact patient specimens. Proc Natl Acad Sci USA. 1991;88:9345-9349. [PubMed] |
| 290. | Rajput A, Agarwal E, Leiphrakpam P, Brattain MG, Chowdhury S. Establishment and Validation of an Orthotopic Metastatic Mouse Model of Colorectal Cancer. ISRN Hepatol. 2013;2013:206875. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 291. | Chow AK, Cheng NS, Lam CS, Ng L, Wong SK, Wan TM, Man JH, Cheung AH, Yau TC, Poon JT, Law WL, Pang RW. Preclinical analysis of the anti-tumor and anti-metastatic effects of Raf265 on colon cancer cells and CD26(+) cancer stem cells in colorectal carcinoma. Mol Cancer. 2015;14:80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 292. | Abou-Elkacem L, Arns S, Brix G, Gremse F, Zopf D, Kiessling F, Lederle W. Regorafenib inhibits growth, angiogenesis, and metastasis in a highly aggressive, orthotopic colon cancer model. Mol Cancer Ther. 2013;12:1322-1331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 213] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 293. | Zhao L, Liu L, Wang S, Zhang YF, Yu L, Ding YQ. Differential proteomic analysis of human colorectal carcinoma cell lines metastasis-associated proteins. J Cancer Res Clin Oncol. 2007;133:771-782. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 294. | Chunhua L, Donglan L, Xiuqiong F, Lihua Z, Qin F, Yawei L, Liang Z, Ge W, Linlin J, Ping Z, Kun L, Xuegang S. Apigenin up-regulates transgelin and inhibits invasion and migration of colorectal cancer through decreased phosphorylation of AKT. J Nutr Biochem. 2013;24:1766-1775. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 95] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 295. | Wang J, Rajput A, Kan JL, Rose R, Liu XQ, Kuropatwinski K, Hauser J, Beko A, Dominquez I, Sharratt EA, Brattain L, Levea C, Sun FL, Keane DM, Gibson NW, Brattain MG. Knockdown of Ron kinase inhibits mutant phosphatidylinositol 3-kinase and reduces metastasis in human colon carcinoma. J Biol Chem. 2009;284:10912-10922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 296. | Lin W, Zhuang Q, Zheng L, Cao Z, Shen A, Li Q, Fu C, Feng J, Peng J. Pien Tze Huang inhibits liver metastasis by targeting TGF-β signaling in an orthotopic model of colorectal cancer. Oncol Rep. 2015;33:1922-1928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 297. | Kochall S, Thepkaysone ML, García SA, Betzler AM, Weitz J, Reissfelder C, Schölch S. Isolation of Circulating Tumor Cells in an Orthotopic Mouse Model of Colorectal Cancer. J Vis Exp. 2017;(125). [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 298. | Yang JL, Seetoo DQ, Wang Y, Ranson M, Berney CR, Ham JM, Russell PJ, Crowe PJ. Urokinase-type plasminogen activator and its receptor in colorectal cancer: Independent prognostic factors of metastasis and cancer-specific survival and potential therapeutic targets. Int J Cancer. 2000;89:431–439. [DOI] [Full Text] |
| 299. | Céspedes MV, Espina C, García-Cabezas MA, Trias M, Boluda A, Gómez del Pulgar MT, Sancho FJ, Nistal M, Lacal JC, Mangues R. Orthotopic microinjection of human colon cancer cells in nude mice induces tumor foci in all clinically relevant metastatic sites. Am J Pathol. 2007;170:1077-1085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 135] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 300. | Klose J, Eissele J, Volz C, Schmitt S, Ritter A, Ying S, Schmidt T, Heger U, Schneider M, Ulrich A. Salinomycin inhibits metastatic colorectal cancer growth and interferes with Wnt/β-catenin signaling in CD133+ human colorectal cancer cells. BMC Cancer. 2016;16:896. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 301. | Alamo P, Gallardo A, Pavón MA, Casanova I, Trias M, Mangues MA, Vázquez E, Villaverde A, Mangues R, Céspedes MV. Subcutaneous preconditioning increases invasion and metastatic dissemination in mouse colorectal cancer models. Dis Model Mech. 2014;7:387-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 302. | Schulz P, Dierkes C, Wiedenmann B, Grötzinger C. Near-Infrared Confocal Laser Endomicroscopy Detects Colorectal Cancer via an Integrin αvβ3 Optical Probe. Mol Imaging Bio. 2015;17:450–460. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 303. | Künzli BM, Bernlochner MI, Rath S, Käser S, Csizmadia E, Enjyoji K, Cowan P, d'Apice A, Dwyer K, Rosenberg R, Perren A, Friess H, Maurer CA, Robson SC. Impact of CD39 and purinergic signalling on the growth and metastasis of colorectal cancer. Purinergic Signal. 2011;7:231-241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 112] [Cited by in RCA: 108] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 304. | Lee WY, Hong HK, Ham SK, Kim CI, Cho YB. Comparison of colorectal cancer in differentially established liver metastasis models. Anticancer Res. 2014;34:3321-3328. [PubMed] |
| 305. | Sasaki H, Miura K, Horii A, Kaneko N, Fujibuchi W, Kiseleva L, Gu Z, Murata Y, Karasawa H, Mizoi T, Kobayashi T, Kinouchi M, Ohnuma S, Yazaki N, Unno M, Sasaki I. Orthotopic implantation mouse model and cDNA microarray analysis indicates several genes potentially involved in lymph node metastasis of colorectal cancer. Cancer Sci. 2008;99:711-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 306. | Tang W, Zhu Y, Gao J, Fu J, Liu C, Liu Y, Song C, Zhu S, Leng Y, Wang G, Chen W, Du P, Huang S, Zhou X, Kang J, Cui L. MicroRNA-29a promotes colorectal cancer metastasis by regulating matrix metalloproteinase 2 and E-cadherin via KLF4. Br J Cancer. 2014;110:450-458. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 148] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 307. | Alamo P, Gallardo A, Di Nicolantonio F, Pavón MA, Casanova I, Trias M, Mangues MA, Lopez-Pousa A, Villaverde A, Vázquez E, Bardelli A, Céspedes MV, Mangues R. Higher metastatic efficiency of KRas G12V than KRas G13D in a colorectal cancer model. FASEB J. 2015;29:464-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 308. | Chen HN, Yuan K, Xie N, Wang K, Huang Z, Chen Y, Dou Q, Wu M, Nice EC, Zhou ZG, Huang C. PDLIM1 Stabilizes the E-Cadherin/β-Catenin Complex to Prevent Epithelial-Mesenchymal Transition and Metastatic Potential of Colorectal Cancer Cells. Cancer Res. 2016;76:1122-1134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 95] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 309. | Meunier K, Ferron M, Calmel C, Fléjou JF, Pocard M, Praz F. Impact of MLH1 expression on tumor evolution after curative surgical tumor resection in a murine orthotopic xenograft model for human MSI colon cancer. Genes Chromosomes Cancer. 2017;56:681-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 310. | Xu H, Zhang Y, Peña MM, Pirisi L, Creek KE. Six1 promotes colorectal cancer growth and metastasis by stimulating angiogenesis and recruiting tumor-associated macrophages. Carcinogenesis. 2017;38:281-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 62] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 311. | Paulson B, Kim IH, Namgoong JM, Kim YG, Lee S, Moon Y, Shin DM, Choo MS, Kim JK. Longitudinal micro-endoscopic monitoring of high-success intramucosal xenografts for mouse models of colorectal cancer. Int J Med Sci. 2019;16:1453-1460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 312. | Enquist IB, Good Z, Jubb AM, Fuh G, Wang X, Junttila MR, Jackson EL, Leong KG. Lymph node-independent liver metastasis in a model of metastatic colorectal cancer. Nat Commun. 2014;5:3530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 313. | Rapic S, Vangestel C, Verhaeghe J, Van den Wyngaert T, Hinz R, Verhoye M, Pauwels P, Staelens S, Stroobants S. Characterization of an Orthotopic Colorectal Cancer Mouse Model and Its Feasibility for Accurate Quantification in Positron Emission Tomography. Mol Imaging Biol. 2017;19:762-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 314. | Mira A, Morello V, Céspedes MV, Perera T, Comoglio PM, Mangues R, Michieli P. Stroma-derived HGF drives metabolic adaptation of colorectal cancer to angiogenesis inhibitors. Oncotarget. 2017;8:38193-38213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 315. | Afik R, Zigmond E, Vugman M, Klepfish M, Shimshoni E, Pasmanik-Chor M, Shenoy A, Bassat E, Halpern Z, Geiger T, Sagi I, Varol C. Tumor macrophages are pivotal constructors of tumor collagenous matrix. J Exp Med. 2016;213:2315-2331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 187] [Cited by in RCA: 265] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 316. | Hu CT, Guo LL, Feng N, Zhang L, Zhou N, Ma LL, Shen L, Tong GH, Yan QW, Zhu SJ, Bian XW, Lai MD, Deng YJ, Ding YQ. MIF, secreted by human hepatic sinusoidal endothelial cells, promotes chemotaxis and outgrowth of colorectal cancer in liver prometastasis. Oncotarget. 2015;6:22410-22423. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 317. | Basilico C, Hultberg A, Blanchetot C, de Jonge N, Festjens E, Hanssens V, Osepa SI, De Boeck G, Mira A, Cazzanti M, Morello V, Dreier T, Saunders M, de Haard H, Michieli P. Four individually druggable MET hotspots mediate HGF-driven tumor progression. J Clin Invest. 2014;124:3172-3186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 318. | Margolin DA, Myers T, Zhang X, Bertoni DM, Reuter BA, Obokhare I, Borgovan T, Grimes C, Green H, Driscoll T, Lee CG, Davis NK, Li L. The critical roles of tumor-initiating cells and the lymph node stromal microenvironment in human colorectal cancer extranodal metastasis using a unique humanized orthotopic mouse model. FASEB J. 2015;29:3571-3581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 319. | Devaud C, Rousseau B, Netzer S, Pitard V, Paroissin C, Khairallah C, Costet P, Moreau JF, Couillaud F, Dechanet-Merville J, Capone M. Anti-metastatic potential of human Vδ1(+) γδ T cells in an orthotopic mouse xenograft model of colon carcinoma. Cancer Immunol Immunother. 