Published online Apr 14, 2017. doi: 10.3748/wjg.v23.i14.2483
Peer-review started: February 7, 2017
First decision: February 23, 2017
Revised: March 8, 2017
Accepted: March 20, 2017
Article in press: March 20, 2017
Published online: April 14, 2017
Processing time: 66 Days and 21.9 Hours
Conventional therapies for inflammatory bowel diseases (IBD) involve combinations of pharmacologic agents such as aminosalicylates, azathioprine, and corticosteroids. Recently, the therapeutic scenario has been heavily increased by the introduction of agents including monoclonal antibodies targeted to specific proinflammatory cytokines, to adhesion molecules, and the induction of anti-inflammatory cytokines and T-cell activation. However, the use of these drugs is accompanied by a certain number of side effects, with some of them being quite severe, rising concerns about the safety profile. Furthermore, the cost of these emerging therapeutic strategies is significant , considering the increasing incidence and the chronic trend of IBD. Nutraceuticals is a broad term used to describe any product derived from food sources claiming extra health benefits beyond the intrinsic nutritional value found in foods. The beneficial effects of nutraceutical compounds in human health have been emerging in the last decades. Although few clinical trials have been performed in IBD patients, nutraceuticals, such as herbal products or vitamins, are generally accepted as safer alternative/supplementation to conventional therapy. In vitro and IBD-animal models studies have shown their involvement in several biological processes, including antioxidant defenses, cell proliferation, gene expression, which could account for a role in the maintenance of the mucosal barrier integrity, the control of the inflammatory pathways and the modulation of the immune response. These data suggest a wide spectrum of positive effects exerted by nutraceuticals, with a high potential for a therapeutic use in humans. In the present review, the beneficial effects of the most investigated nutraceutical compounds in the setting of human IBD are discussed.
Core tip: Current therapies for inflammatory bowel diseases (IBD) include aminosalicylates, azathioprine, corticosteroids and recently clinical management with biologic agents has been implemented. However, safety issue are emerging along with concern about the high cost of these new drugs. Nutraceuticals is a broad term used to describe any product derived from food sources, such as herbal products or vitamins, with extra health benefits beyond the basic nutritional value. Despite few clinical trials in IBD patients, nutraceuticals are generally accepted as safer alternative/supplementation to conventional therapy and the available data support their high potential for therapeutic use in human IBD.
- Citation: Larussa T, Imeneo M, Luzza F. Potential role of nutraceutical compounds in inflammatory bowel disease. World J Gastroenterol 2017; 23(14): 2483-2492
- URL: https://www.wjgnet.com/1007-9327/full/v23/i14/2483.htm
- DOI: https://dx.doi.org/10.3748/wjg.v23.i14.2483
Inflammatory bowel diseases (IBD), including Crohn’s disease (CD) and ulcerative colitis (UC), are a group of idiopathic, chronic and relapsing inflammatory disorders of the gastrointestinal tract, whose incidence and prevalence has been increasing in the last decades[1]. Although the etiology of IBD is still unclear, it is assumed that many interacting components could affect IBD development, including genetic susceptibility, ethnicity, environmental factors, infectious diseases, and dietary habits[2]. At present, the acknowledged pathogenetic mechanisms are featured by immune dysregulation, altered intestinal microflora, oxidative stress, defects in the gastrointestinal mucosal barrier and increased permeability, whose interplay leads to the onset of a state of chronic mucosal inflammation[3]. IBD patients often require lifelong medication, being the main goal of therapy both to induce a clinical remission and then maintain it for a long period of time. Severity and location of the disease account for the choice of therapeutic strategies, but also the awareness of potential side effects. Indeed, the currently approved drugs, such as corticosteroids, immunosuppressants and anti-tumor necrosis factor (TNF)-α antibodies, have been related to the risk of opportunistic infections and malignancies[4]. Furthermore, the course of the disease is often poorly controlled in a significant number of patients and besides conventional therapy, there are now emerging other novel biologic agents[5]. A crucial issue is the cost of these drugs, which are much more expensive than conventional therapy and concerns have arisen about the cost-effective management of IBD[6]. Surgery is the last option in critical patients, but is often associated with short- and long-term complications[7]. A poor adherence to therapy worsens this scenario, suggesting efforts by clinicians in understanding patients’ needs and barriers to achieve a successful management[8]. For all the above mentioned reasons, alternatives for a safer, cheaper, and efficacious approach in managing IBD patients are being sought.
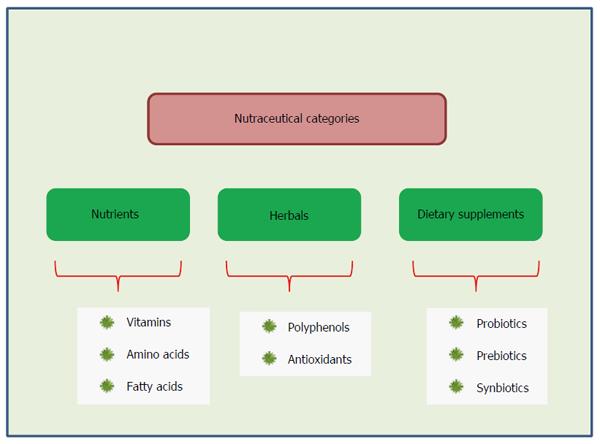
Nutraceutical compounds, such as bioactive peptides, phytochemicals, and omega 3-polyunsaturated fatty acids, are currently under investigation for their helpful activities in IBD[9]. According to the acknowledged definition, nutraceuticals are foods or parts thereof that provides medical or health benefits, including the prevention and/or treatment of a disease. The term “nutraceutical” was coined in 1989 by Stephen DeFelice and combines two words - “nutrient” (a nourishing food component) and “pharmaceutical” (a medical drug)[10]. The definition of nutraceuticals and related products generally depends on the source. They can be classified on the basis of their natural sources, or according their pharmacological conditions, as well as chemical constitution of the products. This means that different way of classification are possible. Chauhan et al[11] proposed that nutraceuticals can be grouped into three broad categories: (1) substances with established nutritional functions, such as vitamins, minerals, amino acids and fatty acids, also defined nutrients; (2) herbs or botanical products as concentrates and extracts, often called herbals; and (3) reagents derived from other sources (e.g., pyruvate, chondroitin sulphate, steroid hormone precursors) serving specific functions, such as sports nutrition, weight-loss supplements and meal replacements, also indicated as dietary supplements (Figure 1). In recent years, use of complementary and alternative medicine (CAM) has spread due to the perceived natural and health benefits and the most commonly used CAM in IBD patients appear to be vitamin supplements and herbal therapies[12]. Previous studies in active IBD and in experimental DSS-colitis have shown that dietary supplements, such as probiotics, fish oil, curcumin and aloe vera, can ameliorate intestinal inflammation[13]. Plant-derived natural compounds carry out their protective and therapeutic effect through different molecular pathways, including anti-inflammatory and immunoregulatory mechanisms, anti-oxidative properties, and modulation of intracellular signaling transduction pathways[14]. Curcumin and green tea supplementation have been reported to be effective in reducing both IBD symptomatology and inflammatory scores, but strong evidence is limited[15]. The aim of this minireview is to describe the more common nutraceutical compounds used in IBD and to comment on recent findings for their possible applications in humans. We did not chosen to discuss data deriving from in vitro or animal studies, and the agents heading each of the four paragraphs represent compounds worthy of note for their use in human clinical trials investigating IBD.
A growing body of evidence documents the use of probiotics and prebiotics in IBD treatment. Probiotics are defined as “live microorganisms which when administered in adequate amounts confer a health benefit on the host”[16]. The human gastrointestinal tract contains about 1014 bacteria, mostly concentrated in the large intestine and named intestinal microflora. It contributes to digestion of nutrients and waste products of metabolism and acts as an important barrier function against pathogens[17]. The triggering of chronic intestinal inflammation seems to depend somehow on the flora. In animal models, resident enteric bacteria are necessary for development of spontaneous colitis[18]. At the same time, a disruption of the fine balance between the host and its microbes is a hallmark of the inflammatory process in the gut[19]. Since this proven involvement of intestinal bacteria in IBD, various attempts have been made to modify the flora with probiotics. Escherichia coli (E. coli) Nissle 1917, S. boulardii, L. casei, L. rhamnosus, Bifidobacterium, represent some of the most studied microorganism in human IBD. In 1997, Malchow evaluated the maintaining remission rates among the probiotic and placebo groups using E. coli Nissle 1917 in CD patients, but no statistically significant difference was found due to the small sample size[20]. A reduction in clinical relapse of CD to 6.25% vs 37.5% was obtained with S. boulardii supplementation over a 6 mo period but a larger subsequent study with the same agent did not confirm these benefits[21,22]. A third study with S. boulardii showed a reduction in the intestinal permeability in the probiotic group, however some concerns arose due to wide variability of intestinal permeability in CD patients and lack of correlation with CD activity index (CDAI) or endoscopic remission[23]. The largest probiotic trials in UC assessed the role of VSL#3, a multibacterial culture for oral use, consisting of the following species of bacteria: B. breve, B. longum, B. infantis, L. acidophilus, L. plantarum, L. paracasei, L. bulgaricus, and S. thermophiles[24]. An Indian multicenter trial showed a 42.9% of VSL#3 patients remission, compared with 15.7% of placebo patients[25], as well as an Italian 8 wk study which showed that VSL#3 was significantly superior to placebo in reducing the disease activity of mild-to-moderate UC. Moreover, VSL#3 improved rectal bleeding and seemed to lower entity of relapsing UC patients, although these parameters did not reach statistical significance due to the high placebo response rate and relatively short duration of the study[26]. Bifidobacteria was successful in maintaining UC remission in a long term trial, showing a 73% remission rate compared with 10% in the placebo group[27]. The probiotic drug E. coli Nissle 1917 shows equivalent efficacy and safety in maintaining remission compared to the gold standard mesalazine in a large cohort of patients with UC. The ability in preventing relapse was confirmed by statistical analysis with both of the PP population and ITT analysis[28]. Similar findings were demonstrated by Rembacken et al[29] in 1999, who reported a 67% of relapse rate in the E. coli Nissle 1917 group compared with 73% in the mesalazine group (P = 0.059). A lot of mechanisms have been proposed to explain the beneficial role of probiotics in IBD, focusing on their ability to colonize the colon and inhibit the growth of pathogenic species[30]. Moreover, probiotics are known to interact with epithelial and immune cells resident in the intestinal mucosa, reinforcing the barrier function and modulating the immune response[31]. Therapeutic modulation of the gut microbiota in IBD also contemplates the use of prebiotics, dietary substances that stimulate the growth and metabolism of protective commensal enteric bacteria, and synbiotics, which are products that contain both probiotics and prebiotics[32]. Hafer et al[33] showed no significant improvement in clinical activity index, endoscopic score or immunohistochemical parameters in CD and UC patients receiving lactulose compared with the control group. A similar failure was observed by the administration of fructo-oligosaccharides in 103 CD patients in a 4 wk trial[34]. A synbiotic consumption was effective in CD patients, ameliorating clinical outcomes and histological findings[35], and also in the UC setting synbiotic administration resulted in a promising outcome[36].
Table 1 summarizes the most relevant randomized controlled trials with probiotics, prebiotics and synbiotics, performed in patients with IBD in the last twenty years.
| Ref. | Treatment | Duration | Subjects (n) | Findings |
| Malchow et al[20] 1997 | E. coli Nissle 1917 | 12 mo | Active CD (28) | Trend toward reduced relapse rate |
| Guslandi[21] 2000 | S. boulardii | 6 mo | Active CD (32) | Significant reduction in relapse rate |
| Bourreille et al[22] 2013 | S. boulardii | 12 mo | Active CD (165) | No significant reduction in relapse rate |
| Garcia Vilela et al[23] 2008 | S. boulardii | 3 mo | Remission CD (34) | Reduction in intestinal permeability |
| Sood et al[25] 2009 | VSL#3 | 12 wk | Active UC (147) | Significant achieved remission |
| Tursi et al[26] 2010 | VSL#3 | 8 wk | Active UC (144) | Significant reduction in disease activity |
| Ishikawa et al[27] 2003 | Bifidobacteria | 12 mo | Remission UC (21) | Significant maintenance of remission |
| Kruis et al[28] 2004 | E. coli Nissle 1917 | 12 mo | Remission UC (327) | Equivalence to mesalazine in remission |
| Rembacken et al[29] 1999 | E. coli Nissle 1917 | 12 mo | Remission UC (166) | Equivalence to mesalazine in remission |
| Hafer et al[33] 2007 | Lactulose | 4 mo | Active CD and UC (31) | No clinical benefits |
| Benjamin et al[34] 2011 | Fructo-oligosaccharides | 4 wk | Active CD (103) | No clinical benefits |
| Steed et al[35] 2010 | B. longum plus inulin/oligofructose mix | 6 mo | Active CD (35) | Significant improvement in CDAI scores |
| Ishikawa et al[36] 2011 | B. breve plus galacto-oligosaccharide | 12 mo | Active UC (41) | Improvement of endoscopic score |
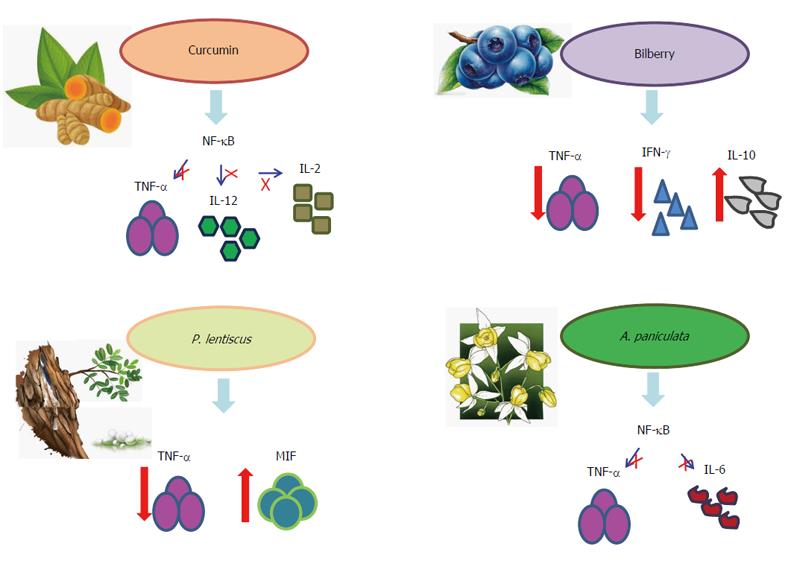
Phytochemicals are a group of nutraceutical compounds derived from plants which hold healthy properties. Benefits from nutraceuticals rich in polyphenols and antioxidants derive from their properties to scavenge free radicals, induce anti-inflammatory responses, maintaining a homeostatic regulation of the gut microbiota, and activate the intestinal T regulatory cells[37]. Phenolic compounds represent the most widely distributed plant secondary metabolites and several studies have investigated their effects on intestinal inflammation, either as pure molecules or as plant extracts, in humans[38]. Curcumin is the principal natural curcuminoid (a class of phenols) found in the plant Curcuma longa, which is commonly used as a spice, food preservative and a coloring agent in foods. Its anti-inflammatory mechanism works mainly through the suppression of the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB)-related inflammatory pathway, with subsequent inhibition of TNF-α, IL-12 and IL-2, thus affecting the immune response modulation and representing a safe and promising agent for treatment of IBD[39]. Curcumin was reported to be effective in inducing remission in IBD patients both in a pilot study and in a multicenter randomized, placebo-controlled, double-blind trial, without producing adverse effects[40,41]. Moreover, curcumin showed a lower relapse rate in UC compared with placebo, supporting its efficacy also as a maintenance therapy[42]. Beside oral administration, curcumin was found to be effective also in enema formulation, as reported by Singla et al[43] in a randomized, double-blind, single-centre pilot study. Of note, the tolerability of oral supplementation with curcumin was assessed in a pediatric IBD population, and did not raise concerns regarding its safety[44]. Aloe vera gel, a plant extract known for medicinal purposes in several cultures for centuries, is one of the common herbal therapies used for IBD, despite a lack of large trials confirming its efficacy[45]. Langmead et al[46] demonstrated the induction of clinical response in UC patients after a four week treatment with orally Aloe vera gel administration, but no significant effects on endoscopic and histological outcomes were found. Flavonoids, which are widely distributed in fruits and vegetables, are included into the polyphenols category. Flavonoid sources as dietary supplement for therapeutic use have been proposed and their mode of action have been documented. Their use in IBD, thus limited in evidences, is intriguing due to the exhibited anti-inflammatory and immunomodulatory properties[47]. Anthocyanins are a class of dietary flavonoids widespread in fruits and flowers, where they are responsible for the blue, purple and red colours. Their anti-oxidant properties, added to a direct interference both with gene expression and receptor-regulated signaling pathways of inflammation, have been recently investigated. During an open label pilot study, UC patients with mild to moderate disease were treated with an anthocyanin-rich bilberry preparation. After 6 wk treatment, endoscopic and histologic disease activity and fecal calprotectin levels were significantly reduced in the study participants[48]. Furthermore, colon biopsies of UC patients who responded to the 6 wk bilberry treatment revealed reduced amounts of the pro-inflammatory cytokines IFN-γ and TNF-α along with enhanced levels of the immunoregulatory cytokine IL-10[49]. Beside anthocyanins, other flavonoids exhibit nutritional values and a good safety profile of flavonoids from myrrh and chamomile has been found in a non-inferiority trial with IBD patients[50]. Boswellia serrata is a traditional herbal remedy with the recognized properties of intestinal epithelial barrier preservation and oxidative and inflammatory damage attenuation, and therefore in 2011 a large trial was carried out with this extract with the aim to maintain remission in CD patients[51]. Despite a good safety profile, no statistically significant difference was found compared with placebo regarding the primary endpoint. In a UC setting, an old study demonstrated an improvement of clinical parameters in the 30 patients treated with Boswellia serrata gum resin preparation compared with the controls who received sulfasalazine[52]. Pistacia lentiscus, known as Chios mastic gum, is an evergreen shrub widely distributed in the Mediterranean region. Oleogum resin from Pistacia lentiscus was found to act as an immunomodulatory agent on peripheral blood mononuclear cells by inhibiting TNF-α and stimulating macrophage migration inhibitory factor (MIF) activity. Indeed, its administration in CD patients resulted both in the reduction of TNF-α secretion and in the increase of MIF, with consequent inhibition of random migration and chemotaxis of monocytes/macrophages[53]. Clinical benefits of Pistacia lentiscus in CD was sustained by another study which showed a significant reduction in the CDAI compared with pretreatment values, following 4 wk of treatment[54]. The herbal extract HMPL-004 is derived from Andrographis paniculata, a herbal mixture used to treat inflammatory diseases, which has been reported to significantly reduce the transcriptional activity of NF-κB and decrease secretions of pro-inflammatory cytokines such as TNF-α and IL-6. Its benefits in active UC were addressed by two randomized, double-blind, 8 wk trials, showing a decrease in the total Mayo score of three points as well as a 30% reduction in rectal bleeding[55,56]. However, those promising greater rates of remission and clinical response compared with placebo or mesalazine did not reach statistical significance, thus suggesting a potential role for HMPL-004 in the management of IBD but also enforcing the need for additional and adequately powered studies. Figure 2 summarizes the interactions between some phytochemical agents and the inflammatory network.
Dietary lipids are one of the most active nutritional substrates modulating the human immune response and, in particular, the gut mucosal immune system. The behavior of polyunsaturated fatty acids (PUFA) have been widely investigated during inflammatory processes and also in the IBD setting. The most interesting fatty acids are the n-6 PUFA arachidonic acid (AA), which is the precursor of inflammatory eicosanoids like prostaglandin E(2) and leukotriene B(4), and the n-3 PUFAs eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which are abundant in fish oils. The modifying action of the lipid mediator profile is exerted by n-3 PUFAs mainly acting as a competitive substrate, which decreases the production of the eicosanoids from AA, but also reducing leucocyte chemotaxis and inflammatory cytokine production[57]. A rising incidence of IBD has been reported in countries in which the diseases were previously uncommon and this fact became more prominent after the “westernisation” of lifestyle, in particular with dietary changes including a higher intake of n-6 PUFAs and a reduced consumption of n-3 PUFAs[58]. Tjonneland et al[59] observed a correlation between higher intake of linoleic acid, a n-6 PUFA, and an increased risk of UC, suggesting a possible role for dietary linoleic acid in the etiology of the disease. On the other hand, oleic acid, which is the predominant ingredient of olive oil, was found to be inversely associated with UC development[60]. In agreement with this finding, a prospective large study showed an inverse association between greater long-term intake of long-chain n-3 PUFAs and risk of UC, confirming the protective effect of n-3 PUFA intake, while no specific fatty acids appeared to be associated with the risk of CD[61]. A Japanese study showed that a dietary intervention focused on lowering n-6/n-3 PUFA ratio was effective in maintaining disease remission in patients with IBD, possibly through the increasing of n-3 PUFA intake[62]. A 12 wk fish oil supplementation in patients with IBD resulted in n-3 PUFA incorporation into gut mucosal tissue and modification of inflammatory mediator profiles, showing how readily colonic lipids, prostaglandin and thromboxane synthesis can be altered by dietary changes[63]. Eleven patients with UC were studied in an 8-mo, double-blind, placebo-controlled, trial of dietary supplementation with fish oil, achieving a mean disease activity index that had declined in 56% of patients receiving fish oil and in 4% of patients on placebo. Moreover, fish oil ingestion revealed a well-tolerated profile in all patients and no alteration in routine blood exams appeared[64]. Despite these promising results, a large, randomized, multicenter trial did not show the utility of omega-3 free fatty acids for the prevention of relapse in CD[65]. However , the above mentioned successful data need to be interpret with caution due to the small study size and poor study quality. Indeed, a recent review observed how the current data do not allow for a definitive conclusion regarding the efficacy of fish oil in IBD, there being not sufficient data to recommend the use of omega 3 fatty acids for treating those conditions[66].
An interesting role in the nutraceutical scenario used in the IBD setting has been proposed for the fat-soluble vitamins, such as A, D, E, and K. The deficiency of vitamin D, whose main source is endogenous production in the skin upon exposure to sunlight, was found to be significantly associated with IBD[67]. Evidence supports an immunological role of vitamin D in IBD, both promoting tissue barrier formation through the expression of cell adhesion proteins and stabilization of tight junctions between epithelial cells, and inhibiting the production of pro-inflammatory cytokines through the activation of vitamin D receptor[68]. Interventional human studies examining the effects of vitamin D supplementation on disease activity in CD showed lower relapse rates and improvement in CDAI[69,70]. Results from a recent randomized controlled trial support the benefits from vitamin D supplementation also in UC patients, since a decrease in ESR and CRP levels was found in the treatment group[71]. However, an optimal vitamin D supplementation protocol for patients with IBD remains undetermined, and large well-designed clinical trials and mechanistic studies are needed to determine if, and how, the promising data of literature can be translated into tangible clinical benefits[72]. Still less is available regarding the other fat-soluble vitamins. It has been suggested that vitamin K may be involved in the modulation of disease activity and maintenance of bone health in IBD patients. Nakajima et al[73] evaluated vitamin K levels of patients with IBD by measuring serum undecarboxylated osteocalcin and found a significant correlation with the clinical activity index of CD. The complexity of these interactions has been highlighted by Kuwabara et al[74], who found that a low plasma concentration of vitamin K was an independent risk factor for low bone mineral density in IBD patients, but these low levels were associated with the patients’ fat intake, and not with the intake of vitamin K, thus suggesting a malabsorption rather than a poor dietary intake.
Dietary peptides and amino acids (AAs) have been shown to modulate intestinal immune functions and influence inflammatory responses, being involved in reducing inflammation, oxidative stress, and apoptosis in the gut[75]. Processes that lead to bioactive peptide release include in vivo enzymatic digestion in the gastrointestinal tract both by human and microbiota enzymes, or in vitro food processing. Any protein source can produce bioactive peptides, milk being the best studied, but bioactive peptides from egg, fish, meat, algae or soy have also been reported[76]. Milk-derived products are already in clinical use for the treatment of IBD, such as casein-based enteral feeds which are used for the treatment of CD and whose efficacy might be due, in part, to the presence of the anti-inflammatory cytokine transforming growth factor-β[77]. Colostrum is a form of milk produced by the mammary glands of mammals just prior to calving. Bovine colostrum is a rich source of nutrients, antibodies, antimicrobial peptides (e.g., lactoferrin, lactoperoxidase) and growth factors and its beneficial properties have been demonstrated during an initial study with UC patients treated by enema administration[78]. An amelioration in body composition, with a decrease in fat percentage, has been obtained in CD patients after whey and soy protein dietary supplementation[79]. Considering that a reduction of body fat contributes to the control of inflammation, these nutritional strategies may be useful as alternative or ancillary treatments in IBD. The current available information indicates a potential for food-derived peptides to counteract inflammation during the course of IBD, but further investigation is needed to clarify which peptides are responsible for the benefits and how they exert their impact . While experimental studies in animal models evaluating isolated AAs such as tryptophan, glutamine, and cysteine, offer promising data, their effects in IBD have been poorly documented in humans. The few available clinical studies show disappointing results with oral glutamine in CD and a controversial role for arginine[80].
New challenges lie ahead for clinical management of IBD, since an increasing emphasis on the safety of therapies for IBD is emerging from literature, hand in hand with the introduction of novel drugs. The available data concerning the administration of nutraceutical compounds in IBD patients support their beneficial effects accompanied by a good safety profile and invite clinicians to pay more attention to these opportunities. Indeed, the cost of treatment of IBD patients is continuously rising and nutraceutical approaches might represent a new effective and cheap treatment method. However, evidence-based information about their use is still lacking and more clinical studies to elucidate their role and optimal administration are needed.
The authors would like to thank Dr. Ashour Michael for revision of the English language.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Hoensch HHP, Lakatos PL, Yuksel I S- Editor: Ma YJ L- Editor: A E- Editor: Wang CH
| 1. | de Souza HS, Fiocchi C. Immunopathogenesis of IBD: current state of the art. Nat Rev Gastroenterol Hepatol. 2016;13:13-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1185] [Cited by in RCA: 1120] [Article Influence: 124.4] [Reference Citation Analysis (1)] |
| 2. | Abegunde AT, Muhammad BH, Bhatti O, Ali T. Environmental risk factors for inflammatory bowel diseases: Evidence based literature review. World J Gastroenterol. 2016;22:6296-6317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 125] [Cited by in RCA: 151] [Article Influence: 16.8] [Reference Citation Analysis (3)] |
| 3. | Kucharzik T, Maaser C, Lügering A, Kagnoff M, Mayer L, Targan S, Domschke W. Recent understanding of IBD pathogenesis: implications for future therapies. Inflamm Bowel Dis. 2006;12:1068-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 169] [Cited by in RCA: 177] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 4. | Toruner M, Loftus EV, Harmsen WS, Zinsmeister AR, Orenstein R, Sandborn WJ, Colombel JF, Egan LJ. Risk factors for opportunistic infections in patients with inflammatory bowel disease. Gastroenterology. 2008;134:929-936. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 719] [Cited by in RCA: 748] [Article Influence: 44.0] [Reference Citation Analysis (1)] |
| 5. | Baumgart DC, Sandborn WJ. Inflammatory bowel disease: clinical aspects and established and evolving therapies. Lancet. 2007;369:1641-1657. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1247] [Cited by in RCA: 1357] [Article Influence: 75.4] [Reference Citation Analysis (0)] |
| 6. | Park KT, Bass D. Inflammatory bowel disease-attributable costs and cost-effective strategies in the United States: a review. Inflamm Bowel Dis. 2011;17:1603-1609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 108] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 7. | Ferrari L, Krane MK, Fichera A. Inflammatory bowel disease surgery in the biologic era. World J Gastrointest Surg. 2016;8:363-370. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 33] [Cited by in RCA: 41] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Kane SV, Robinson A. Review article: understanding adherence to medication in ulcerative colitis - innovative thinking and evolving concepts. Aliment Pharmacol Ther. 2010;32:1051-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Uranga JA, López-Miranda V, Lombó F, Abalo R. Food, nutrients and nutraceuticals affecting the course of inflammatory bowel disease. Pharmacol Rep. 2016;68:816-826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 94] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 10. | Kalra EK. Nutraceutical--definition and introduction. AAPS PharmSci. 2003;5:E25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 459] [Cited by in RCA: 293] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 11. | Chauhan B, Kumar G, Kalam N, Ansari SH. Current concepts and prospects of herbal nutraceutical: A review. J Adv Pharm Technol Res. 2013;4:4-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 97] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 12. | Hilsden RJ, Verhoef MJ, Rasmussen H, Porcino A, DeBruyn JC. Use of complementary and alternative medicine by patients with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:655-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 88] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 13. | Parian A, Limketkai BN. Dietary Supplement Therapies for Inflammatory Bowel Disease: Crohn’s Disease and Ulcerative Colitis. Curr Pharm Des. 2016;22:180-188. [PubMed] |
| 14. | Farzaei MH, Bahramsoltani R, Abdolghaffari AH, Sodagari HR, Esfahani SA, Rezaei N. A mechanistic review on plant-derived natural compounds as dietary supplements for prevention of inflammatory bowel disease. Expert Rev Gastroenterol Hepatol. 2016;10:745-758. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Rossi RE, Whyand T, Murray CD, Hamilton MI, Conte D, Caplin ME. The role of dietary supplements in inflammatory bowel disease: a systematic review. Eur J Gastroenterol Hepatol. 2016;28:1357-1364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 16. | Hill C, Guarner F, Reid G, Gibson GR, Merenstein DJ, Pot B, Morelli L, Canani RB, Flint HJ, Salminen S. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11:506-514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4055] [Cited by in RCA: 5557] [Article Influence: 505.2] [Reference Citation Analysis (2)] |
| 17. | Jonkers D, Stockbrügger R. Probiotics and inflammatory bowel disease. J R Soc Med. 2003;96:167-171. [PubMed] |
| 18. | Sellon RK, Tonkonogy S, Schultz M, Dieleman LA, Grenther W, Balish E, Rennick DM, Sartor RB. Resident enteric bacteria are necessary for development of spontaneous colitis and immune system activation in interleukin-10-deficient mice. Infect Immun. 1998;66:5224-5231. [PubMed] |
| 19. | Babickova J, Gardlik R. Pathological and therapeutic interactions between bacteriophages, microbes and the host in inflammatory bowel disease. World J Gastroenterol. 2015;21:11321-11330. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 25] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Malchow HA. Crohn’s disease and Escherichia coli. A new approach in therapy to maintain remission of colonic Crohn’s disease? J Clin Gastroenterol. 1997;25:653-658. [PubMed] |
| 21. | Guslandi M, Mezzi G, Sorghi M, Testoni PA. Saccharomyces boulardii in maintenance treatment of Crohn’s disease. Dig Dis Sci. 2000;45:1462-1464. [PubMed] |
| 22. | Bourreille A, Cadiot G, Le Dreau G, Laharie D, Beaugerie L, Dupas JL, Marteau P, Rampal P, Moyse D, Saleh A. Saccharomyces boulardii does not prevent relapse of Crohn’s disease. Clin Gastroenterol Hepatol. 2013;11:982-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 121] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 23. | Garcia Vilela E, De Lourdes De Abreu Ferrari M, Oswaldo Da Gama Torres H, Guerra Pinto A, Carolina Carneiro Aguirre A, Paiva Martins F, Marcos Andrade Goulart E, Sales Da Cunha A. Influence of Saccharomyces boulardii on the intestinal permeability of patients with Crohn’s disease in remission. Scand J Gastroenterol. 2008;43:842-848. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 123] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 24. | Chapman TM, Plosker GL, Figgitt DP. VSL#3 probiotic mixture: a review of its use in chronic inflammatory bowel diseases. Drugs. 2006;66:1371-1387. [PubMed] |
| 25. | Sood A, Midha V, Makharia GK, Ahuja V, Singal D, Goswami P, Tandon RK. The probiotic preparation, VSL#3 induces remission in patients with mild-to-moderately active ulcerative colitis. Clin Gastroenterol Hepatol. 2009;7:1202-129, 1209.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 387] [Cited by in RCA: 355] [Article Influence: 22.2] [Reference Citation Analysis (0)] |
| 26. | Tursi A, Brandimarte G, Papa A, Giglio A, Elisei W, Giorgetti GM, Forti G, Morini S, Hassan C, Pistoia MA. Treatment of relapsing mild-to-moderate ulcerative colitis with the probiotic VSL#3 as adjunctive to a standard pharmaceutical treatment: a double-blind, randomized, placebo-controlled study. Am J Gastroenterol. 2010;105:2218-2227. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 391] [Cited by in RCA: 353] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 27. | Ishikawa H, Akedo I, Umesaki Y, Tanaka R, Imaoka A, Otani T. Randomized controlled trial of the effect of bifidobacteria-fermented milk on ulcerative colitis. J Am Coll Nutr. 2003;22:56-63. [PubMed] |
| 28. | Kruis W, Fric P, Pokrotnieks J, Lukás M, Fixa B, Kascák M, Kamm MA, Weismueller J, Beglinger C, Stolte M. Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Gut. 2004;53:1617-1623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 851] [Cited by in RCA: 821] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 29. | Rembacken BJ, Snelling AM, Hawkey PM, Chalmers DM, Axon AT. Non-pathogenic Escherichia coli versus mesalazine for the treatment of ulcerative colitis: a randomised trial. Lancet. 1999;354:635-639. [PubMed] |
| 30. | Faubion WA, Sandborn WJ. Probiotic therapy with E. coli for ulcerative colitis: take the good with the bad. Gastroenterology. 2000;118:630-631. [PubMed] |
| 31. | García-Lafuente A, Antolín M, Guarner F, Crespo E, Malagelada JR. Modulation of colonic barrier function by the composition of the commensal flora in the rat. Gut. 2001;48:503-507. [PubMed] |
| 32. | Gong D, Gong X, Wang L, Yu X, Dong Q. Involvement of Reduced Microbial Diversity in Inflammatory Bowel Disease. Gastroenterol Res Pract. 2016;2016:6951091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 93] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 33. | Hafer A, Krämer S, Duncker S, Krüger M, Manns MP, Bischoff SC. Effect of oral lactulose on clinical and immunohistochemical parameters in patients with inflammatory bowel disease: a pilot study. BMC Gastroenterol. 2007;7:36. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 65] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 34. | Benjamin JL, Hedin CR, Koutsoumpas A, Ng SC, McCarthy NE, Hart AL, Kamm MA, Sanderson JD, Knight SC, Forbes A. Randomised, double-blind, placebo-controlled trial of fructo-oligosaccharides in active Crohn’s disease. Gut. 2011;60:923-929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 244] [Cited by in RCA: 260] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 35. | Steed H, Macfarlane GT, Blackett KL, Bahrami B, Reynolds N, Walsh SV, Cummings JH, Macfarlane S. Clinical trial: the microbiological and immunological effects of synbiotic consumption - a randomized double-blind placebo-controlled study in active Crohn’s disease. Aliment Pharmacol Ther. 2010;32:872-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 158] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 36. | Ishikawa H, Matsumoto S, Ohashi Y, Imaoka A, Setoyama H, Umesaki Y, Tanaka R, Otani T. Beneficial effects of probiotic bifidobacterium and galacto-oligosaccharide in patients with ulcerative colitis: a randomized controlled study. Digestion. 2011;84:128-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 140] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 37. | Saxena A, Kaur K, Hegde S, Kalekhan FM, Baliga MS, Fayad R. Dietary agents and phytochemicals in the prevention and treatment of experimental ulcerative colitis. J Tradit Complement Med. 2014;4:203-217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 38. | Mosele JI, Macià A, Motilva MJ. Metabolic and Microbial Modulation of the Large Intestine Ecosystem by Non-Absorbed Diet Phenolic Compounds: A Review. Molecules. 2015;20:17429-17468. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 134] [Cited by in RCA: 167] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 39. | Vecchi Brumatti L, Marcuzzi A, Tricarico PM, Zanin V, Girardelli M, Bianco AM. Curcumin and inflammatory bowel disease: potential and limits of innovative treatments. Molecules. 2014;19:21127-21153. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 92] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 40. | Holt PR, Katz S, Kirshoff R. Curcumin therapy in inflammatory bowel disease: a pilot study. Dig Dis Sci. 2005;50:2191-2193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 261] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 41. | Lang A, Salomon N, Wu JC, Kopylov U, Lahat A, Har-Noy O, Ching JY, Cheong PK, Avidan B, Gamus D. Curcumin in Combination With Mesalamine Induces Remission in Patients With Mild-to-Moderate Ulcerative Colitis in a Randomized Controlled Trial. Clin Gastroenterol Hepatol. 2015;13:1444-9.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 241] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 42. | Hanai H, Iida T, Takeuchi K, Watanabe F, Maruyama Y, Andoh A, Tsujikawa T, Fujiyama Y, Mitsuyama K, Sata M. Curcumin maintenance therapy for ulcerative colitis: randomized, multicenter, double-blind, placebo-controlled trial. Clin Gastroenterol Hepatol. 2006;4:1502-1506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 406] [Cited by in RCA: 429] [Article Influence: 22.6] [Reference Citation Analysis (3)] |
| 43. | Singla V, Pratap Mouli V, Garg SK, Rai T, Choudhury BN, Verma P, Deb R, Tiwari V, Rohatgi S, Dhingra R. Induction with NCB-02 (curcumin) enema for mild-to-moderate distal ulcerative colitis - a randomized, placebo-controlled, pilot study. J Crohns Colitis. 2014;8:208-214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 136] [Article Influence: 12.4] [Reference Citation Analysis (2)] |
| 44. | Suskind DL, Wahbeh G, Burpee T, Cohen M, Christie D, Weber W. Tolerability of curcumin in pediatric inflammatory bowel disease: a forced-dose titration study. J Pediatr Gastroenterol Nutr. 2013;56:277-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 45. | Hilsden RJ, Verhoef MJ, Best A, Pocobelli G. Complementary and alternative medicine use by Canadian patients with inflammatory bowel disease: results from a national survey. Am J Gastroenterol. 2003;98:1563-1568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 83] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 46. | Langmead L, Feakins RM, Goldthorpe S, Holt H, Tsironi E, De Silva A, Jewell DP, Rampton DS. Randomized, double-blind, placebo-controlled trial of oral aloe vera gel for active ulcerative colitis. Aliment Pharmacol Ther. 2004;19:739-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 153] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 47. | Hoensch HP, Oertel R. The value of flavonoids for the human nutrition: Short review and perspectives. Clin Nutr Exp. 2015;3:8-14. [RCA] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (2)] |
| 48. | Biedermann L, Mwinyi J, Scharl M, Frei P, Zeitz J, Kullak-Ublick GA, Vavricka SR, Fried M, Weber A, Humpf HU. Bilberry ingestion improves disease activity in mild to moderate ulcerative colitis - an open pilot study. J Crohns Colitis. 2013;7:271-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 92] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 49. | Roth S, Spalinger MR, Gottier C, Biedermann L, Zeitz J, Lang S, Weber A, Rogler G, Scharl M. Bilberry-Derived Anthocyanins Modulate Cytokine Expression in the Intestine of Patients with Ulcerative Colitis. PLoS One. 2016;11:e0154817. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 62] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 50. | Langhorst J, Varnhagen I, Schneider SB, Albrecht U, Rueffer A, Stange R, Michalsen A, Dobos GJ. Randomised clinical trial: a herbal preparation of myrrh, chamomile and coffee charcoal compared with mesalazine in maintaining remission in ulcerative colitis--a double-blind, double-dummy study. Aliment Pharmacol Ther. 2013;38:490-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 51. | Holtmeier W, Zeuzem S, Preiss J, Kruis W, Böhm S, Maaser C, Raedler A, Schmidt C, Schnitker J, Schwarz J. Randomized, placebo-controlled, double-blind trial of Boswellia serrata in maintaining remission of Crohn’s disease: good safety profile but lack of efficacy. Inflamm Bowel Dis. 2011;17:573-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 52. | Gupta I, Parihar A, Malhotra P, Singh GB, Lüdtke R, Safayhi H, Ammon HP. Effects of Boswellia serrata gum resin in patients with ulcerative colitis. Eur J Med Res. 1997;2:37-43. [PubMed] |
| 53. | Kaliora AC, Stathopoulou MG, Triantafillidis JK, Dedoussis GV, Andrikopoulos NK. Alterations in the function of circulating mononuclear cells derived from patients with Crohn’s disease treated with mastic. World J Gastroenterol. 2007;13:6031-6036. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 54. | Kaliora AC, Stathopoulou MG, Triantafillidis JK, Dedoussis GV, Andrikopoulos NK. Chios mastic treatment of patients with active Crohn’s disease. World J Gastroenterol. 2007;13:748-753. [PubMed] |
| 55. | Tang T, Targan SR, Li ZS, Xu C, Byers VS, Sandborn WJ. Randomised clinical trial: herbal extract HMPL-004 in active ulcerative colitis - a double-blind comparison with sustained release mesalazine. Aliment Pharmacol Ther. 2011;33:194-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 56. | Sandborn WJ, Targan SR, Byers VS, Rutty DA, Mu H, Zhang X, Tang T. Andrographis paniculata extract (HMPL-004) for active ulcerative colitis. Am J Gastroenterol. 2013;108:90-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 106] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 57. | Calder PC. Polyunsaturated fatty acids, inflammatory processes and inflammatory bowel diseases. Mol Nutr Food Res. 2008;52:885-897. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 314] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 58. | Marion-Letellier R, Savoye G, Beck PL, Panaccione R, Ghosh S. Polyunsaturated fatty acids in inflammatory bowel diseases: a reappraisal of effects and therapeutic approaches. Inflamm Bowel Dis. 2013;19:650-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 83] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 59. | IBD in EPIC Study Investigators, Tjonneland A, Overvad K, Bergmann MM, Nagel G, Linseisen J, Hallmans G, Palmqvist R, Sjodin H, Hagglund G, Berglund G, Lindgren S, Grip O, Palli D, Day NE, Khaw KT, Bingham S, Riboli E, Kennedy H, Hart A. Linoleic acid, a dietary n-6 polyunsaturated fatty acid, and the aetiology of ulcerative colitis: a nested case-control study within a European prospective cohort study. Gut. 2009;58:1606-1611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 269] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 60. | de Silva PS, Luben R, Shrestha SS, Khaw KT, Hart AR. Dietary arachidonic and oleic acid intake in ulcerative colitis etiology: a prospective cohort study using 7-day food diaries. Eur J Gastroenterol Hepatol. 2014;26:11-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 61. | Uchiyama K, Nakamura M, Odahara S, Koido S, Katahira K, Shiraishi H, Ohkusa T, Fujise K, Tajiri H. N-3 polyunsaturated fatty acid diet therapy for patients with inflammatory bowel disease. Inflamm Bowel Dis. 2010;16:1696-1707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 62. | Ananthakrishnan AN, Khalili H, Konijeti GG, Higuchi LM, de Silva P, Fuchs CS, Willett WC, Richter JM, Chan AT. Long-term intake of dietary fat and risk of ulcerative colitis and Crohn’s disease. Gut. 2014;63:776-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 296] [Cited by in RCA: 362] [Article Influence: 32.9] [Reference Citation Analysis (0)] |
| 63. | Hillier K, Jewell R, Dorrell L, Smith CL. Incorporation of fatty acids from fish oil and olive oil into colonic mucosal lipids and effects upon eicosanoid synthesis in inflammatory bowel disease. Gut. 1991;32:1151-1155. [PubMed] |
| 64. | Aslan A, Triadafilopoulos G. Fish oil fatty acid supplementation in active ulcerative colitis: a double-blind, placebo-controlled, crossover study. Am J Gastroenterol. 1992;87:432-437. [PubMed] |
| 65. | Feagan BG, Sandborn WJ, Mittmann U, Bar-Meir S, D’Haens G, Bradette M, Cohen A, Dallaire C, Ponich TP, McDonald JW. Omega-3 free fatty acids for the maintenance of remission in Crohn disease: the EPIC Randomized Controlled Trials. JAMA. 2008;299:1690-1697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 180] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 66. | Turner D, Shah PS, Steinhart AH, Zlotkin S, Griffiths AM. Maintenance of remission in inflammatory bowel disease using omega-3 fatty acids (fish oil): a systematic review and meta-analyses. Inflamm Bowel Dis. 2011;17:336-345. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 132] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 67. | Del Pinto R, Pietropaoli D, Chandar AK, Ferri C, Cominelli F. Association Between Inflammatory Bowel Disease and Vitamin D Deficiency: A Systematic Review and Meta-analysis. Inflamm Bowel Dis. 2015;21:2708-2717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 188] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 68. | Mouli VP, Ananthakrishnan AN. Review article: vitamin D and inflammatory bowel diseases. Aliment Pharmacol Ther. 2014;39:125-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 175] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 69. | Miheller P, Muzes G, Hritz I, Lakatos G, Pregun I, Lakatos PL, Herszényi L, Tulassay Z. Comparison of the effects of 1,25 dihydroxyvitamin D and 25 hydroxyvitamin D on bone pathology and disease activity in Crohn’s disease patients. Inflamm Bowel Dis. 2009;15:1656-1662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 101] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 70. | Jørgensen SP, Agnholt J, Glerup H, Lyhne S, Villadsen GE, Hvas CL, Bartels LE, Kelsen J, Christensen LA, Dahlerup JF. Clinical trial: vitamin D3 treatment in Crohn’s disease - a randomized double-blind placebo-controlled study. Aliment Pharmacol Ther. 2010;32:377-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 286] [Cited by in RCA: 295] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 71. | Sharifi A, Hosseinzadeh-Attar MJ, Vahedi H, Nedjat S. A randomized controlled trial on the effect of vitamin D3 on inflammation and cathelicidin gene expression in ulcerative colitis patients. Saudi J Gastroenterol. 2016;22:316-323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 52] [Cited by in RCA: 60] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 72. | Hlavaty T, Krajcovicova A, Payer J. Vitamin D therapy in inflammatory bowel diseases: who, in what form, and how much? J Crohns Colitis. 2015;9:198-209. [PubMed] |
| 73. | Nakajima S, Iijima H, Egawa S, Shinzaki S, Kondo J, Inoue T, Hayashi Y, Ying J, Mukai A, Akasaka T. Association of vitamin K deficiency with bone metabolism and clinical disease activity in inflammatory bowel disease. Nutrition. 2011;27:1023-1028. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 39] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 74. | Kuwabara A, Tanaka K, Tsugawa N, Nakase H, Tsuji H, Shide K, Kamao M, Chiba T, Inagaki N, Okano T. High prevalence of vitamin K and D deficiency and decreased BMD in inflammatory bowel disease. Osteoporos Int. 2009;20:935-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 82] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 75. | Zhang H, Hu CA, Kovacs-Nolan J, Mine Y. Bioactive dietary peptides and amino acids in inflammatory bowel disease. Amino Acids. 2015;47:2127-2141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 54] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 76. | Martínez-Augustin O, Rivero-Gutiérrez B, Mascaraque C, Sánchez de Medina F. Food derived bioactive peptides and intestinal barrier function. Int J Mol Sci. 2014;15:22857-22873. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 68] [Cited by in RCA: 80] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 77. | Richman E, Rhodes JM. Review article: evidence-based dietary advice for patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2013;38:1156-1171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 78] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 78. | Khan Z, Macdonald C, Wicks AC, Holt MP, Floyd D, Ghosh S, Wright NA, Playford RJ. Use of the ‘nutriceutical’, bovine colostrum, for the treatment of distal colitis: results from an initial study. Aliment Pharmacol Ther. 2002;16:1917-1922. [PubMed] |
| 79. | Machado JF, Oya V, Coy CS, Morcillo AM, Severino SD, Wu C, Sgarbieri VC, Vilela MM. Whey and soy protein supplements changes body composition in patients with Crohn’s disease undergoing azathioprine and anti-TNF-alpha therapy. Nutr Hosp. 2015;31:1603-1610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 80. | Coëffier M, Marion-Letellier R, Déchelotte P. Potential for amino acids supplementation during inflammatory bowel diseases. Inflamm Bowel Dis. 2010;16:518-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 65] [Article Influence: 4.3] [Reference Citation Analysis (0)] |