Published online Jun 14, 2017. doi: 10.3748/wjg.v23.i22.4127
Peer-review started: January 12, 2017
First decision: March 3, 2017
Revised: March 14, 2017
Accepted: April 12, 2017
Article in press: April 12, 2017
Published online: June 14, 2017
Processing time: 155 Days and 0.4 Hours
We present a case of a 56-year-old man with 3 synchronous gastric tumors. The patient presented with melena, and 3 gastric abnormalities were detected on gastroduodenoscopic examination, including a small ulcerative lesion in the gastric antrum, a submucosal mass in the gastric body, and severe erosion in the fundus. Histological examination of biopsy samples yielded respective diagnoses of gastric adenocarcinoma, gastritis, and mucosa-associated lymphoid tissue (MALT) lymphoma. The patient first received medication to eradicate any underlying Helicobacter pylori infection, which might have been a cause of the MALT lymphoma. Four weeks later, after examination of repeat biopsy samples revealed that the MALT lymphoma had resolved, the patient underwent subtotal gastrectomy. Further histological examination of resected tissue confirmed the antrum lesion as adenocarcinoma and the body lesion as schwannoma. To our knowledge, this is the first reported case of synchronous triple primary gastric adenocarcinoma, MALT lymphoma, and schwannoma.
Core tip: Synchronous occurrence of two types of gastric tumor is relatively well described, but this is the first report of synchronous triple gastric adenocarcinoma, mucosa-associated lymphoid tissue (MALT) lymphoma, and schwannoma. Consideration of the possible underlying involvement of Helicobacter pylori in MALT lymphoma and preoperative treatment with appropriate medication allowed performance of subtotal gastrectomy and a successful outcome.
- Citation: Choi KW, Joo M, Kim HS, Lee WY. Synchronous triple occurrence of MALT lymphoma, schwannoma, and adenocarcinoma of the stomach. World J Gastroenterol 2017; 23(22): 4127-4131
- URL: https://www.wjgnet.com/1007-9327/full/v23/i22/4127.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i22.4127
The most frequent diagnosis of tumor of the stomach is adenocarcinoma (90%-95%), followed by lymphoma, gastrointestinal stromal tumor (GIST), and carcinoid tumor. Synchronous occurrence of two types of tumor in the stomach is relatively well known. Here, we present an extremely rare case of synchronous gastric adenocarcinoma, mucosa-associated lymphoid tissue (MALT) lymphoma, and schwannoma in a 56-year-old man in Korea.
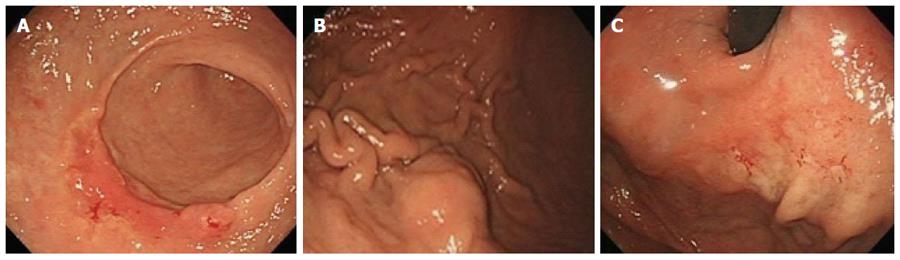
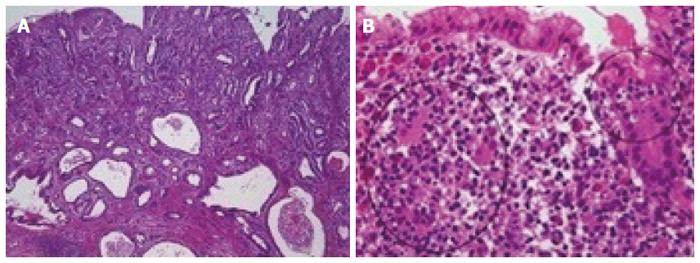
A 56-year-old male visited to our clinic with melena. Apart from the presence of diabetes, he had no other remarkable symptom or past medical history. There were no specific findings in physical examination except for obesity (body mass index, 32). All laboratory results, including tumor markers, were in normal range. Gastroduodenoscopy showed slightly raised ulcer on the antral anterior wall. Additional findings included a positive rolling sign in the mid-body suggestive of a submucosal lesion and a diffuse erythematous lesion in the fundus area, and these areas were also biopsied (Figure 1). A computed tomography scan of the abdomen showed an ovoid homogeneous 2 cm × 2 cm mass at the greater curvature of the mid-body and mildly enlarged perigastric lymph nodes. Positron emission tomography - computed tomography showed no evidence of any other lymphoid involvement. Histological examination of the antral and fundic biopsy samples yielded respective diagnoses of moderately differentiated adenocarcinoma and low-grade MALT lymphoma with plasmacytic differentiation (Figure 2).
The patient was first prescribed medication to eradicate any underlying Helicobacter pylori (H. pylori) infection, which might have been a causative factor in the MALT lymphoma, and examination of repeat biopsy obtained at the fundus after 4 wk medication confirmed that the MALT lymphoma had resolved. The patient was then referred for surgical intervention. At laparotomy, the patient underwent radical subtotal gastrectomy with gastrojejunostomy. During gastrectomy, a well-defined nodular lesion measuring 2 cm × 2 cm was palpated in the greater curvature 5 cm proximal to the adenocarcinoma.
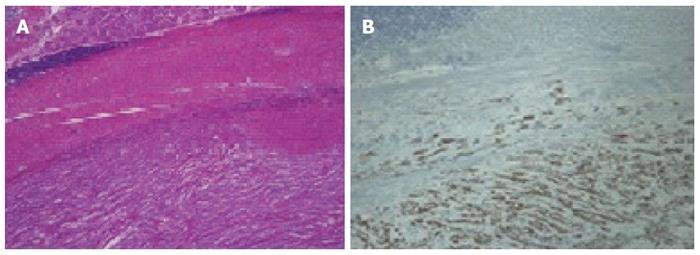
Histological examination of the partial stomach showed the presence of an early gastric cancer consisting of a moderately differentiated intestinal-type adenocarcinoma located in the antrum and measuring 3.2 cm × 2.5 cm. The tumor was infiltrating into the deep submucosa of the antrum. There was no lymph node metastasis in 17 retrieved nodes. The final pathologic stage for gastric adenocarcinoma was pT1bN0M0, p-Stage IA (American Joint Committee on Cancer 7th edition). Histological examination of hematoxylin and eosin-stained sections of the other submucosal tumor revealed that it consisted of spindle cells covered by a smooth muscle layer, lymphoid cuffs, and fundic-type glands. On immunohistochemical analysis, this submucosal tumor showed strong positivity for S-100 and negative expression for c-Kit. This immunostaining pattern differentiates gastrointestinal schwannoma from GIST (Figure 3).
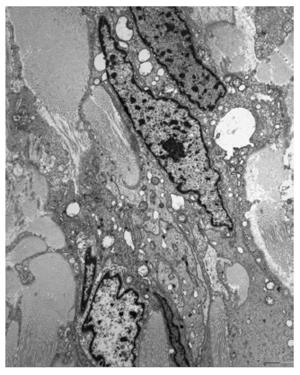
Electron microscopic examination of ultrathin sections of the submucosal tumor revealed sheets of elongated cells with numerous complex cytoplasmic processes. The cytoplasmic membrane was completely covered with external lamina. The nucleus had irregular margins and a heterochromatic chromatin pattern, and the perikaryal cytoplasm contained several mitochondria, rough endoplasmic reticulum, ribosomes, and many lysosomes. Hence, a final diagnosis of schwannoma was made (Figure 4).
The patient’s postoperative period was uneventful and he was discharged in good health. Follow-up visits, including endoscopy every 6 mo, for up to 2 yr after operation were unremarkable.
Occurrence of two types of primary gastric neoplasm is relatively well known, but no reports have been published regarding the simultaneous presence of gastric adenocarcinoma, MALT lymphoma, and schwannoma.
Gastric adenocarcinoma accounts for more than 90% of all malignant gastric tumors and may co-exist with synchronous tumors of a different histologic type, most commonly lymphoma.
Primary gastric lymphoma occurs in 5% of gastric malignancies and their worldwide incidence is increasing. Primary gastric lymphoma is mostly non-Hodgkin lymphoma. Diffuse large B cell and marginal zone B cell type are the most common subtypes. The pathogenesis is often related to H. pylori infection[1]. Since Rabinovitch et al[2] published the first case in 1952, 56 cases of simultaneous occurrence of gastric adenocarcinoma and gastric lymphoma have been reported. In that series, gastric lymphoma was mainly MALT type (69.6%) or low grade (87.2%), the correlation between H. pylori and MALT lymphoma was 86%/72% in the Eastern and Western cases[3].
Gastric adenocarcinoma and gastric MALT lymphoma are considered to be one of the results of H. pylori infection. Gastric cancer can occur in about 1%-2% of H. pylori infection cases, and the risk is nine times higher than in patients without H. pylori infection. In addition, H. pylori infection is highly correlated with gastric MALT lymphoma and is found as a low-grade type MALT lymphoma in over 90% of cases[4]. At present, the most widely accepted initial therapy for localized low-grade MALT lymphoma is aimed at the eradication of H. pylori infection, with regimens combining antibiotics and proton-pump inhibitors. Many reports have confirmed the efficacy of antibiotic therapy and showed long-term remission in 60%-100% of patients with localized H. pylori-positive MALT lymphoma[5].
In our patient, we decided to treat the MALT lymphoma first by prescribing medication for the eradication of H. pylori organisms to avoid total gastrectomy. After 4 wk, repeat biopsy was conducted at the fundic site and we confirmed that the MALT lymphoma had resolved. Subsequently, the patient underwent radical subtotal gastrectomy, which included removal of the submucosal tumor in the mid-body. The final pathologic findings were moderately differentiated intestinal-type adenocarcinoma (submucosal invasion without regional lymph node metastasis) and schwannoma, and follow-up visits up to 2 y after operation were unremarkable.
According to Nakamura's study[6], the survival rate of patients with synchronous gastric adenocarcinoma and gastric lymphoma was similar to survival rate of gastric adenocarcinoma alone and was significantly lower than survival rate of gastric lymphoma alone.
Schwannoma is a rare gastrointestinal mesenchymal tumor. The most common site for schwannoma in the gastrointestinal tract is the stomach, followed by the colon. There are some histological differences between gastric schwannoma and soft-tissue schwannoma. Unlike soft tissue schwannoma, encapsulation, nuclear palisading and vascular hyalinization are rare in gastric schwannoma[7]. Gastric schwannoma seems to have a good prognosis without recurrence and metastasis. As for simultaneous occurrences of schwannoma with other types of gastric cancer, only three cases have been reported prior to 2015[8].
In conclusion, synchronous triple gastric adenocarcinoma, MALT lymphoma, and schwannoma has not been reported previously in the literature. H. pylori eradication and surgery are the mainstay treatment. Further biologic and genetic studies will be required to explain the simultaneous development of tumors of different histotypes.
A 56-year-old man presented to our hospital with melena and three gastric abnormalities were detected on gastroduodenoscopic examination.
Mucosa-associated lymphoid tissue (MALT) lymphoma, adenocarcinoma, and submucosal tumor in stomach.
Carcinoid tumor, primary lymphoma, gastrointestinal stromal tumor.
All laboratory results were within normal limits.
Gastroduodenoscopic examination showed a small ulcerative lesion in the gastric antrum, a submucosal mass in the gastric body, and severe erosion in the fundus. CT showed an ovoid homogeneous 2 cm × 2 cm mass at the greater curvature of the mid-body and mildly enlarged perigastric lymph nodes.
MALT lymphoma, adenocarcinoma, schwannoma.
Antibiotics treatment and radical subtotal gastrectomy.
Synchronous occurrence of two types of tumor in the stomach is relatively well known. This is rare case of synchronous triple tumors in stomach.
MALT lymphoma is a form of lymphoma involving the MALT, frequently of the stomach. Gastric schwannoma is a benign nerve sheath tumor composed of Schwann cells.
Further biologic and genetic studies will be required to explain the simultaneous development of tumors of different histotypes.
It is a well written article, a case report about synchronous triple primary gastric adenocarcinoma, MALT lymphoma, and schwannoma.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Chetty R, Wu DC, Velenik V S- Editor: Ma YJ L- Editor: Filipodia E- Editor: Wang CH
| 1. | Ferrucci PF, Zucca E. Primary gastric lymphoma pathogenesis and treatment: what has changed over the past 10 years? Br J Haematol. 2007;136:521-538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Rabinovitch J, Pines B, Grayzel D. Coexisting lymphosarcoma and ulcer-carcinoma of the stomach. AMA Arch Surg. 1952;64:185-191. [PubMed] |
| 3. | Hamaloglu E, Topaloglu S, Ozdemir A, Ozenc A. Synchronous and metachronous occurrence of gastric adenocarcinoma and gastric lymphoma: A review of the literature. World J Gastroenterol. 2006;12:3564-3574. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 33] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Kaffes A, Hughes L, Hollinshead J, Katelaris P. Synchronous primary adenocarcinoma, mucosa-associated lymphoid tissue lymphoma and a stromal tumor in a Helicobacter pylori-infected stomach. J Gastroenterol Hepatol. 2002;17:1033-1036. [PubMed] |
| 5. | Wotherspoon AC, Doglioni C, Diss TC, Pan L, Moschini A, de Boni M, Isaacson PG. Regression of primary low-grade B-cell gastric lymphoma of mucosa-associated lymphoid tissue type after eradication of Helicobacter pylori. Lancet. 1993;342:575-577. [PubMed] |
| 6. | Nakamura S, Aoyagi K, Iwanaga S, Yao T, Tsuneyoshi M, Fujishima M. Synchronous and metachronous primary gastric lymphoma and adenocarcinoma: a clinicopathological study of 12 patients. Cancer. 1997;79:1077-1085. [PubMed] |
| 7. | Voltaggio L, Murray R, Lasota J, Miettinen M. Gastric schwannoma: a clinicopathologic study of 51 cases and critical review of the literature. Hum Pathol. 2012;43:650-659. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 134] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 8. | Yang LH, Wang JO, Ma S, Zhu Z, Sun JX, Ding SL, Li G, Xu HT, Wang L, Dai SD. Synchronous of gastric adenocarcinoma and schwannoma: report of a case and review of literatures. Int J Clin Exp Pathol. 2015;8:1041-1045. [PubMed] |