2013;62:1199-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 320. | Schölch S, García SA, Iwata N, Niemietz T, Betzler AM, Nanduri LK, Bork U, Kahlert C, Thepkaysone ML, Swiersy A, Büchler MW, Reissfelder C, Weitz J, Rahbari NN. Circulating tumor cells exhibit stem cell characteristics in an orthotopic mouse model of colorectal cancer. Oncotarget. 2016;7:27232-27242. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 37] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 321. | Kashtan H, Rabau M, Mullen JB, Wong AH, Roder JC, Shpitz B, Stern HS, Gallinger S. Intra-rectal injection of tumour cells: a novel animal model of rectal cancer. Surg Oncol. 1992;1:251-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 322. | Donigan M, Norcross LS, Aversa J, Colon J, Smith J, Madero-Visbal R, Li S, McCollum N, Ferrara A, Gallagher JT, Baker CH. Novel murine model for colon cancer: non-operative trans-anal rectal injection. J Surg Res. 2009;154:299-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 323. | Cohen G, Lecht S, Arien-Zakay H, Ettinger K, Amsalem O, Oron-Herman M, Yavin E, Prus D, Benita S, Nissan A, Lazarovici P. Bio-imaging of colorectal cancer models using near infrared labeled epidermal growth factor. PLoS One. 2012;7:e48803. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 324. | Kim YI, Jeong S, Jung KO, Song MG, Lee CH, Chung SJ, Park JY, Cha MG, Lee SG, Jun BH, Lee YS, Hwang DW, Youn H, Kang KW, Lee YS, Jeong DH, Lee DS. Simultaneous Detection of EGFR and VEGF in Colorectal Cancer using Fluorescence-Raman Endoscopy. Sci Rep. 2017;7:1035. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 325. | Zigmond E, Halpern Z, Elinav E, Brazowski E, Jung S, Varol C. Utilization of murine colonoscopy for orthotopic implantation of colorectal cancer. PLoS One. 2011;6:e28858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 326. | Zaytseva YY, Elliott VA, Rychahou P, Mustain WC, Kim JT, Valentino J, Gao T, O'Connor KL, Neltner JM, Lee EY, Weiss HL, Evers BM. Cancer cell-associated fatty acid synthase activates endothelial cells and promotes angiogenesis in colorectal cancer. Carcinogenesis. 2014;35:1341-1351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 84] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 327. | Bettenworth D, Mücke MM, Schwegmann K, Faust A, Poremba C, Schäfers M, Domagk D, Lenz P. Endoscopy-guided orthotopic implantation of colorectal cancer cells results in metastatic colorectal cancer in mice. Clin Exp Metastasis. 2016;33:551-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 328. | Kishimoto H, Momiyama M, Aki R, Kimura H, Suetsugu A, Bouvet M, Fujiwara T, Hoffman RM. Development of a clinically-precise mouse model of rectal cancer. PLoS One. 2013;8:e79453. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 329. | Hite N, Klinger A, Hellmers L, Maresh GA, Miller PE, Zhang X, Li L, Margolin DA. An Optimal Orthotopic Mouse Model for Human Colorectal Cancer Primary Tumor Growth and Spontaneous Metastasis. Dis Colon Rectum. 2018;61:698-705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 330. | Prasad S, Yadav VR, Sung B, Reuter S, Kannappan R, Deorukhkar A, Diagaradjane P, Wei C, Baladandayuthapani V, Krishnan S, Guha S, Aggarwal BB. Ursolic acid inhibits growth and metastasis of human colorectal cancer in an orthotopic nude mouse model by targeting multiple cell signaling pathways: chemosensitization with capecitabine. Clin Cancer Res. 2012;18:4942-4953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 130] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 331. | Wang J, Chen C, Wang S, Zhang Y, Yin P, Gao Z, Xu J, Feng D, Zuo Q, Zhao R, Chen T. Bufalin Inhibits HCT116 Colon Cancer Cells and Its Orthotopic Xenograft Tumor in Mice Model through Genes Related to Apoptotic and PTEN/AKT Pathways. Gastroenterol Res Pract. 2015;2015:457193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 332. | Bhome R, Goh RW, Bullock MD, Pillar N, Thirdborough SM, Mellone M, Mirnezami R, Galea D, Veselkov K, Gu Q, Underwood TJ, Primrose JN, De Wever O, Shomron N, Sayan AE, Mirnezami AH. Exosomal microRNAs derived from colorectal cancer-associated fibroblasts: role in driving cancer progression. Aging (Albany NY). 2017;9:2666-2694. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 120] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 333. | Tan X, Zhang Z, Yao H, Shen L. Tim-4 promotes the growth of colorectal cancer by activating angiogenesis and recruiting tumor-associated macrophages via the PI3K/AKT/mTOR signaling pathway. Cancer Lett. 2018;436:119-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 64] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 334. | Mizukoshi K, Okazawa Y, Haeno H, Koyama Y, Sulidan K, Komiyama H, Saeki H, Ohtsuji N, Ito Y, Kojima Y, Goto M, Habu S, Hino O, Sakamoto K, Orimo A. Metastatic seeding of human colon cancer cell clusters expressing the hybrid epithelial/mesenchymal state. Int J Cancer. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 335. | Russell WMS, Burch RL. The principles of humane experimental technique. London: Methuen&Co. Ltd., 1959. |
