Published online Feb 21, 2019. doi: 10.3748/wjg.v25.i7.848
Peer-review started: December 3, 2018
First decision: January 11, 2019
Revised: January 20, 2019
Accepted: January 26, 2019
Article in press: January 26, 2019
Published online: February 21, 2019
Processing time: 81 Days and 19.8 Hours
Embolic superior mesenteric artery (SMA) occlusion is associated with high mortality rates. Delayed treatment often leads to serious consequences, including intestinal necrosis, resection, and even patient death. Endovascular repair is being introduced, which can improve clinical symptoms and prognosis and decrease the incidence of exploratory laparotomy. Many reports have described successful endovascular revascularization of embolic SMA occlusion. However, most of those reports are case reports, and there are few reports on Chinese patients. In this paper, we describe the technical and clinical outcomes of aspiration therapy using a guiding catheter and long sheath technique which facilitates the endovascular repair procedure.
To evaluate the complications, feasibility, effectiveness, and safety of endovascular treatment for the acute embolic occlusion of the SMA.
This retrospective study reviewed eight patients (six males and two females) from August 2013 to October 2018 at Xuanwu Hospital, Capital Medical University. The patients presented with acute embolic occlusion of the SMA on admission and were initially diagnosed by computed tomography angiography (CTA). The patients who underwent endovascular treatment with a guiding catheter had no obvious evidence of bowel infarct. No intestinal necrosis was identified by gastrointestinal surgeons through peritoneal puncture or CTA. The complications, feasibility, effectiveness, safety, and mortality were assessed.
Six (75%) patients were male, and the mean patient age was 70.00 ± 8.43 years (range, 60-84 years). The acute embolic occlusion of the SMA was initially diagnosed by CTA. All patients had undertaken anticoagulation primarily, and percutaneous aspiration using a guiding catheter was then undertaken because the emboli had large amounts of thrombus residue. No death occurred among the patients. Complete patency of the suffering artery trunk was achieved in six patients, and defect filling was accomplished in two patients. The in-hospital mortality was 0%. The overall 12-mo survival rate was 100%. All patients survived, and two of the eight patients had complications (the clot broke off during aspiration).
Aspiration therapy is feasible, safe, and beneficial for acute embolic SMA occlusion. Aspiration therapy has many benefits for reducing patients’ death, resolving thrombi, and improving symptoms.
Core tip: Percutaneous aspiration embolectomy was recently used to treat embolic superior mesenteric artery (SMA) occlusion. The aim of this study was to assess the utility of endovascular revascularization. Eight patients with acute embolic SMA occlusion underwent aspiration therapy using a guiding catheter. The rate of technical success, clinical success, and adverse events was 100%, 100%, and 25%, respectively. Recurrence was not observed. The median follow-up period after aspiration was 328 d. Aspiration using a guiding catheter achieved immediate revascularization of emboli of the SMA trunk and is a useful tool in the recanalization of embolic occlusion of the SMA in select patients.
- Citation: Liu YR, Tong Z, Hou CB, Cui SJ, Guo LR, Qi YX, Qi LX, Guo JM, Gu YQ. Aspiration therapy for acute embolic occlusion of the superior mesenteric artery. World J Gastroenterol 2019; 25(7): 848-858
- URL: https://www.wjgnet.com/1007-9327/full/v25/i7/848.htm
- DOI: https://dx.doi.org/10.3748/wjg.v25.i7.848
Acute abdominal emergencies are critical, and the pathogenesis is complicated, partly due to acute mesenteric ischaemia (AMI), which comprises 1%-2% of acute abdominal emergencies[1-3]. Embolic superior mesenteric artery (SMA) occlusion is the most common cause of AMI and is associated with high mortality rates[4]. Delayed treatment of SMA occlusion often leads to serious consequences, including intestinal necrosis, resection, and even patient death. Exploratory laparotomy and surgical removal of the thrombus has been the major surgical technique in the past; however, endovascular repair is being introduced, as its efficacy has been proven in clinical trials[5-10]. Intervention improves clinical symptoms and prognosis and decreases the incidence of exploratory laparotomy.
Many reports have described successful endovascular revascularization of embolic SMA occlusion by several endovascular techniques, such as catheter thrombolysis and percutaneous aspiration embolectomy[1,11-17]. However, most of those reports are case reports, and there are few reports on Chinese patients. In this paper, we describe the technical and clinical outcomes of endovascular repair, namely, aspiration therapy using a guiding catheter, in eight Chinese patients with embolic SMA occlusion.
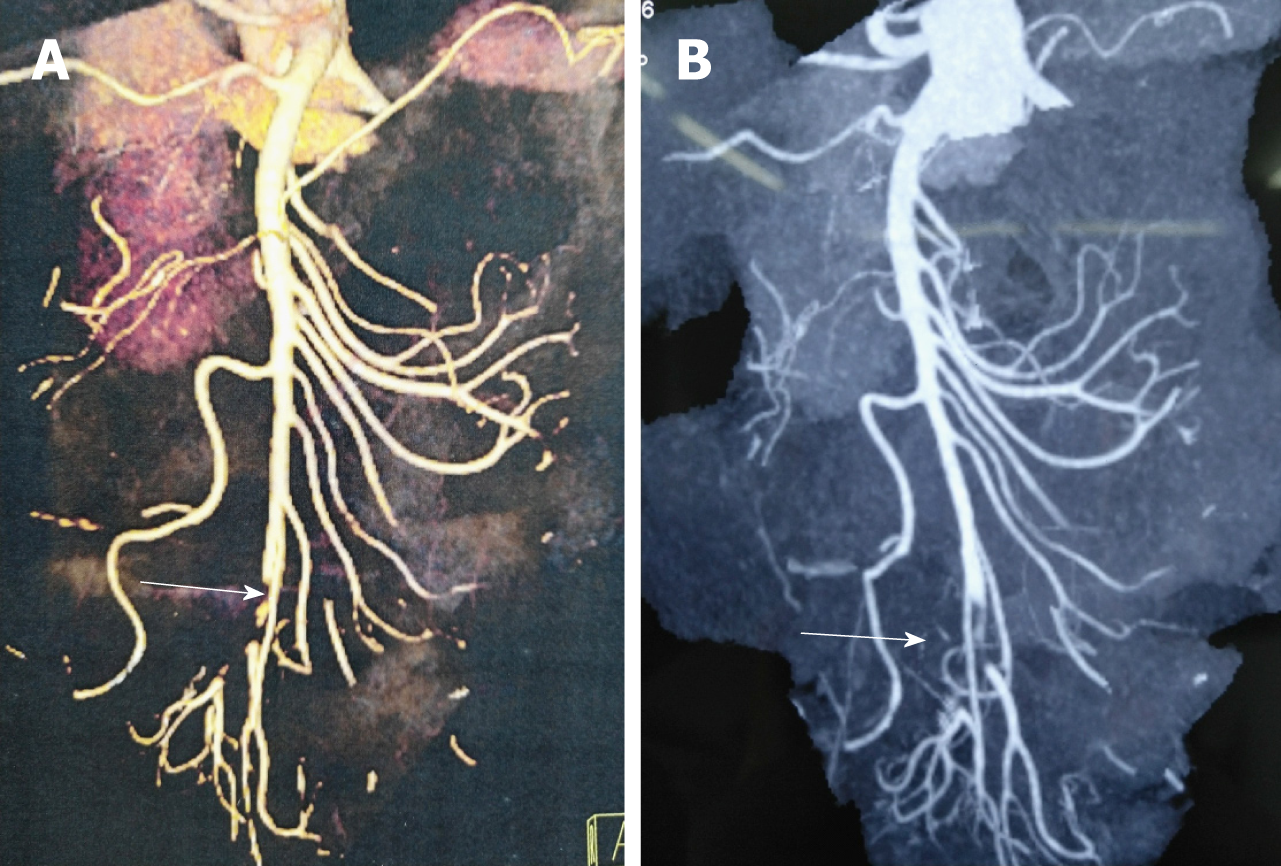
This study was a retrospective analysis in our institution. From August 2013 to October 2018, eight patients with SMA embolism, including six males and two females and ranging in age from 60 to 84 years (mean age, 70.00 ± 8.43 years), were treated by transcatheter aspiration therapy at Xuanwu Hospital. All patients were initially diagnosed by computed tomography angiography (CTA, Figure 1). The patients who underwent endovascular treatment had no obvious evidence of bowel infarct (Figure 2). No intestinal necrosis was identified by gastrointestinal surgeons through peritoneal puncture or CTA.
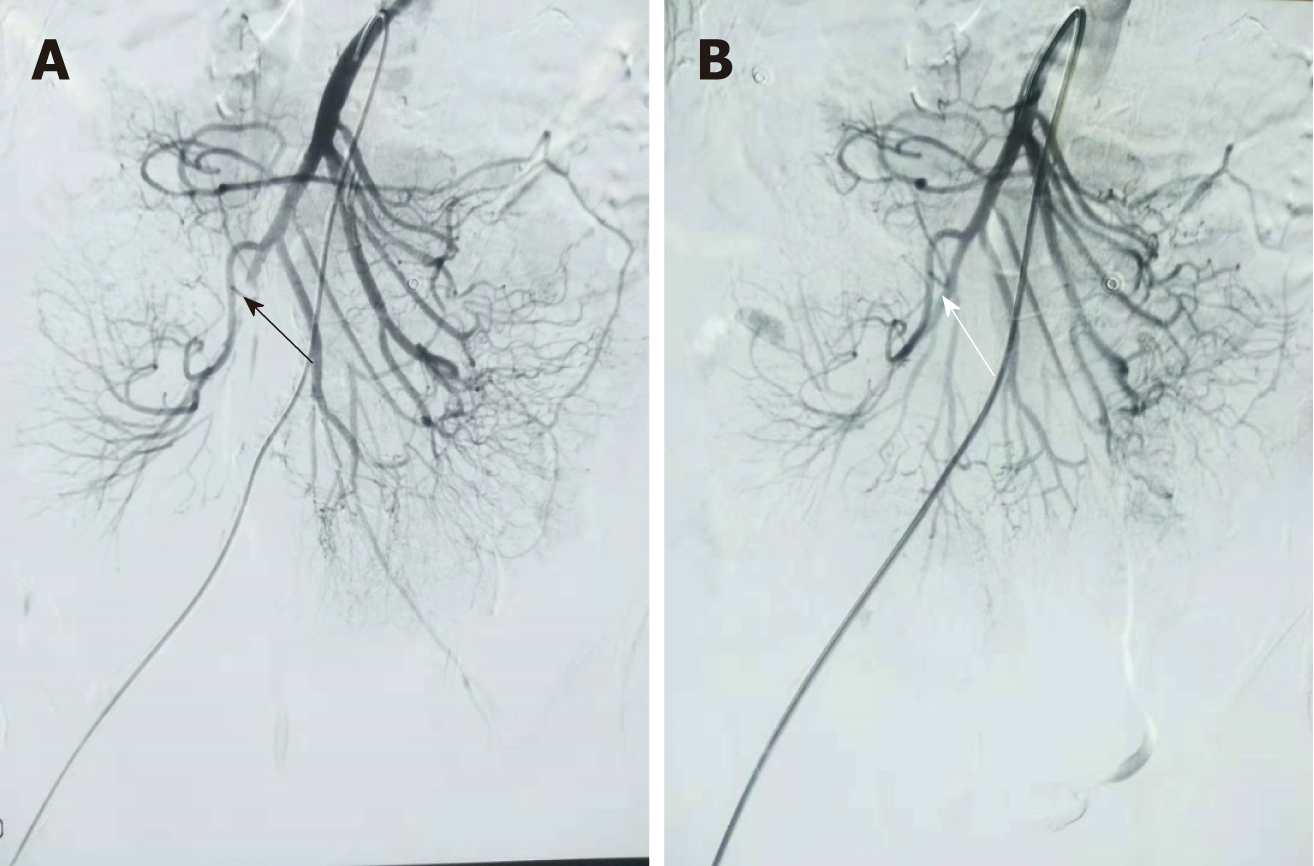
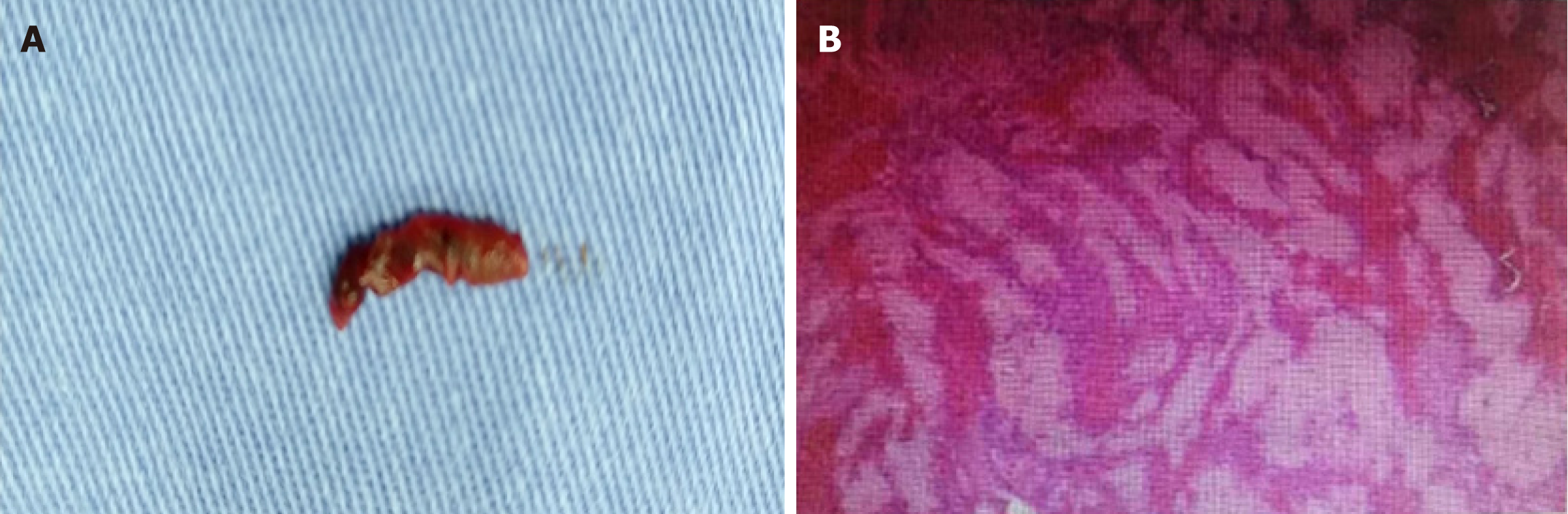
All operations were performed by an experienced vascular surgeon. Under local anaesthesia, the right common femoral artery was punctured according to the Seldinger technique and an 8-Fr short sheath (Introducer II; Terumo) was implanted. Then, heparin was administered (50 IU/kg, North China Pharmaceutical Company Ltd, China) via a short sheath. An additional 1000 IU was administered every hour. Selective catheterization of the SMA with the 5-Fr Cobra catheter (C1, Cook, Bloomington, IN, United States) or the SIMON 5-Fr catheter (SIM1, Selecon; Terumo, Tokyo, Japan) was performed. Through the catheter, angiography was performed to confirm the SMA embolism (Figure 3). A hydrophilic guidewire (Radifocus, Terumo, Tokyo, Japan) was navigated into the distal segment of the SMA. The short sheath replaced the 8-Fr long sheath of 65 cm (Super Arrow Flex PSI set, Arrow International, Reading, PA, United States), and the long sheath was inserted into the orifice of the SMA. The 8-Fr long sheath was left in the proximal section of the SMA. The 5-Fr catheter of 110 cm in length (DAV, Cook) was inserted into the 6F guiding sheath of 90 cm in length (BRITE TIP; Cordis, Miami Lakes, Florida), and the 6-Fr guiding catheter and the 5F catheter were advanced coaxially to the SMA over the guidewire. The 5-Fr catheter was removed and the 6-F guiding catheter reserved for aspiration of the emboli. A 50-mL syringe was connected to the 6-Fr guiding catheter. When the guiding catheter became occluded with the emboli, it was withdrawn slightly with pumping until blood was aspirated. The 6F guiding sheath was flushed thoroughly with saline solution into gauze so that the thrombus could be found (Figure 4). The guiding catheter was reinserted and the procedure repeated. The emboli of the branches were treated using a 5-F catheter. Urokinase (250000 IU, Tianjin Biochemical Pharmaceutical Co., Ltd.) was infused into the SMA through the catheter to resolve residual emboli. Papaverine (30 mg, North China Pharmaceutical Company, Ltd, China) was infused into the SMA through the catheter to resolve vasospasm.
One patient underwent catheter-directed thrombolysis (CDT). Thrombolysis was performed using a multiple-sidehole infusion catheter (Multi-Sideport, Cook) via the SMA with urokinase at a rate of 50000 IU/h to downsize the emboli. Thrombolysis was monitored by fibrinogen (fibrinogen value was larger than 1 g/L). Catheter-directed local anticoagulation with heparin sodium was continuously administered into the SMA as well. Dosage should be adapted to patients individually on the basis of tests of activated partial thromboplastin time (APTT 1.5-2.0 times normal value). An angiograph of thrombolysis efficiency was performed 48 h after the intervention.
All patients had clinical and imaging follow-up, which was performed every 3 mo one year after operation and then every 6 mo until death or October 31, 2018. During the follow-up, all patients were evaluated by clinical symptoms and signs, laboratory tests of blood routine examination, and CTA or ultrasonography of the SMA.
We reviewed the case file records. The clinical outcomes included feasibility, effectiveness, complications, clinical symptoms and signs, laparotomy, bowel resection, hospital stay, mortality and recurrence, SMA perfusion observed by CTA, and digital subtraction angiography (DSA).
Absence or presence of peritonitis was determined by clinical abdominal examination. Embolism was considered according to atrial fibrillation and a history of embolism. Degree of thrombus removal was divided into complete and partial. Complete thrombus removal referred to complete patency of the SMA and sufficient perfusion of the entire bowel, and partial thrombus removal referred to residual emboli or sluggish flow of the SMA.
The statistical methods of this study were reviewed by Cheng-Bei Hou from Center of Evidence-Based Medicine, Xuanwu Hospital, Capital Medical University. Data management and statistical analyses were performed using SPSS 19.0 software (SPSS Inc, Chicago, IL, United States). Continuous variables were tested for normal distribution. Normally distributed variables are expressed as the mean ± standard deviation (SD), whereas non-normally distributed variables are reported as median. Categorical variables are reported as counts with proportions.
The patients included six men and two women, with an age range from 60 to 84 years (mean age, 70.00 ± 8.43 years). SMA embolism was initially diagnosed by a vascular surgeon considering clinical manifestation and CTA findings. All patients were seen in consultation with a gastrointestinal surgeon and vascular surgeon. No intestinal necrosis was identified by doctors considering clinical symptoms, signs, peritoneal puncture, and CTA findings. After admission, all patients received low molecular weight heparin (LMWH) (100 IU/kg Sanofi Winthrop Industrie, France) anticoagulant therapy. Routine blood examination was performed, including white blood cell (WBC), neutrophilic granulocyte, red blood cell (RBC), and platelet (PLT) counts and hepatic and renal function analyses. The clinical characteristics of patients are shown in Table 1.
| Patient No. | Sex | Age (yr) | Basal disease | Symptoms | Signs (tenderness) | Signs (re-bound tenderness) | WBC count (×103/μL) | Echocardiography (LA τhrombus) |
| 1 | M | 60 | HBP | Abdominal pain, vomiting, dark stool | Present | Present | 15.3 | Absent |
| 2 | M | 68 | Af, DM | Abdominal pain, diarrhea | Present | Present | 17.4 | Absent |
| 3 | F | 71 | Af, CAD, HF | Abdominal pain, hematochezia | Present | Present | 24.0 | Absent |
| 4 | M | 84 | DM | Abdominal pain | Present | Absent | 17.8 | Absent |
| 5 | M | 61 | Af | Abdominal pain | Present | Absent | 15.1 | Absent |
| 6 | M | 66 | Af, DM | Abdominal pain, diarrhea | Present | Present | 16.9 | Absent |
| 7 | F | 70 | HBP | Abdominal pain, dark stool | Present | Present | 23.5 | Absent |
| 8 | M | 80 | HBP, DM | Abdominal pain, vomiting | Present | Absent | 17.1 | Absent |
The median white cell blood count was 17.25 × 109/L (range from 15.3 to 24.0 × 109/L), C-reactive protein (CRP) was 27.60 mg/L (range from 5 to 52 mg/L), platelet concentration was 264.35 × 109/L (range from 128 to 385 × 109/L), and the glomerular filtration rate (GFR) was 81.24 mL/min (range from 75 to 96 mL/min). No renal insufficiency was observed.
The interval between the onset of symptoms and the acquisition of angiography ranged from 9 to 30 h (median time, 9.50). Eight complete SMA trunk occlusions were detected by angiography via the catheter. In one patient (No. 2), emboli were noted in the jejunal artery branches. Six patients (Nos. 1 and 4-8) had good collateral flow. One patient (No. 2) had slow collateral flow, and one patient (No. 3) had no collateral flow (Table 2).
| Patient No. | CTA | Time from onset totreatment (h) | Occlusion of main SMA trunk | Branch lesion location(s) | Collateral flowto jejunal/ileal branches |
| 1 | Filling defect, mild bowel oedema, mild ileus | 9 | Complete occlusion | None | Good |
| 2 | Filling defect, mild bowel oedema, mild ileus | 10 | Complete occlusion | Jejunal arteries | Slow |
| 3 | Filling defect, mild bowel oedema, scanty ascites, mild ileus | 30 | Complete occlusion | None | Absent |
| 4 | Filling defect, mild bowel oedema, mild ileus | 7 | Complete occlusion; SMA stenosis | None | Good |
| 5 | Filling defect, mild bowel oedema, mild ileus | 8 | Complete occlusion | None | Good |
| 6 | Filling defect, mild bowel oedema, mild ileus | 11 | Complete occlusion | None | Good |
| 7 | Filling defect, mild bowel oedema, mild ileus | 6 | Complete occlusion | None | Good |
| 8 | Filling defect, mild bowel oedema, mild ileus | 28 | Complete occlusion | None | Good |
Percutaneous aspiration embolectomy using a guiding catheter was performed in all eight patients. The total procedure time from the initial diagnostic angiography to the final angiography was 53-85 min (mean time, 72.00 ± 13.70). Seven (Nos. 1, 2, 4, 5, and 6-8) patients initially underwent aspiration embolectomy, and thrombolysis was initially performed in one patient (No. 3). Thrombolysis was initially performed in the early study period because of the patient had heart failure, and primary aspiration embolectomy using a guiding catheter was performed in the late period as some thrombolysis was found 3 d after urokinase injection. In one patient (No. 2), primary percutaneous aspiration embolectomy was attempted, but residual emboli were noted in the jejunal artery branches. Intra-artery transcatheter thrombolytic therapy with urokinase was performed for the treatment of residual emboli. Thrombolysis was conducted for 3 d, resulting in complete resolution of the emboli. Follow-up angiography showed reestablishment of arterial flow. In two patients (Nos. 1 and 4), primary percutaneous aspiration embolectomy was applied, and the two patients received primary thrombolysis with urokinase (250000) during the operation because of the clot breaking off. PTA was performed in one patient (No. 4) because of SMA stenosis. Aspirated emboli consisted of white and red clots. At completion of the SMA aspiration, significantly improved filling of the SMA was seen in all eight patients. Aspiration thrombectomy of the SMA resulted in complete (Nos. 1, 2, and 4-7) or partial (Nos. 3 and 8) restoration of blood flow in the main SMA, which was documented on immediate direct SMA angiography. Primary percutaneous aspiration embolectomy was applied for two patients (Nos. 1 and 4), and the two patients received primary thrombolysis with urokinase (250000) during the operation because of the clot breaking off. The detached clots did not result in intestinal ischaemia, as collateral flow to the jejunal/ileal branches was good (Table 3).
| Patient No. | Total procedure time (min) | Trunk lesion | Branch lesion location(s) | Additional treatment | Complications |
| 1 | 85 | Successful | The clot breaking off and ileal arterial embolism, good flow | Thrombolysis with urokinase during the operation | The clot breaking off |
| 2 | 85 | Successful | Multiple residual emboli in jejunal arteries, slow flow | Intra-artery transcatheter thrombolytic therapy with urokinase successful | - |
| 3 | 50 | Partial rec-analization | - | thrombolysis was initially performed before aspiration embolectomy | - |
| 4 | 75 | Successful (PTA) | The clot breaking off and ileocolic artery emboli. | primary thrombolysis with urokinase during the operation | The clot breaking off |
| 5 | 79 | Successful | - | - | - |
| 6 | 80 | Successful | - | - | - |
| 7 | 53 | Successful | - | - | - |
| 8 | 69 | Partial recanalization | - | - | - |
Substantial improvement in abdominal pain was observed within 1-2 d after the operation in all patients. Sufficient clinical improvement, characterized by a progressive decrease in abdominal pain and distention, was observed in all patients. Oral nutrition intake was started at 2-17 (7.75 ± 5.65) d. The eight patients were discharged 9-17 (12.25 ± 3.11) d after admission. The in-hospital mortality was 0%. Abdominal pain, nausea, distention, haematochezia, and diarrhoea were completely resolved when the patients were discharged. CTA images obtained before discharge demonstrated nearly complete recanalization of SMA thrombosis in all patients, with improvement in oedema of the intestine in all patients. Heart failure of one patient (No. 3) was improved. One patient (No. 4) suffered from left cerebral infarction because of an embolism aroused by atrial fibrillation, and symptoms improved after discharge (Table 4).
| Patient No. | The time of feed (d) | Hospital stay (d) | In-hospital mortality | Symptoms | Signs (tenderness) | Signs (rebound tenderness) |
| 1 | 2 | 9 | None | Abdominal symptom resolved in 1 d | Present | Present |
| 2 | 6 | 12 | None | Diarrhoea developed after aspiration but subsided spontaneously; Abdominal symptom resolved in 1 d | Present | Present |
| 3 | 6 | 12 | None | Haematochezia developed after aspiration but subsided spontaneously; Abdominal symptom resolved in 1 d | Present | Present |
| 4 | 17 | 17 | None | Abdominal symptom resolved in 1 d | Present | Absent |
| 5 | 5 | 8 | None | Abdominal symptom resolved in 1 d | Present | Absent |
| 6 | 16 | 11 | None | Diarrhoea lasted 2 d | Present | Present |
| 7 | 7 | 13 | None | Abdominal symptom resolved in 2 d; Dark stool lasted 3 d | Present | Present |
| 8 | 3 | 16 | None | Abdominal symptom resolved in 2 d | Present | Absent |
The median length of time of follow-up was 328 (range, 90-390) months. One patient (No. 4) developed mild abdominal pain 3 mo after surgery because of SMA stenosis, and other patients persisted asymptomatically. Routine blood tests were normal. No patients required extensive bowel resection. No thrombus recurrence was found under regular anticoagulation. Warfarin or rivaroxaban was applied orally in all patients at least 6 mo after discharge if there were no risk factors for recurrence. During the follow-up, ultrasonography confirmed the blood flow perfusion of the SMA.
Percutaneous aspiration using a guiding catheter for acute embolic occlusion of the SMA may lead to dissection of the SMA. The dissection restricting blood flow requires emergency treatment. Dissection of the SMA may be caused by the gap between the guidewire and the guiding catheter. The gap between the guidewire and the guiding catheter should be reduced. Since there were no dilators that fit the guiding catheter, a smaller catheter was used as a dilator. There is no gap between the 6-Fr guiding catheter and the 5-Fr catheter; thus, the 6-Fr guiding catheter was used to remove the SMA emboli, and the 5-Fr catheter was used to remove the emboli in the branches of the SMA. From two studies performed by Acosta et al[11] and Kawasaki et al[14], we conclude that larger catheters lead to increased intima dissection. SMA dissection was not found in any patients in our study. With a careful operation and coaxial advancing of the guiding catheter and a seamless dilator, the incidence of SMA dissection can be reduced. It is crucial to select the appropriate guiding catheter according to the SMA diameter. As for difficult transcutaneous cases, it is a good choice using a hybrid approach. SMA puncture was practiced under genuine direct vision can avoid dissection of the SMA. Furthermore, the intestine can be detected through laparotomy.
All four patients successfully underwent aspiration. Raupach et al[18] analysed 37 patients with acute mesenteric embolism who underwent primary endovascular therapy, and achieved complete recanalization of the SMA trunk in 91.9% of cases. Our technique used a long sheath compared with other reports on the treatment of trunk lesions. The long sheath was inserted into the orifice of the SMA, and the long sheath was left in the proximal section of the SMA. The guiding catheter was inserted into the SMA repeatedly and immediately through the long sheath. Using a long sheath both saves time and avoids SMA dissection.
A distal embolism may develop during advancement of the catheter. As for the SMA trunk, the therapeutic effects of thrombolysis are uncertain. Björnsson et al[9] reported a feature that successful thrombolysis was achieved in 30 patients; 13 explorative laparotomies, 10 repeat laparotomies, and 8 bowel resections were performed; and the in-hospital mortality rate was 26%. Boo-Gyoung et al[19] initially tried endovascular thrombolytic therapy, but it did not achieve complete revascularization. Therefore, they performed a percutaneous aspiration thrombectomy, which led to complete revascularization without any additional procedures. However, for branch arteries, the thrombolysis was useful[20].
Heiss et al[13] reported that SMA aspiration showed a 30-d mortality rate of 33%. In another paper, 1 patient died at 12 h, and another patient died of short bowel syndrome at 8 mo[11]. Kawasaki et al[14] reported a 30-d mortality rate of 14% (1 of 7 patients). The patients in our study recovered quickly. No patients needed bowel resection. We think that the low morbidity of our study might be explained by the following: (1) patients were diagnosed early by CT; and (2) patients had relatively mild symptoms and signs, because severe patients were admitted to undergo gastrointestinal surgery. The initial treatment modality should be decided by consensus between gastrointestinal and vascular surgeons considering the patient’s symptoms and signs, CT findings, laboratory results, and clinical experiences[21]. We first tried endovascular treatment if the CT scan had no obvious evidence of bowel infarct[22]. Rebound tenderness may suggest bowel necrosis and may lead to exploratory laparotomy. However, endovascular treatment may make surgical laparotomy unnecessary or may reduce surgical procedure and time. Thus, we adopted endovascular treatment first in seven patients (7/8). Choi et al[23] reported that nine patients with embolic occlusion of the SMA were treated by percutaneous aspiration embolectomy, and no patients had obvious evidence of bowel infarction on CT scans. One patient died of whole bowel necrosis and sepsis, and eight patients survived without complications.
The aspiration method that uses the long sheath technique might therefore be more feasible than thrombolysis[1]; it may also be more feasible than surgical embolectomy[10]. Several other devices can be used to remove blood clots in the SMA, for example, a Rotarex systema mechanical rotational thrombectomy device[24]. These devices are also effective in the removal of blood clots, but they may lead to complications and increase medical costs. Bruno Freitas et al reported complications represented by self-limited small perforations with a 6F Rotarex Debulking Device (Straub Medical, Wangs, Switzerland)[25]. Percutaneous mechanical thrombectomy seems to be a rapid and effective treatment for acute SMA embolism in the median portion of its trunk[26]. Aspiration using a guiding catheter is inexpensive and effective according to several studies, including the current study[11,27].
Follow-up of patients for 1 year detected no cases of recurrence. One patient (No. 4) developed mild abdominal pain 3 mo after surgery because of SMA stenosis. The long-term consequences were good because of early revascularization. Echocardiography was performed in all patients, but thrombus was not detected in the left atrium. Anticoagulation drugs were prescribed to all patients to prevent re-embolism regardless of the echocardiography findings.
The main limitation of our study is the analysis of a small number of enrolled patients. Moreover, the peritonitis patients were admitted for gastrointestinal surgery; thus, a comparative study between open surgery treatment and endovascular treatment was not conducted. Third, thrombolysis and aspiration require further study.
Emboli resulting in embolic occlusion of the SMA often come from the atrium. Aspiration using a guiding catheter can remove most of the clots, and aspiration can achieve immediate revascularization of emboli of the SMA trunk. Thrombolysis can deal with residual fresh blood clots. However, with regard to old thrombi, which cannot be cleared by aspiration, further studies are needed.
Embolic superior mesenteric artery (SMA) occlusion is associated with high mortality rates. Delayed treatment often leads to serious consequences, including intestinal necrosis, resection, and even patient death. Endovascular repair is being introduced, which can improve clinical symptoms and prognosis and decrease the incidence of exploratory laparotomy. Many reports have described successful endovascular revascularization of embolic SMA occlusion. However, most of those reports are case reports, and there are few reports on Chinese patients. In this paper, we describe the technical and clinical outcomes of aspiration therapy using a guiding catheter and long sheath technique which facilitates the endovascular repair procedure.
To evaluate the complications, feasibility, effectiveness, and safety of endovascular treatment using a guiding catheter for the acute embolic occlusion of the SMA.
Many reports have described successful endovascular revascularization of embolic SMA occlusion by several endovascular techniques. However, most of those reports are case reports. There are few reports on Chinese patients. In this paper, we describe the technical and clinical outcomes of aspiration therapy using a guiding catheter and long sheath technique which facilitates the endovascular repair procedure.
This retrospective study reviewed patients with acute embolic occlusion of the SMA. All patients were treated by aspiration therapy with a guiding catheter. The complications, feasibility, effectiveness, safety, and mortality were assessed.
All patients had successfully undertaken percutaneous aspiration using a guiding catheter. No death occurred among the patients. Most of the clots were removed and patency of the suffering artery trunk was achieved. Although the complication of the clot breaking off was detected in partial patients, blood perfusion was not affected.
We need a large number of enrolled patients and conduct a comparative study between open surgery treatment and endovascular treatment. Furthermore, thrombolysis can deal with fresh blood clots. However, with regard to old thrombi, which cannot be cleared by aspiration, further studies are needed.
Aspiration therapy is feasible, safe, and beneficial for acute embolic SMA occlusion. Aspiration therapy using a guiding catheter and long sheath technique facilitates the endovascular repair procedure. Aspiration therapy has many benefits for reducing patients’ death, resolving thrombi, and improving symptoms.
Aspiration therapy using a guiding catheter and long sheath technique is feasible, safe and beneficial for acute SMA embolic occlusion, which should be applied and popularized. Especially, auxiliary applications of a long sheath technique facilitate operation procedure. Tender operation is needed to avoid the clot breaking off. However, with regard to old thrombi, which cannot be cleared by aspiration, further studies are needed. A randomized controlled trial comparing open surgery treatment and endovascular treatment is needed to be conducted in the future.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Manenti A S- Editor: Ma RY L- Editor: Wang TQ E- Editor: Huang Y
| 1. | Björck M, Acosta S, Lindberg F, Troëng T, Bergqvist D. Revascularization of the superior mesenteric artery after acute thromboembolic occlusion. Br J Surg. 2002;89:923-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 51] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Gupta PK, Natarajan B, Gupta H, Fang X, Fitzgibbons RJ. Morbidity and mortality after bowel resection for acute mesenteric ischemia. Surgery. 2011;150:779-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 74] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 3. | Wong YC, Wu CH, Wang LJ, Chen HW, Lin BC, Huang CC. Mesenteric vascular occlusion: comparison of ancillary CT findings between arterial and venous occlusions and independent CT findings suggesting life-threatening events. Korean J Radiol. 2013;14:38-44. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Schoots IG, Levi MM, Reekers JA, Lameris JS, van Gulik TM. Thrombolytic therapy for acute superior mesenteric artery occlusion. J Vasc Interv Radiol. 2005;16:317-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 86] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Ryer EJ, Kalra M, Oderich GS, Duncan AA, Gloviczki P, Cha S, Bower TC. Revascularization for acute mesenteric ischemia. J Vasc Surg. 2012;55:1682-1689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 114] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 6. | Gagnière J, Favrolt G, Alfidja A, Kastler A, Chabrot P, Cassagnes L, Buc E, Pezet D, Boyer L. Acute thrombotic mesenteric ischemia: primary endovascular treatment in eight patients. Cardiovasc Intervent Radiol. 2011;34:942-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Zeleňák K, Sinák I, Janík J, Mikolajčík A, Mištuna D. Successful recanalization of acute superior mesenteric artery thromboembolic occlusion by a combination of intraarterial thrombolysis and mechanical thrombectomy with a carotid filter. Cardiovasc Intervent Radiol. 2013;36:844-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Tsuda M, Nakamura M, Yamada Y, Saito H, Ishibashi T, Takahashi S. Acute superior mesenteric artery embolism: rapid reperfusion with hydrodynamic thrombectomy and pharmacological thrombolysis. J Endovasc Ther. 2003;10:1015-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Björnsson S, Björck M, Block T, Resch T, Acosta S. Thrombolysis for acute occlusion of the superior mesenteric artery. J Vasc Surg. 2011;54:1734-1742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Block TA, Acosta S, Björck M. Endovascular and open surgery for acute occlusion of the superior mesenteric artery. J Vasc Surg. 2010;52:959-966. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 92] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 11. | Acosta S, Sonesson B, Resch T. Endovascular therapeutic approaches for acute superior mesenteric artery occlusion. Cardiovasc Intervent Radiol. 2009;32:896-905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 75] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Resch TA, Acosta S, Sonesson B. Endovascular techniques in acute arterial mesenteric ischemia. Semin Vasc Surg. 2010;23:29-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Heiss P, Loewenhardt B, Manke C, Hellinger A, Dietl KH, Schlitt HJ, Scheibl K, Feuerbach S, Paetzel C. Primary percutaneous aspiration and thrombolysis for the treatment of acute embolic superior mesenteric artery occlusion. Eur Radiol. 2010;20:2948-2958. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Kawasaki R, Miyamoto N, Oki H, Yamaguchi M, Okada T, Sugimura K, Sugimoto K. Aspiration therapy for acute superior mesenteric artery embolism with an angled guiding sheath and guiding catheter. J Vasc Interv Radiol. 2014;25:635-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Shah SN, Sacks D, Chavali R. Mechanical embolectomy and recanalization of superior mesenteric artery embolism using the MERCI retrieval device. J Vasc Interv Radiol. 2011;22:1638-1640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Goltz JP, Petritsch B, Spor L, Hahn D, Kickuth R. Acute thromboembolic occlusion of the superior mesenteric artery following covered stent occlusion in the superior mesenteric artery: endovascular therapy using mechanical rotational thrombectomy. Vasa. 2012;41:375-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Yang HJ, Cho YK, Jo YJ, Jung YY, Choi SA, Lee SH. Successful recanalization of acute superior mesenteric artery thrombotic occlusion with primary aspiration thrombectomy. World J Gastroenterol. 2010;16:4112-4114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Raupach J, Lojik M, Chovanec V, Renc O, Strýček M, Dvořák P, Hoffmann P, Guňka I, Ferko A, Ryška P, Omran N, Krajina A, Čabelková P, Čermáková E, Malý R. Endovascular Management of Acute Embolic Occlusion of the Superior Mesenteric Artery: A 12-Year Single-Centre Experience. Cardiovasc Intervent Radiol. 2016;39:195-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 19. | Kim BG, Ohm JY, Bae MN, Kim HN, Kim YJ, Chung MH, Park CS, Ihm SH, Kim HY. Successful percutaneous aspiration thrombectomy for acute mesenteric ischemia in a patient with atrial fibrillation despite optimal anticoagulation therapy. Can J Cardiol. 2013;29:1329.e5-1329.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Byun SJ, So BJ. Successful aspiration and thrombolytic therapy for acute superior mesenteric artery occlusion. J Korean Surg Soc. 2012;83:115-118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (2)] |
| 21. | Acosta S. Surgical management of peritonitis secondary to acute superior mesenteric artery occlusion. World J Gastroenterol. 2014;20:9936-9941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 38] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 22. | Liu YR, Huang B, Yuan D, Wu ZP, Zhao JC. Unusual case of digestive hemorrhage: celiac axis-portal vein arteriovenous fistula. World J Gastroenterol. 2015;21:1362-1364. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Choi KS, Kim JD, Kim HC, Min SI, Min SK, Jae HJ, Chung JW. Percutaneous Aspiration Embolectomy Using Guiding Catheter for the Superior Mesenteric Artery Embolism. Korean J Radiol. 2015;16:736-743. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Zhang Z, Chen X, Zhu R. Percutaneous Mechanical Thrombectomy Treatment of Acute Superior Mesenteric Artery Embolism. EJVES Short Rep. 2017;34:17-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Freitas B, Bausback Y, Schuster J, Ulrich M, Bräunlich S, Schmidt A, Scheinert D. Thrombectomy Devices in the Treatment of Acute Mesenteric Ischemia: Initial Single-Center Experience. Ann Vasc Surg. 2018;51:124-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 26. | Kuhelj D, Kavcic P, Popovic P. Percutaneous mechanical thrombectomy of superior mesenteric artery embolism. Radiol Oncol. 2013;47:239-243. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 27. | Ogihara S, Yamamura S, Tomono H, Iwabuchi H, Ebihara T, Minagawa Y, Ogawa T, Kurosawa S, Yakabi K, Nakamura T. Superior mesenteric arterial embolism: treatment by trans-catheter thrombo-aspiration. J Gastroenterol. 2003;38:272-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |