Published online Jul 28, 2017. doi: 10.3748/wjg.v23.i28.5253
Peer-review started: February 9, 2017
First decision: April 21, 2017
Revised: May 4, 2017
Accepted: June 12, 2017
Article in press: June 12, 2017
Published online: July 28, 2017
Processing time: 174 Days and 17.2 Hours
A 65-year-old man with cT1bN0M0 stage I middle thoracic esophageal cancer underwent subtotal esophagectomy and gastric tube reconstruction through the posterior mediastinal route after preoperative carbon-ion radiotherapy and chemotherapy in a clinical trial. Anastomotic leakage occurred, but it spontaneously improved. At six months after the operation, he was rehospitalized with a cough and dysphagia. An esophago-bronchiole fistula and stenosis of the gastric tube were observed. He first underwent stent placement in the gastric tube. Two weeks later, the syringeal epithelium was burned by argon plasma coagulation after stent removal. Endoscopic occlusion was then performed for the fistula with two guidewire-assisted silicone spigots. Two weeks later, he was discharged on an oral diet, and he has not developed recurrence of the fistula or cancer for three years. This is the first report of endoscopic occlusion with a guidewire-assisted silicone spigot through the esophagus.
Core tip: Anastomotic leakage, which is a complication of esophagectomy, sometimes causes a refractory fistula. An esophago-bronchiole fistula (EBF) is a relatively rare but serious complication. We performed endoscopic occlusion using an endobronchial Watanabe spigot (EWS), a type of silicone bronchial blocker that is widely used in the respiratory field to treat pulmonary air leak, hemoptysis and bronchopleural fistula. We herein report a new and unique technique using the EWS to close a refractory EBF after esophagectomy. This report is the first to show that endoscopic occlusion using the EWS through the esophagus can simply and safely repair a refractory fistula.
- Citation: Uesato M, Kono T, Akutsu Y, Murakami K, Kagaya A, Muto Y, Nakano A, Aikawa M, Tamachi T, Amagai H, Arasawa T, Muto Y, Matsubara H. Endoscopic occlusion with silicone spigots for the closure of refractory esophago-bronchiole fistula after esophagectomy. World J Gastroenterol 2017; 23(28): 5253-5256
- URL: https://www.wjgnet.com/1007-9327/full/v23/i28/5253.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i28.5253
Anastomotic leakage, which is a complication of esophagectomy, sometimes causes a refractory fistula[1]. An esophago-bronchiole fistula (EBF) is a relatively rare but serious complication. Conventional therapy, such as hemoclipping, fibrin glue and stenting, are often performed[2-4]. However, surgical repair may be ultimately performed. We herein report a new and unique technique using an endobronchial Watanabe spigot (EWS) through the esophagus to close a refractory EBF after esophagectomy.
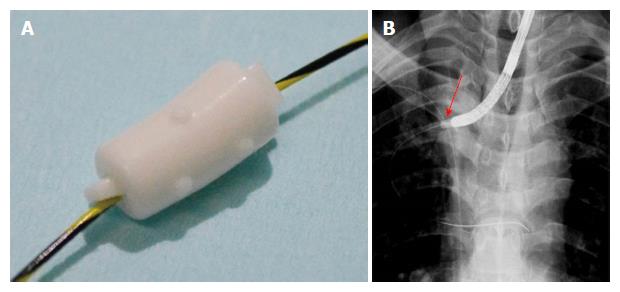
A 65-year-old man with cT1bN0M0 stage I middle thoracic esophageal cancer underwent subtotal esophagectomy and gastric tube reconstruction through the posterior mediastinal route after preoperative carbon-ion radiotherapy and chemotherapy in a clinical trial. Anastomotic leakage occurred, but it spontaneously improved. There was no residual cancer in the resected specimen. At six months after the operation, he was rehospitalized with a cough and dysphagia. An EBF at the right B1 bronchiole and stenosis of the gastric tube were observed (Figure 1). The region of the anastomotic leakage and the region of EBF were same. The patient first underwent full-covered stent (Flexella-J; ELLA-CS, s.r.o., Hradec Kralove, Czech Republic) placement in the gastric tube under fluoroscopic guidance. Two weeks later, we recognized the release of the stenosis with the persistent EBF after the stent removal. Hemoclipping was performed for the fistula but failed. We next burned the syringeal epithelium by argon plasma coagulation (Figure 2). At the same time, endoscopic occlusion was performed. Under fluoroscopic guidance, a 0.035-inch guidewire (Jagwire; Boston Scientific, Natick, MA, United States) was inserted into the EBF through an ultrathin endoscope (EG-580NW; FUJIFILM, Tokyo, Japan). After the endoscope was removed, a 5-mm endobronchial Watanabe spigot (EWS; Novatech, La Ciotat, France) was penetrated through its long axis using the guidewire (Figure 3A). After inserting a snaretube (MAJ-10; OLYMPUS, Tokyo, Japan) to the endoscope channel, the guidewire was retrogradely passed to the endoscope through the tube. Under fluoroscopic and endoscopic guidance, the EWS was wedged into the EBF (Figure 3B). Another 7-mm EWS was additionally inserted in a similar manner. The image just after the insertion showed the fistula occluded by the EWS (Figure 4A and B). Two weeks later, he was discharged on an oral diet, and he has not developed recurrence of the fistula or cancer for three years (Figure 5A-C).
A new and unique technique using a guidewire-assisted EWS through the esophagus proved useful for closing a refractory EBF after esophagectomy.
The patient in the present case had not only an EBF but also stenosis of the upper gastric tube. Upper gastric tube is the periphery of the blood flow, had approximately 5 cm stenosis. We therefore suspect that the cause of the fistula was the anastomotic leakage occurred by ischemia. A refractory fistula commuting with the airway system often causes pneumonia and respiratory failure. A number of minimally invasive treatments have been proposed for treating a refractory fistula, including hemoclipping[2], stenting[4], polyglycolic acid sheets and fibrin glue[3] and over-the-scope clipping[4]. In addition, since these therapies failed in the present case, surgery with a musculo-cutaneous flap was considered.
Before performing invasive treatment, we attempted endoscopic occlusion with an EWS, a type of silicone bronchial blocker[5] that is widely used in the respiratory field to treat pulmonary air leak[6], hemoptysis[7] and bronchopleural fistula[8]. We selected EWS occlusion through the esophagus to blockade the nearest portion of the EBF. The spigot is typically grasped with forceps and inserted into the affected bronchus using a flexible bronchoscope[5]. However, because fistulas of the digestive system are more irregular than those in the tracheal route, it can be difficult to insert the EWS using forceps. Therefore, in the present case, a guidewire was first inserted, and then the EWS was placed along the guidewire.
In 2003, Miyazawa et al[9] first reported the “Push and Slide” method in Japanese. Recently, the usefulness of endobronchial occlusion for massive hemoptysis with a guidewire-assisted custom-made silicone spigot was reported[7]. We recommend this method, as the EWS can be inserted precisely. There are three kinds of size in the EWS (short axis/long axis: 5/8.5 mm, 6/10.5, 7/12.5)[6]. A fistula to the respiratory tract exceeding its size seems to be out of the indication. In an esophago-bronchial or tracheal fistula, the spigot may fall into the airway. Therefore, the best indication of the fistula could be occluded by the EWS is an esophago-bronchiole fistula has the length longer than approximately 10 mm. In addition, coagulating the syringeal epithelium by argon plasma coagulation before the EWS insertion might accelerate the occlusion of the EBF[2].
In conclusion, we successfully performed EWS occlusion through the esophagus for an EBF without complications. We therefore recommend EWS occlusion as a potential treatment for a refractory EBF after esophagectomy. This is the first report of the successful closure of a refractory fistula, although EWS occlusion through the gastrointestinal tract needs further exploration.
A 65-year-old man with esophageal cancer underwent subtotal esophagectomy and gastric tube reconstruction. At six months after the operation, he was rehospitalized with a cough and dysphagia.
An esophago-bronchiole fistula was observed.
Aspiration pneumonitis.
An esophago-bronchiole fistula at the right B1 bronchiole and stenosis of the gastric tube were observed.
He first underwent stent placement in the gastric tube. Two weeks later, the syringeal epithelium was burned by argon plasma coagulation after stent removal. Endoscopic occlusion was then performed for the fistula with two guidewire-assisted silicone spigots.
A new and unique technique using a guidewire-assisted endobronchial Watanabe spigot through the esophagus proved useful for closing a refractory esophago-bronchiole fistula after esophagectomy.
The authors showed a new and unique technique using a guidewire-assisted endobronchial Watanabe spigot through the esophagus proved useful for closing a refractory esophago-bronchial fistula after esophagectomy. The technique is new and original. The text is well-written.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Sugimura K, Tsubosa Y S- Editor: Gong ZM L- Editor: A E- Editor: Li D
| 1. | Yamana I, Takeno S, Yamada T, Sato K, Hashimoto T, Yamashita Y. The Risk Factors for Refractory Fistula after Esophagectomy with Gastric Tube Reconstruction in Patients with Esophageal Cancer. Dig Surg. 2017;34:18-24. [PubMed] [DOI] [Full Text] |
| 2. | van Bodegraven AA, Kuipers EJ, Bonenkamp HJ, Meuwissen SG. Esophagopleural fistula treated endoscopically with argon beam electrocoagulation and clips. Gastrointest Endosc. 1999;50:407-409. [PubMed] [DOI] [Full Text] |
| 3. | Matsuura N, Hanaoka N, Ishihara R, Sugimura K, Motoori M, Miyata H, Yano M. Polyglycolic acid sheets for closure of refractory esophago-pulmonary fistula after esophagectomy. Endoscopy. 2016;48 Suppl 1 UCTN:E78-E79. [PubMed] [DOI] [Full Text] |
| 4. | Bertani H, Grande G, Mirante VG, Franco I, Mangiafico S, Manta R, Conigliaro RL. Multimodal endoscopic treatment of primary esophago-pleural fistula. Endoscopy. 2016;48:E298-E299. [PubMed] |
| 5. | Watanabe Y, Matsuo K, Tamaoki A, Kamoto R, Hiraki S. Bronchial occlusion with Endobronchial Watanabe Spigot. J Bronchol. 2003;10:264-267. [DOI] [Full Text] |
| 6. | Sasada S, Tamura K, Chang YS, Okamoto N, Matsuura Y, Tamiya M, Suzuki H, Uehara N, Kobayashi M, Hirashima T. Clinical evaluation of endoscopic bronchial occlusion with silicone spigots for the management of persistent pulmonary air leaks. Intern Med. 2011;50:1169-1173. [PubMed] [DOI] [Full Text] |
| 7. | Coiffard B, Laroumagne S, Plojoux J, Astoul P, Dutau H. Endobronchial occlusion for massive hemoptysis with a guidewire-assisted custom-made silicone spigot: a new technique. J Bronchology Interv Pulmonol. 2014;21:366-368. [PubMed] [DOI] [Full Text] |
| 8. | Dalar L, Kosar F, Eryuksel E, Karasulu L, Altin S. Endobronchial Watanabe spigot embolisation in the treatment of bronchopleural fistula due to tuberculous empyema in intensive care unit. Ann Thorac Cardiovasc Surg. 2013;19:140-143. [PubMed] [DOI] [Full Text] |
| 9. | Miyazawa H, Shinno H, Noto H, Fujisaka S, Taniguchi H, Izumi S. Bronchial Occlusion Using EWS (Endoscopic Watanabe Spigot) by Push & Slide Method and a Pilot Study of Bronchoscopic Lung Volume Reduction Using EWS for Severe Emphysema. J Jpn Soc Respir Endosc. 2003;25:695-703. [DOI] [Full Text] |