| 336. | Wege AK, Ernst W, Eckl J, Frankenberger B, Vollmann-Zwerenz A, Männel DN, Ortmann O, Kroemer A, Brockhoff G. Humanized tumor mice--a new model to study and manipulate the immune response in advanced cancer therapy. Int J Cancer. 2011;129:2194-2206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 77] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 337. | Choi Y, Lee S, Kim K, Kim SH, Chung YJ, Lee C. Studying cancer immunotherapy using patient-derived xenografts (PDXs) in humanized mice. Exp Mol Med. 2018;50:99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 75] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 338. | Bird GA, Polsky A, Estes P, Hanlon T, Hamilton H, Morton JJ, Gutman J, Jimeno A, Turner BC, Refaeli Y. Expansion of human and murine hematopoietic stem and progenitor cells ex vivo without genetic modification using MYC and Bcl-2 fusion proteins. PLoS One. 2014;9:e105525. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 339. | Morton JJ, Bird G, Keysar SB, Astling DP, Lyons TR, Anderson RT, Glogowska MJ, Estes P, Eagles JR, Le PN, Gan G, McGettigan B, Fernandez P, Padilla-Just N, Varella-Garcia M, Song JI, Bowles DW, Schedin P, Tan AC, Roop DR, Wang XJ, Refaeli Y, Jimeno A. XactMice: humanizing mouse bone marrow enables microenvironment reconstitution in a patient-derived xenograft model of head and neck cancer. Oncogene. 2016;35:290-300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 96] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 340. | McIntosh BE, Brown ME, Duffin BM, Maufort JP, Vereide DT, Slukvin II, Thomson JA. Nonirradiated NOD,B6.SCID Il2rγ-/- Kit(W41/W41) (NBSGW) mice support multilineage engraftment of human hematopoietic cells. Stem Cell Reports. 2015;4:171-180. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 181] [Article Influence: 18.1] [Reference Citation Analysis (0)] |
| 341. | Jespersen H, Lindberg MF, Donia M, Söderberg EMV, Andersen R, Keller U, Ny L, Svane IM, Nilsson LM, Nilsson JA. Clinical responses to adoptive T-cell transfer can be modeled in an autologous immune-humanized mouse model. Nat Commun. 2017;8:707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 117] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 342. | Jangalwe S, Shultz LD, Mathew A, Brehm MA. Improved B cell development in humanized NOD-scid IL2Rγnull mice transgenically expressing human stem cell factor, granulocyte-macrophage colony-stimulating factor and interleukin-3. Immun Inflamm Dis. 2016;4:427-440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 95] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 343. | Herndler-Brandstetter D, Shan L, Yao Y, Stecher C, Plajer V, Lietzenmayer M, Strowig T, de Zoete MR, Palm NW, Chen J, Blish CA, Frleta D, Gurer C, Macdonald LE, Murphy AJ, Yancopoulos GD, Montgomery RR, Flavell RA. Humanized mouse model supports development, function, and tissue residency of human natural killer cells. Proc Natl Acad Sci USA. 2017;114:E9626-E9634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 130] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 344. | Capasso A, Lang J, Pitts TM, Jordan KR, Lieu CH, Davis SL, Diamond JR, Kopetz S, Barbee J, Peterson J, Freed BM, Yacob BW, Bagby SM, Messersmith WA, Slansky JE, Pelanda R, Eckhardt SG. Characterization of immune responses to anti-PD-1 mono and combination immunotherapy in hematopoietic humanized mice implanted with tumor xenografts. J Immunother Cancer. 2019;7:37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 128] [Article Influence: 21.3] [Reference Citation Analysis (0)] |
| 345. | Overman MJ, Lonardi S, Wong KYM, Lenz HJ, Gelsomino F, Aglietta M, Morse MA, Van Cutsem E, McDermott R, Hill A, Sawyer MB, Hendlisz A, Neyns B, Svrcek M, Moss RA, Ledeine JM, Cao ZA, Kamble S, Kopetz S, André T. Durable Clinical Benefit With Nivolumab Plus Ipilimumab in DNA Mismatch Repair-Deficient/Microsatellite Instability-High Metastatic Colorectal Cancer. J Clin Oncol. 2018;36:773-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1013] [Cited by in RCA: 1474] [Article Influence: 210.6] [Reference Citation Analysis (0)] |
| 346. | Barretina J, Caponigro G, Stransky N, Venkatesan K, Margolin AA, Kim S, Wilson CJ, Lehár J, Kryukov GV, Sonkin D, Reddy A, Liu M, Murray L, Berger MF, Monahan JE, Morais P, Meltzer J, Korejwa A, Jané-Valbuena J, Mapa FA, Thibault J, Bric-Furlong E, Raman P, Shipway A, Engels IH, Cheng J, Yu GK, Yu J, Aspesi P, de Silva M, Jagtap K, Jones MD, Wang L, Hatton C, Palescandolo E, Gupta S, Mahan S, Sougnez C, Onofrio RC, Liefeld T, MacConaill L, Winckler W, Reich M, Li N, Mesirov JP, Gabriel SB, Getz G, Ardlie K, Chan V, Myer VE, Weber BL, Porter J, Warmuth M, Finan P, Harris JL, Meyerson M, Golub TR, Morrissey MP, Sellers WR, Schlegel R, Garraway LA. The Cancer Cell Line Encyclopedia enables predictive modelling of anticancer drug sensitivity. Nature. 2012;483:603-607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5947] [Cited by in RCA: 5818] [Article Influence: 447.5] [Reference Citation Analysis (0)] |
| 347. | Krbal L, Soukup J, Stanislav J, Hanusova V. Derivation and basic characterization of colorectal carcinoma primary cell lines. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2017;161:360-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 348. | Bolck HA, Pauli C, Göbel E, Mühlbauer K, Dettwiler S, Moch H, Schraml P. Cancer Sample Biobanking at the Next Level: Combining Tissue With Living Cell Repositories to Promote Precision Medicine. Front Cell Dev Biol. 2019;7:246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 349. | Kang Y, Zhang R, Suzuki R, Li SQ, Roife D, Truty MJ, Chatterjee D, Thomas RM, Cardwell J, Wang Y, Wang H, Katz MH, Fleming JB. Two-dimensional culture of human pancreatic adenocarcinoma cells results in an irreversible transition from epithelial to mesenchymal phenotype. Lab Invest. 2015;95:207-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 350. | Hickman JA, Graeser R, de Hoogt R, Vidic S, Brito C, Gutekunst M, van der Kuip H; IMI PREDECT Consortium. Three-dimensional models of cancer for pharmacology and cancer cell biology: capturing tumor complexity in vitro/ex vivo. Biotechnol J. 2014;9:1115-1128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 270] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 351. | Luca AC, Mersch S, Deenen R, Schmidt S, Messner I, Schäfer KL, Baldus SE, Huckenbeck W, Piekorz RP, Knoefel WT, Krieg A, Stoecklein NH. Impact of the 3D microenvironment on phenotype, gene expression, and EGFR inhibition of colorectal cancer cell lines. PLoS One. 2013;8:e59689. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 212] [Cited by in RCA: 250] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 352. | van Tienderen GS, Groot Koerkamp B, IJzermans JNM, van der Laan LJW, Verstegen MMA. Recreating Tumour Complexity in a Dish: Organoid Models to Study Liver Cancer Cells and their Extracellular Environment. Cancers (Basel). 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 353. | van de Wetering M, Francies HE, Francis JM, Bounova G, Iorio F, Pronk A, van Houdt W, van Gorp J, Taylor-Weiner A, Kester L, McLaren-Douglas A, Blokker J, Jaksani S, Bartfeld S, Volckman R, van Sluis P, Li VS, Seepo S, Sekhar Pedamallu C, Cibulskis K, Carter SL, McKenna A, Lawrence MS, Lichtenstein L, Stewart C, Koster J, Versteeg R, van Oudenaarden A, Saez-Rodriguez J, Vries RG, Getz G, Wessels L, Stratton MR, McDermott U, Meyerson M, Garnett MJ, Clevers H. Prospective derivation of a living organoid biobank of colorectal cancer patients. Cell. 2015;161:933-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1313] [Cited by in RCA: 1734] [Article Influence: 192.7] [Reference Citation Analysis (0)] |
| 354. | Vlachogiannis G, Hedayat S, Vatsiou A, Jamin Y, Fernández-Mateos J, Khan K, Lampis A, Eason K, Huntingford I, Burke R, Rata M, Koh DM, Tunariu N, Collins D, Hulkki-Wilson S, Ragulan C, Spiteri I, Moorcraft SY, Chau I, Rao S, Watkins D, Fotiadis N, Bali M, Darvish-Damavandi M, Lote H, Eltahir Z, Smyth EC, Begum R, Clarke PA, Hahne JC, Dowsett M, de Bono J, Workman P, Sadanandam A, Fassan M, Sansom OJ, Eccles S, Starling N, Braconi C, Sottoriva A, Robinson SP, Cunningham D, Valeri N. Patient-derived organoids model treatment response of metastatic gastrointestinal cancers. Science. 2018;359:920-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1436] [Cited by in RCA: 1328] [Article Influence: 189.7] [Reference Citation Analysis (0)] |
| 355. | Tiriac H, Belleau P, Engle DD, Plenker D, Deschênes A, Somerville TDD, Froeling FEM, Burkhart RA, Denroche RE, Jang GH, Miyabayashi K, Young CM, Patel H, Ma M, LaComb JF, Palmaira RLD, Javed AA, Huynh JC, Johnson M, Arora K, Robine N, Shah M, Sanghvi R, Goetz AB, Lowder CY, Martello L, Driehuis E, LeComte N, Askan G, Iacobuzio-Donahue CA, Clevers H, Wood LD, Hruban RH, Thompson E, Aguirre AJ, Wolpin BM, Sasson A, Kim J, Wu M, Bucobo JC, Allen P, Sejpal DV, Nealon W, Sullivan JD, Winter JM, Gimotty PA, Grem JL, DiMaio DJ, Buscaglia JM, Grandgenett PM, Brody JR, Hollingsworth MA, O'Kane GM, Notta F, Kim E, Crawford JM, Devoe C, Ocean A, Wolfgang CL, Yu KH, Li E, Vakoc CR, Hubert B, Fischer SE, Wilson JM, Moffitt R, Knox J, Krasnitz A, Gallinger S, Tuveson DA. Organoid Profiling Identifies Common Responders to Chemotherapy in Pancreatic Cancer. Cancer Discov. 2018;8:1112-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 457] [Cited by in RCA: 739] [Article Influence: 105.6] [Reference Citation Analysis (0)] |
| 356. | Yan HHN, Siu HC, Law S, Ho SL, Yue SSK, Tsui WY, Chan D, Chan AS, Ma S, Lam KO, Bartfeld S, Man AHY, Lee BCH, Chan ASY, Wong JWH, Cheng PSW, Chan AKW, Zhang J, Shi J, Fan X, Kwong DLW, Mak TW, Yuen ST, Clevers H, Leung SY. A Comprehensive Human Gastric Cancer Organoid Biobank Captures Tumor Subtype Heterogeneity and Enables Therapeutic Screening. Cell Stem Cell. 2018;23:882-897.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 486] [Article Influence: 69.4] [Reference Citation Analysis (0)] |
| 357. | Lee SH, Hong JH, Park HK, Park JS, Kim BK, Lee JY, Jeong JY, Yoon GS, Inoue M, Choi GS, Lee IK. Colorectal cancer-derived tumor spheroids retain the characteristics of original tumors. Cancer Lett. 2015;367:34-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 47] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 358. | Sato T, Vries RG, Snippert HJ, van de Wetering M, Barker N, Stange DE, van Es JH, Abo A, Kujala P, Peters PJ, Clevers H. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature. 2009;459:262-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4394] [Cited by in RCA: 5172] [Article Influence: 323.3] [Reference Citation Analysis (0)] |
| 359. | Drost J, van Jaarsveld RH, Ponsioen B, Zimberlin C, van Boxtel R, Buijs A, Sachs N, Overmeer RM, Offerhaus GJ, Begthel H, Korving J, van de Wetering M, Schwank G, Logtenberg M, Cuppen E, Snippert HJ, Medema JP, Kops GJ, Clevers H. Sequential cancer mutations in cultured human intestinal stem cells. Nature. 2015;521:43-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 677] [Cited by in RCA: 796] [Article Influence: 79.6] [Reference Citation Analysis (0)] |
| 360. | Fumagalli A, Drost J, Suijkerbuijk SJ, van Boxtel R, de Ligt J, Offerhaus GJ, Begthel H, Beerling E, Tan EH, Sansom OJ, Cuppen E, Clevers H, van Rheenen J. Genetic dissection of colorectal cancer progression by orthotopic transplantation of engineered cancer organoids. Proc Natl Acad Sci USA. 2017;114:E2357-E2364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 191] [Article Influence: 23.9] [Reference Citation Analysis (0)] |
| 361. | Gao D, Vela I, Sboner A, Iaquinta PJ, Karthaus WR, Gopalan A, Dowling C, Wanjala JN, Undvall EA, Arora VK, Wongvipat J, Kossai M, Ramazanoglu S, Barboza LP, Di W, Cao Z, Zhang QF, Sirota I, Ran L, MacDonald TY, Beltran H, Mosquera JM, Touijer KA, Scardino PT, Laudone VP, Curtis KR, Rathkopf DE, Morris MJ, Danila DC, Slovin SF, Solomon SB, Eastham JA, Chi P, Carver B, Rubin MA, Scher HI, Clevers H, Sawyers CL, Chen Y. Organoid cultures derived from patients with advanced prostate cancer. Cell. 2014;159:176-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 882] [Cited by in RCA: 1151] [Article Influence: 104.6] [Reference Citation Analysis (0)] |
| 362. | Agnoletto C, Corrà F, Minotti L, Baldassari F, Crudele F, Cook WJJ, Di Leva G, d'Adamo AP, Gasparini P, Volinia S. Heterogeneity in Circulating Tumor Cells: The Relevance of the Stem-Cell Subset. Cancers (Basel). 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 113] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 363. | Aleman J, Skardal A. A multi-site metastasis-on-a-chip microphysiological system for assessing metastatic preference of cancer cells. Biotechnol Bioeng. 2019;116:936-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 102] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 364. | Miller PG, Shuler ML. Design and demonstration of a pumpless 14 compartment microphysiological system. Biotechnol Bioeng. 2016;113:2213-2227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 159] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 365. | Guinney J, Dienstmann R, Wang X, de Reyniès A, Schlicker A, Soneson C, Marisa L, Roepman P, Nyamundanda G, Angelino P, Bot BM, Morris JS, Simon IM, Gerster S, Fessler E, De Sousa E Melo F, Missiaglia E, Ramay H, Barras D, Homicsko K, Maru D, Manyam GC, Broom B, Boige V, Perez-Villamil B, Laderas T, Salazar R, Gray JW, Hanahan D, Tabernero J, Bernards R, Friend SH, Laurent-Puig P, Medema JP, Sadanandam A, Wessels L, Delorenzi M, Kopetz S, Vermeulen L, Tejpar S. The consensus molecular subtypes of colorectal cancer. Nat Med. 2015;21:1350-1356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3408] [Cited by in RCA: 3555] [Article Influence: 355.5] [Reference Citation Analysis (0)] |
| 366. | Mooi JK, Wirapati P, Asher R, Lee CK, Savas P, Price TJ, Townsend A, Hardingham J, Buchanan D, Williams D, Tejpar S, Mariadason JM, Tebbutt NC. The prognostic impact of consensus molecular subtypes (CMS) and its predictive effects for bevacizumab benefit in metastatic colorectal cancer: molecular analysis of the AGITG MAX clinical trial. Ann Oncol. 2018;29:2240-2246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 111] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 367. | Jean-Quartier C, Jeanquartier F, Jurisica I, Holzinger A. In silico cancer research towards 3R. BMC Cancer. 2018;18:408. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 82] [Cited by in RCA: 69] [Article Influence: 9.9] [Reference Citation Analysis (0)] |
| 368. | Christopher R, Dhiman A, Fox J, Gendelman R, Haberitcher T, Kagle D, Spizz G, Khalil IG, Hill C. Data-driven computer simulation of human cancer cell. Ann N Y Acad Sci. 2004;1020:132-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 53] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 369. | Uhlen M, Zhang C, Lee S, Sjöstedt E, Fagerberg L, Bidkhori G, Benfeitas R, Arif M, Liu Z, Edfors F, Sanli K, von Feilitzen K, Oksvold P, Lundberg E, Hober S, Nilsson P, Mattsson J, Schwenk JM, Brunnström H, Glimelius B, Sjöblom T, Edqvist PH, Djureinovic D, Micke P, Lindskog C, Mardinoglu A, Ponten F. A pathology atlas of the human cancer transcriptome. Science. 2017;357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1721] [Cited by in RCA: 2351] [Article Influence: 293.9] [Reference Citation Analysis (0)] |
| 370. | Farshidfar F, Weljie AM, Kopciuk KA, Hilsden R, McGregor SE, Buie WD, MacLean A, Vogel HJ, Bathe OF. A validated metabolomic signature for colorectal cancer: exploration of the clinical value of metabolomics. Br J Cancer. 2016;115:848-857. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 114] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 371. | Porta-Pardo E, Garcia-Alonso L, Hrabe T, Dopazo J, Godzik A. A Pan-Cancer Catalogue of Cancer Driver Protein Interaction Interfaces. PLoS Comput Biol. 2015;11:e1004518. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 91] [Cited by in RCA: 94] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 372. | Subramanian A, Narayan R, Corsello SM, Peck DD, Natoli TE, Lu X, Gould J, Davis JF, Tubelli AA, Asiedu JK, Lahr DL, Hirschman JE, Liu Z, Donahue M, Julian B, Khan M, Wadden D, Smith IC, Lam D, Liberzon A, Toder C, Bagul M, Orzechowski M, Enache OM, Piccioni F, Johnson SA, Lyons NJ, Berger AH, Shamji AF, Brooks AN, Vrcic A, Flynn C, Rosains J, Takeda DY, Hu R, Davison D, Lamb J, Ardlie K, Hogstrom L, Greenside P, Gray NS, Clemons PA, Silver S, Wu X, Zhao WN, Read-Button W, Wu X, Haggarty SJ, Ronco LV, Boehm JS, Schreiber SL, Doench JG, Bittker JA, Root DE, Wong B, Golub TR. A Next Generation Connectivity Map: L1000 Platform and the First 1,000,000 Profiles. Cell. 2017;171:1437-1452.e17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1427] [Cited by in RCA: 2130] [Article Influence: 266.3] [Reference Citation Analysis (0)] |
| 373. | Kim YA, Cho DY, Przytycka TM. Understanding Genotype-Phenotype Effects in Cancer via Network Approaches. PLoS Comput Biol. 2016;12:e1004747. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 42] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 374. | Aoki K, Tamai Y, Horiike S, Oshima M, Taketo MM. Colonic polyposis caused by mTOR-mediated chromosomal instability in Apc+/Delta716 Cdx2+/- compound mutant mice. Nat Genet. 2003;35:323-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 188] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 375. | Rao CV, Yang YM, Swamy MV, Liu T, Fang Y, Mahmood R, Jhanwar-Uniyal M, Dai W. Colonic tumorigenesis in BubR1+/-ApcMin/+ compound mutant mice is linked to premature separation of sister chromatids and enhanced genomic instability. Proc Natl Acad Sci USA. 2005;102:4365-4370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 135] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 376. | Hahn MM, Vreede L, Bemelmans SA, van der Looij E, van Kessel AG, Schackert HK, Ligtenberg MJ, Hoogerbrugge N, Kuiper RP, de Voer RM. Prevalence of germline mutations in the spindle assembly checkpoint gene BUB1B in individuals with early-onset colorectal cancer. Genes Chromosomes Cancer. 2016;55:855-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 377. | Batlle E, Bacani J, Begthel H, Jonkheer S, Gregorieff A, van de Born M, Malats N, Sancho E, Boon E, Pawson T, Gallinger S, Pals S, Clevers H. EphB receptor activity suppresses colorectal cancer progression. Nature. 2005;435:1126-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 303] [Cited by in RCA: 319] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 378. | Paul Olson TJ, Hadac JN, Sievers CK, Leystra AA, Deming DA, Zahm CD, Albrecht DM, Nomura A, Nettekoven LA, Plesh LK, Clipson L, Sullivan R, Newton MA, Schelman WR, Halberg RB. Dynamic tumor growth patterns in a novel murine model of colorectal cancer. Cancer Prev Res (Phila). 2014;7:105-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 379. | Suzui M, Okuno M, Tanaka T, Nakagama H, Moriwaki H. Enhanced colon carcinogenesis induced by azoxymethane in min mice occurs via a mechanism independent of beta-catenin mutation. Cancer Lett. 2002;183:31-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 380. | Møllersen L, Vikse R, Andreassen A, Steffensen IL, Mikalsen A, Paulsen JE, Alexander J. Adenomatous polyposis coli truncation mutations in 2-amino-1-methyl-6-phenylimidazo[4,5-b]pyridine (PhIP)-induced intestinal tumours of multiple intestinal neoplasia mice. Mutat Res. 2004;557:29-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 381. | Smits R, van der Houven van Oordt W, Luz A, Zurcher C, Jagmohan-Changur S, Breukel C, Khan PM, Fodde R. Apc1638N: a mouse model for familial adenomatous polyposis-associated desmoid tumors and cutaneous cysts. Gastroenterology. 1998;114:275-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 110] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 382. | Xu J, Cortellino S, Tricarico R, Chang WC, Scher G, Devarajan K, Slifker M, Moore R, Bassi MR, Caretti E, Clapper M, Cooper H, Bellacosa A. Thymine DNA Glycosylase (TDG) is involved in the pathogenesis of intestinal tumors with reduced APC expression. Oncotarget. 2017;8:89988-89997. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 383. | Kawaguchi Y, Hinoi T, Saito Y, Adachi T, Miguchi M, Niitsu H, Sasada T, Shimomura M, Egi H, Oka S, Tanaka S, Chayama K, Sentani K, Oue N, Yasui W, Ohdan H. Mouse model of proximal colon-specific tumorigenesis driven by microsatellite instability-induced Cre-mediated inactivation of Apc and activation of Kras. J Gastroenterol. 2016;51:447-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 384. | Roper J, Richardson MP, Wang WV, Richard LG, Chen W, Coffee EM, Sinnamon MJ, Lee L, Chen PC, Bronson RT, Martin ES, Hung KE. The dual PI3K/mTOR inhibitor NVP-BEZ235 induces tumor regression in a genetically engineered mouse model of PIK3CA wild-type colorectal cancer. PLoS One. 2011;6:e25132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 113] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 385. | Byun AJ, Hung KE, Fleet JC, Bronson RT, Mason JB, Garcia PE, Crott JW. Colon-specific tumorigenesis in mice driven by Cre-mediated inactivation of Apc and activation of mutant Kras. Cancer Lett. 2014;347:191-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 386. | Kang DW, Lee SW, Hwang WC, Lee BH, Choi YS, Suh YA, Choi KY, Min DS. Phospholipase D1 Acts through Akt/TopBP1 and RB1 to Regulate the E2F1-Dependent Apoptotic Program in Cancer Cells. Cancer Res. 2017;77:142-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 387. | Kitamura T, Biyajima K, Aoki M, Oshima M, Taketo MM. Matrix metalloproteinase 7 is required for tumor formation, but dispensable for invasion and fibrosis in SMAD4-deficient intestinal adenocarcinomas. Lab Invest. 2009;89:98-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 388. | Hamamoto T, Beppu H, Okada H, Kawabata M, Kitamura T, Miyazono K, Kato M. Compound disruption of smad2 accelerates malignant progression of intestinal tumors in apc knockout mice. Cancer Res. 2002;62:5955-5961. [PubMed] |
| 389. | Luo F, Brooks DG, Ye H, Hamoudi R, Poulogiannis G, Patek CE, Winton DJ, Arends MJ. Conditional expression of mutated K-ras accelerates intestinal tumorigenesis in Msh2-deficient mice. Oncogene. 2007;26:4415-4427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 390. | Edelmann W, Umar A, Yang K, Heyer J, Kucherlapati M, Lia M, Kneitz B, Avdievich E, Fan K, Wong E, Crouse G, Kunkel T, Lipkin M, Kolodner RD, Kucherlapati R. The DNA mismatch repair genes Msh3 and Msh6 cooperate in intestinal tumor suppression. Cancer Res. 2000;60:803-807. [PubMed] |
| 391. | Sakamoto K, Tominaga Y, Yamauchi K, Nakatsu Y, Sakumi K, Yoshiyama K, Egashira A, Kura S, Yao T, Tsuneyoshi M, Maki H, Nakabeppu Y, Tsuzuki T. MUTYH-null mice are susceptible to spontaneous and oxidative stress induced intestinal tumorigenesis. Cancer Res. 2007;67:6599-6604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |