Published online Mar 21, 2018. doi: 10.3748/wjg.v24.i11.1278
Peer-review started: January 11, 2018
First decision: January 25, 2018
Revised: January 30, 2018
Accepted: February 9, 2018
Article in press: February 9, 2018
Published online: March 21, 2018
Processing time: 64 Days and 4.9 Hours
To evaluate the safety and feasibility of a new technology combining low-pressure pneumoperitoneum (LPP) and abdominal wall lift (AWL) in laparoscopic total mesorectal excision (TME) for rectal cancer.
From November 2015 to July 2017, 26 patients underwent laparoscopic TME for rectal cancer using LPP (6-8 mmHg) with subcutaneous AWL in Qilu Hospital of Shandong University, Jinan, China. Clinical data regarding patients’ demographics, intraoperative monitoring indices, operation-related indices and pathological outcomes were prospectively collected.
Laparoscopic TME was performed in 26 cases (14 anterior resection and 12 abdominoperineal resection) successfully, without conversion to open or laparoscopic surgery with standard-pressure pneumoperitoneum. Intraoperative monitoring showed stable heart rate, blood pressure and paw airway pressure. The mean operative time was 194.29 ± 41.27 min (range: 125-270 min) and 200.41 ± 20.56 min (range: 170-230 min) for anterior resection and abdominoperineal resection, respectively. The mean number of lymph nodes harvested was 16.71 ± 5.06 (range: 7-27). There was no positive circumferential or distal resection margin. No local recurrence was observed during a median follow-up period of 11.96 ± 5.55 mo (range: 5-23 mo).
LPP combined with AWL is safe and feasible for laparoscopic TME. The technique can provide satisfactory exposure of the operative field and stable operative monitoring indices.
Core tip: Low-pressure pneumoperitoneum (LPP) and abdominal wall lift (AWL) have been proposed as alternative approaches to standard-pressure pneumoperitoneum to avoid adverse cardiorespiratory effects. However, the operative field under these approaches is less optimal and accompanied by increased technical difficulties. We developed a new technique combining LPP and AWL, which improved exposure of the operative field that was compromised with LPP or AWL alone. We evaluated the safety and feasibility of this new technique in 26 cases of laparoscopic total mesorectal excision for rectal cancer. This technique can provide satisfactory exposure of the operative field and stable operative monitoring indices.
- Citation: Xia PT, Yusofu M, Han HF, Hu CX, Hu SY, Yu WB, Liu SZ. Low-pressure pneumoperitoneum with abdominal wall lift in laparoscopic total mesorectal excision for rectal cancer: Initial experience. World J Gastroenterol 2018; 24(11): 1278-1284
- URL: https://www.wjgnet.com/1007-9327/full/v24/i11/1278.htm
- DOI: https://dx.doi.org/10.3748/wjg.v24.i11.1278
Pneumoperitoneum with carbon dioxide (CO2) is the conventional method of creating a workspace in laparoscopic surgery. The application of pneumoperitoneum results in a variety of physiologic alterations, due to the systemic absorption of CO2 and increased intra-abdominal pressure. CO2 absorption across the peritoneum into the circulation can lead to hypercarbia and changes in blood gas parameters. Appropriate ventilator adjustment is usually required to eliminate the increased CO2 load. Increased intraabdominal pressure by standard-pressure pneumoperitoneum (SPP; 12-15 mmHg) has been reported to result in lower respiratory compliance, increased paw airway pressure, enhanced venous stasis, reduced portal venous pressure and impaired cardiac function[1-5]. These alterations may be detrimental in high-risk patients with poor cardiopulmonary reserve, such as older and morbidly obese patients with American Society of Anesthesiologists (ASA) status III and IV[6].
Low-pressure pneumoperitoneum (LPP), defined as 5-7 mmHg[7], has been proposed to reduce the adverse consequences of SPP, and is recommended in older and compromised patients. It was reported that LPP reduced the adverse effects on cardiopulmonary function without affecting laparoscopic feasibility[5,8]. It has also proved feasible and safe in cholecystectomy[5,9], Nissen fundoplication[10], hysterectomy[11], adrenalectomy[12] and donor nephrectomy[13]. Abdominal wall lift (AWL) is another alternative technique to SPP which avoids the destructive changes associated with CO2 absorption and increased intraabdominal pressure. A variety of AWL systems have been developed and applied in a wide range of surgical procedures[14]. Compared with SPP, AWL results in more stable cardiopulmonary, hemodynamic and renal functions during laparoscopic procedures[15-17].
A frequent disadvantage during laparoscopic surgery with LPP or AWL is that the operative field is less optimal, which increases technical difficulties. In order to obtain adequate visualization, we combined LPP with AWL and initially used this technique in a case of laparoscopic single-site cholecystectomy[18]. In the present prospective pilot study, we aimed to evaluate the safety and feasibility of LPP with AWL in laparoscopic total mesorectal excision (TME) for rectal cancer.
This was a prospective study, and the protocol was approved by the Ethics Committee of Scientific Research of Shandong University Qilu Hospital, Jinan, China. From November 2015 to May 2017, 26 patients underwent laparoscopic TME using LPP with AWL in Qilu Hospital of Shandong University, Jinan, China. Written informed consent was obtained from all patients. Rectal adenocarcinoma was diagnosed by colonoscopy and biopsy. Computed tomography scans of the abdomen and pelvis were used to determine tumor stage. Patients without distant metastasis were eligible for enrollment in the study. All operations were performed by the same surgical group with considerable experience in advanced laparoscopic gastroenterological surgery.
Clinical data regarding patients’ demographics [age, sex, body mass index (BMI)], ASA status, intraoperative monitoring indices (heart rate, blood pressure and paw airway pressure), operative time, blood loss, complications and pathological outcomes (tumor size, differentiation, depth of invasion, lymph nodes harvested, Dukes stage, completeness of TME, circumferential and distal margins) were obtained.
The subcutaneous AWL system (Mizuho Medical Inc., Tokyo, Japan) was used in this study. It consisted of a sterilized steel scaffold with a lifting arm, retractors and steel needles. Other instruments included a harmonic scalpel (Ultracision; Ethicon Endosurgery, Cincinnati, OH, United States) and conventional laparoscopic instruments, such as a coagulation hook, dissector and grasper (Yida Medical Device Co., Ltd., Hangzhou, China). Hem-O-Lock clips (Weck Closure Systems, Triangle Park, NC, United States) were used to ligate vessels.
The patients were placed in the lithotomy position under general anesthesia with a laryngeal mask airway. A 10-mm supraumbilical arc incision was made, and then a Veress needle was inserted to create the CO2 pneumoperitoneum. The pressure was maintained at 6 mmHg with an insufflation rate of 10 L/min. The steel scaffold was fixed to the operating table. A sterilized needle was inserted through the subcutaneous tissue at 5 cm above the pubic level, then drafted by a retractor and the abdominal wall was slightly elevated to obtain additional exposure of the operative area (Figure 1).
The procedures were performed using 5 trocars. A careful exploration was performed to detect possible liver, peritoneal or pelvis metastases. The patient was then adjusted to the head-down position, which was about 20°-30° inclined to help move the small intestine for better exposure of the inferior mesenteric artery (IMA). The dissection began from the sigmoid mesocolon at the level of the sacral promontory, up to the origin of the IMA. The ascending left colic artery was preserved after a thorough clearance of the lymphatic and adipose tissues at the base of the IMA. The IMA was then ligated, and the inferior mesenteric vein was dissected and ligated at the level of the ligament of Treitz. The splenic flexure was mobilized routinely to achieve a tension-free anastomosis.
Exposure seemed inadequate during the above procedures, and an effort was made to achieve the optimal operative field. We developed and tested three methods. The first was to add a second needle in the supraumbilical area. This was abandoned due to frequent collisions of the instruments with the scaffold and lifting arms. We then tried the method reported by Park et al[19], where anchoring sutures were placed around the camera port and lifted up by an assistant to retract the abdominal wall for additional exposure. This method was successful and the workspace was improved. However, the view obtained from manual work was not stable. Therefore, we increased the pressure of the pneumoperitoneum to 8 mmHg. This method provided an adequate operative field for dissection of the IMA and inferior mesenteric vein and mobilization of the splenic flexure. These procedures were completed within approximately 20-30 min, and the pressure was then reduced to 6 mmHg.
TME was then started posteriorly after identification of the Holy Plane. Dissection was performed laterally and anteriorly down to the pelvic floor, until circumferential rectal mobilization was complete. The hypogastric nerves, inferior hypogastric plexuses, presacral nerves and ureters were carefully identified and preserved. For patients undergoing anterior resection, an endoscopic linear stapler was used to divide the rectum. The specimen was extracted through a protected incision at the left lower trocar site. After division of the proximal colon and introduction of the anvil of a circular stapler were complete, an intracorporeal end-to-end colorectal anastomosis was performed. A rectal decompression tube was placed and no diverting ileostomy was constructed. An abdominoperineal resection was performed if the tumor was located less than 5 cm from the anal verge, and perforation of the specimen was avoided with careful operation.
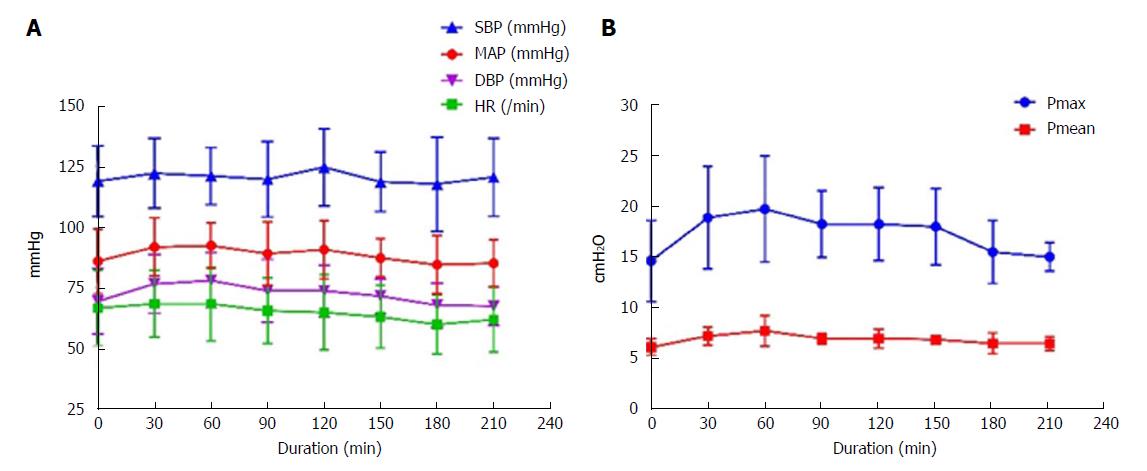
All 26 laparoscopic TME procedures, including 14 cases of anterior resection and 12 cases of abdominoperineal resection, were successfully completed without intraoperative complications. The patients’ demographics, perioperative data and pathologic outcomes are summarized in Table 1. LPP combined with AWL provided adequate exposure of the operating area. There were no conversions to open or laparoscopic surgery with SPP. Intraoperative monitoring resulted in stable curves of heart rate and blood pressure during surgery (Figure 2A). Peak and mean paw airway pressure increased when the pneumoperitoneum was created at the beginning of surgery, was stable throughout the laparoscopic stage, and then decreased after CO2 was discharged at approximately 150-180 min (Figure 2B).
| Variable | n/mean ± SD (range) |
| Age in yr | 62.71 ± 8.71 (41- 82) |
| Sex | |
| Male | 17 |
| Female | 9 |
| BMI in kg/m2 | 24.39 ± 2.68 (21.11-30.12) |
| ASA grade | |
| I | 1 |
| II | 22 |
| III | 3 |
| IV | 0 |
| Procedure | |
| AR | 14 |
| APR | 12 |
| Operative time in min | |
| AR | 194.29 ± 41.27 (125-270) |
| APR | 200.41 ± 20.56 (170-230) |
| Estimated blood loss in mL | |
| AR | 35.71 ± 16.35 (20-80) |
| APR | 85.00 ± 26.61 (50-140) |
| Postoperative complications | |
| Shoulder pain | 1 |
| Pulmonary infection | 1 |
| Calf muscular venous thrombosis | 2 |
| Dysuria | 4 |
| Tumor size in cm | |
| Length | 4.29 ± 1.19 (2-6.5) |
| Thickness | 1.12 ± 0.45 (0.5-2) |
| Distal resection margin in cm | |
| AR | 3.14 ± 1.34 (2-5) |
| APR | - |
| Differentiation | |
| Poorly | 2 |
| Moderate | 19 |
| Highly | 5 |
| Depth of invasion | |
| T1 | 1 |
| T2 | 7 |
| T3 | 1 |
| T4 | 17 |
| Lymph nodes harvested | 16.71 ± 5.06 (7-27) |
| Dukes stage | |
| A | 6 |
| B | 5 |
| C | 15 |
| Follow-up in mo | 11.96 ± 5.55 (5-23) |
One patient had shoulder pain and pulmonary infection postoperatively. Dysuria occurred in 4 male patients after urethral catheters were removed. All 4 patients were diagnosed with benign prostatic hyperplasia preoperatively and the catheters were re-indwelt. All patients resumed free liquid diet 24 h after surgery. The rectal decompression tube was removed 3 d after surgery. There were no cases of adverse cardiovascular events, bleeding or anastomotic leakage observed after surgery.
The rectal specimens were thoroughly examined by the same group of colorectal pathologists. No positive circumferential or distal resection margins were found. No local recurrences were observed during a mean follow-up period of 11.96 mo (range: 5-23 mo).
LPP combined with AWL has been proposed as an alternative approach to SPP by the European Association for Endoscopic Surgery[7]. We initially used this method in a case of laparoscopic transumbilical single-site cholecystectomy which was converted from a gasless laparoscopic single-site procedure with AWL[18]. Due to the high BMI of the patient, a 6 mmHg pneumoperitoneum was created for better exposure of the operative field. In the present study, this technique was applied in laparoscopic TME for the first time.
Our preliminary experience indicated that LPP with AWL was safe and provided a satisfactory workspace for TME. The number of lymph nodes retrieved, the completeness of TME, the circumferential and mean distance to the distal margin were comparable with those reported in studies using SPP[20-23]. Another LPP (8 mmHg) and AWL technique was designed by Park et al[19] and proved feasible in laparoscopic colorectal surgery. In their study, anchoring sutures were placed around the camera port and lifted up by an assistant to retract the abdominal wall for additional exposure. Unlike this technique, we used the subcutaneous AWL system introduced by Nagai et al[24] and Hashimoto et al[25], in which a needle was inserted to retract the inferior abdominal wall rather than the periumbilical area. This technique provided a stable and superior operative field, although no strict comparison was performed between the two techniques.
The present study indicated that LPP combined with AWL resulted in stable heart rate, blood pressure and paw airway pressure monitored during laparoscopic TME. For rectal surgery which requires exposure of the lower abdomen, a head-down or Trendelenburg position is necessary. Pneumoperitoneum combined with this position contributes to pushing abdominal organs towards the chest for sufficient exposure of the IMA and mesocolon before dissection in TME. However, SPP combined with head-down or Trendelenburg position significantly reduces pulmonary compliance by more than 30% and leads to ventilation perfusion mismatch[7]. This should be avoided in patients with impaired cardiopulmonary function. Therefore, gasless or LPP techniques should be recommended in these patients.
Gasless laparoscopic colorectal surgery was reported to be feasible in several studies[26,27]. However, studies of laparoscopic colorectal surgery with LPP are scant, which is possibly due to the restricted operative field. Compared with LPP or AWL alone, the combination of LPP and AWL may be a more appropriate technique with less adverse hemodynamic and respiratory alterations for laparoscopic TME. This was proved by the stable intraoperative monitoring indices, even in patients with ASA III status, although the number of patients was small. In the present study, most of the patients were in ASA I and II status. Further studies are expected to confirm the superiority of this approach in patients with ASA III and IV status.
The most obvious disadvantage of LPP and gasless techniques is limited exposure in the operative field. Based on our experience, the operative field provided by LPP combined with AWL was less optimal than that with SPP, but acceptable for laparoscopic TME in most patients. However, there were some difficulties in exposing and dissecting the IMA with a pneumoperitoneum of 6 mmHg, especially in obese patients. We increased the pressure to 8-10 mmHg and obtained better exposure of the IMA, and then decreased the pressure back to 6 mmHg after dissection.
Two alternative methods were used to improve exposure of the operative field in obese patients. A second needle was inserted 3 cm above the umbilical level. A better operative field was obtained, but surgery was more difficult due to frequent collisions of the laparoscopic instruments with the scaffold and lifting arms. We also used the method reported by Park et al[19], which was feasible, and exposure was improved when the camera port was lifted up. However, the operative field provided by the assistant was unstable. Therefore, we recommend that the pressure should be increased to 8-10 mmHg when there is difficulty in exposing and dissecting the IMA. No obvious changes in heart rate, blood pressure and paw airway pressure were observed during the short operating time.
Another major concern of LPP with AWL was the prolonged operative time and the accompanying increase in CO2 absorption. Installation of the AWL device and inferior exposure of the operative field may result in longer operative time. During surgery, only approximately 5 min was needed to assemble the AWL system. The mean operative time was comparable to surgery with SPP[21,22]. The operative time may be longer for less skillful surgeons. However, CO2 absorption will not increase due to slow absorption in the case of low pressure. It is possible that postoperative pain may increase due to the subcutaneous insertion of steel needles. However, our patients did not complain of pain at the insertion site, which may have been masked by pain from ports and the assisted incisions.
The major limitation of this study was that it was an observational study and restricted to a small number of patients. A large, well-controlled comparative study with open or standard-pressure laparoscopic TME would be helpful in providing stronger evidence. Another obvious limitation was that most patients in the present study were in ASA I and II status. Patients with compromised cardiopulmonary reserve should be enrolled in further studies to draw more convincing conclusions.
Pneumoperitoneum with carbon dioxide (CO2) is the conventional method of creating a workspace in laparoscopic surgery. Standard-pressure pneumoperitoneum (SPP; 12-15 mmHg) has been reported to result in lower respiratory compliance, increased paw airway pressure, enhanced venous stasis, reduced portal venous pressure and impaired cardiac function.
Low-pressure pneumoperitoneum (LPP) and abdominal wall lift (AWL) have been proposed as alternative approaches to SPP to avoid adverse cardiopulmonary effects. However, the operative field with these techniques is less optimal with increased technical difficulties.
In order to obtain adequate visualization, we combined LPP with AWL and initially used this technique in a case of laparoscopic single-site cholecystectomy, and the surgery was performed successfully. For laparoscopic colorectal surgery which requires sufficient exposure of the lower abdomen, a head-down or Trendelenburg position is necessary. SPP combined with this kind of position significantly influences patients’ cardiopulmonary function. Therefore, we decided to find out whether LPP with AWL technique can take the place of SPP in laparoscopic total mesorectal excision (TME) for rectal cancer.
In this study we designed and performed laparoscopic TME for rectal cancer using LPP with AWL, and evaluated the safety and feasibility. The outcomes of this study will guide the application of the new technique in laparoscopic TME and other surgeries in the future.
From November 2015 to July 2017, 26 patients underwent laparoscopic TME for rectal cancer using LPP (6-8 mmHg) with subcutaneous AWL in Qilu Hospital of Shandong University, Jinan, China. Clinical data regarding patients’ demographics, intraoperative monitoring indices, operation-related indices and pathological outcomes were prospectively collected and analyzed.
Laparoscopic TME was performed in 26 cases (14 anterior resection and 12 abdominoperineal resection) successfully without conversion to open or laparoscopic surgery with SPP. Intraoperative monitoring showed stable heart rate, blood pressure and paw airway pressure. The number of lymph nodes retrieved, the completeness of TME, and the circumferential and mean distance to the distal margin were comparable with those reported in studies using SPP. There was no positive circumferential or distal resection margin. No local recurrence was observed during a median follow-up period of 11.96 ± 5.55 mo (range: 5-23 mo). Our preliminary experience indicated that LPP with AWL was safe and provided a satisfactory workspace for TME.
LPP combined with AWL is safe and feasible for laparoscopic TME. The technique can provide satisfactory exposure of the operative field and result in stable operative monitoring indexes. It should be considered as an alternative approach to SPP in patients undergoing laparoscopic TME.
Further studies are required to confirm the superiority of LPP with AWL over SPP in preservation of cardiopulmonary function, especially in patients with American Society of Anesthesiologists III and IV status. A prospective clinical trial study should be the best method for the future research.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Goldaracena N, Snowdon VK, Yukihiko T S- Editor: Wang XJ L- Editor: Filipodia E- Editor: Huang Y
| 1. | Wirth S, Biesemann A, Spaeth J, Schumann S. Pneumoperitoneum deteriorates intratidal respiratory system mechanics: an observational study in lung-healthy patients. Surg Endosc. 2017;31:753-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Nguyen NT, Cronan M, Braley S, Rivers R, Wolfe BM. Duplex ultrasound assessment of femoral venous flow during laparoscopic and open gastric bypass. Surg Endosc. 2003;17:285-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 49] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | Jakimowicz J, Stultiëns G, Smulders F. Laparoscopic insufflation of the abdomen reduces portal venous flow. Surg Endosc. 1998;12:129-132. [PubMed] |
| 4. | Meininger D, Byhahn C, Bueck M, Binder J, Kramer W, Kessler P, Westphal K. Effects of prolonged pneumoperitoneum on hemodynamics and acid-base balance during totally endoscopic robot-assisted radical prostatectomies. World J Surg. 2002;26:1423-1427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Dexter SP, Vucevic M, Gibson J, McMahon MJ. Hemodynamic consequences of high- and low-pressure capnoperitoneum during laparoscopic cholecystectomy. Surg Endosc. 1999;13:376-381. [PubMed] |
| 6. | Nguyen NT, Wolfe BM. The physiologic effects of pneumoperitoneum in the morbidly obese. Ann Surg. 2005;241:219-226. [PubMed] |
| 7. | Neudecker J, Sauerland S, Neugebauer E, Bergamaschi R, Bonjer HJ, Cuschieri A, Fuchs KH, Jacobi Ch, Jansen FW, Koivusalo AM, Lacy A, McMahon MJ, Millat B, Schwenk W. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. Surg Endosc. 2002;16:1121-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 423] [Cited by in RCA: 379] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 8. | Sroussi J, Elies A, Rigouzzo A, Louvet N, Mezzadri M, Fazel A, Benifla JL. Low pressure gynecological laparoscopy (7mmHg) with AirSeal® System versus a standard insufflation (15mmHg): A pilot study in 60 patients. J Gynecol Obstet Hum Reprod. 2017;46:155-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 9. | Sandhu T, Yamada S, Ariyakachon V, Chakrabandhu T, Chongruksut W, Ko-iam W. Low-pressure pneumoperitoneum versus standard pneumoperitoneum in laparoscopic cholecystectomy, a prospective randomized clinical trial. Surg Endosc. 2009;23:1044-1047. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Schietroma M, Carlei F, Cecilia EM, Piccione F, Sista F, De Vita F, Amicucci G. A prospective randomized study of systemic inflammation and immune response after laparoscopic nissen fundoplication performed with standard and low-pressure pneumoperitoneum. Surg Laparosc Endosc Percutan Tech. 2013;23:189-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Madsen MV, Istre O, Staehr-Rye AK, Springborg HH, Rosenberg J, Lund J, Gätke MR. Postoperative shoulder pain after laparoscopic hysterectomy with deep neuromuscular blockade and low-pressure pneumoperitoneum: A randomised controlled trial. Eur J Anaesthesiol. 2016;33:341-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 12. | Schietroma M, Pessia B, Stifini D, Lancione L, Carlei F, Cecilia EM, Amicucci G. Effects of low and standard intra-abdominal pressure on systemic inflammation and immune response in laparoscopic adrenalectomy: A prospective randomised study. J Minim Access Surg. 2016;12:109-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Özdemir-van Brunschot DMD, Scheffer GJ, van der Jagt M, Langenhuijsen H, Dahan A, Mulder JEEA, Willems S, Hilbrands LB, Donders R, van Laarhoven CJHM. Quality of Recovery After Low-Pressure Laparoscopic Donor Nephrectomy Facilitated by Deep Neuromuscular Blockade: A Randomized Controlled Study. World J Surg. 2017;41:2950-2958. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 14. | Alijani A, Cuschieri A. Abdominal wall lift systems in laparoscopic surgery: gasless and low-pressure systems. Semin Laparosc Surg. 2001;8:53-62. [PubMed] |
| 15. | Uemura N, Nomura M, Inoue S, Endo J, Kishi S, Saito K, Ito S, Nakaya Y. Changes in hemodynamics and autonomic nervous activity in patients undergoing laparoscopic cholecystectomy: differences between the pneumoperitoneum and abdominal wall-lifting method. Endoscopy. 2002;34:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Galizia G, Prizio G, Lieto E, Castellano P, Pelosio L, Imperatore V, Ferrara A, Pignatelli C. Hemodynamic and pulmonary changes during open, carbon dioxide pneumoperitoneum and abdominal wall-lifting cholecystectomy. A prospective, randomized study. Surg Endosc. 2001;15:477-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 118] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 17. | Chiu AW, Chang LS, Birkett DH, Babayan RK. The impact of pneumoperitoneum, pneumoretroperitoneum, and gasless laparoscopy on the systemic and renal hemodynamics. J Am Coll Surg. 1995;181:397-406. [PubMed] |
| 18. | Zhang G, Liu S, Yu W, Wang L, Liu N, Li F, Hu S. Gasless laparoendoscopic single-site surgery with abdominal wall lift in general surgery: initial experience. Surg Endosc. 2011;25:298-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Park IJ, Kim SH, Joh YG, Hahn KY. Laparoscopic colorectal surgery using low-pressure pneumoperitoneum combined with abdominal wall lift by placement of anchoring sutures around the camera port. Surg Endosc. 2006;20:956-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Denost Q, Adam JP, Pontallier A, Celerier B, Laurent C, Rullier E. Laparoscopic total mesorectal excision with coloanal anastomosis for rectal cancer. Ann Surg. 2015;261:138-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Liang JT, Cheng JC, Huang KC, Lai HS, Sun CT. Comparison of tumor recurrence between laparoscopic total mesorectal excision with sphincter preservation and laparoscopic abdominoperineal resection for low rectal cancer. Surg Endosc. 2013;27:3452-3464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Kim MJ, Park SC, Park JW, Chang HJ, Kim DY, Nam BH, Sohn DK, Oh JH. Robot-assisted Versus Laparoscopic Surgery for Rectal Cancer: A Phase II Open Label Prospective Randomized Controlled Trial. Ann Surg. 2018;267:243-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 233] [Article Influence: 38.8] [Reference Citation Analysis (0)] |
| 23. | Martínez-Pérez A, Carra MC, Brunetti F, de’Angelis N. Pathologic Outcomes of Laparoscopic vs Open Mesorectal Excision for Rectal Cancer: A Systematic Review and Meta-analysis. JAMA Surg. 2017;152:e165665. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 120] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 24. | Nagai H, Kondo Y, Yasuda T, Kasahara K, Kanazawa K. An abdominal wall-lift method of laparoscopic cholecystectomy without peritoneal insufflation. Surg Laparosc Endosc. 1993;3:175-179. [PubMed] |
| 25. | Hashimoto D, Nayeem SA, Kajiwara S, Hoshino T. Laparoscopic cholecystectomy: an approach without pneumoperitoneum. Surg Endosc. 1993;7:54-56. [PubMed] |
| 26. | Jiang JK, Chen WS, Yang SH, Lin TC, Lin JK. Gasless laparoscopy-assisted colorectal surgery. Surg Endosc. 2001;15:1093-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |