Published online Nov 7, 2016. doi: 10.3748/wjg.v22.i41.9242
Peer-review started: May 9, 2016
First decision: June 20, 2016
Revised: July 9, 2016
Accepted: August 1, 2016
Article in press: August 1, 2016
Published online: November 7, 2016
Processing time: 181 Days and 20.8 Hours
Spontaneous rupture of hepatocellular carcinoma (HCC) is a life-threatening complication and its prognosis is significantly poor because of the high recurrence rate after initial hepatectomy. Resection of isolated extrahepatic metastasis of HCC has been advocated to obtain a possibility of long-term survival. However, it is a challenge for clinicians to detect implantation metastasis of spontaneously ruptured HCC. Accurate re-staging plays the most important role in making a decision on isolated metastasis resection. 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) is useful in detecting intra-abdominal implantation metastasis from a variety of malignancies and shows superior accuracy to conventional imaging modalities in determining the location of metastasis. We present one patient with a new isolated pelvic implantation metastasis detected by 18F-FDG PET/CT and pathologically confirmed by PET/CT-guided percutaneous biopsy, who had a history of resection of spontaneously ruptured HCC two years ago. The patient’s condition was stable at the 6-mo follow-up after resection of the isolated pelvic metastasis.
Core tip: Spontaneous rupture of hepatocellular carcinoma is a life-threatening complication and its prognosis is significantly poor. It is a challenge for clinicians to detect implantation metastasis. Accurate re-staging plays the most important role in making a decision on isolated metastasis resection.18F-fluorodeoxyglucose positron emission tomography/computed tomography is useful in detecting intra-abdominal implantation metastasis from a variety of malignancies and shows superior accuracy to conventional imaging modalities in determining the location of metastasis.
- Citation: Hao B, Guo W, Luo NN, Fu H, Chen HJ, Zhao L, Wu H, Sun L. Metabolic imaging for guidance of curative treatment of isolated pelvic implantation metastasis after resection of spontaneously ruptured hepatocellular carcinoma: A case report. World J Gastroenterol 2016; 22(41): 9242-9246
- URL: https://www.wjgnet.com/1007-9327/full/v22/i41/9242.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i41.9242
Spontaneous rupture is a fatal complication seen in 3%-15% of all patients with hepatocellular carcinoma (HCC) and has a high mortality rate[1-3]. Currently, there is no consensus about the best treatment for spontaneously ruptured HCC. Low-risk curative hepatic resection may be the best treatment option for Child-Pugh A-B patients with spontaneously ruptured HCC. Small tumor length and number, and early Barcelona Clinic Liver Cancer (BCLC) stage are the most crucial predictors associated with satisfactory overall survival. However, resection of isolated extrahepatic metastasis of HCC has been advocated to obtain a possibility of long-term survival. Intra-abdominal implantation metastasis can be seen anywhere in the abdominal/pelvic cavity. Therefore, it is logical that whole body 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) should be a tool for monitoring recurrence of HCC rupture. We present here a patient with spontaneously ruptured HCC resected two years ago and a new pelvic metastasis recently identified by 18F-FDG PET/CT. Pelvic implantation metastasis of spontaneously ruptured HCC was confirmed by PET/CT guided percutaneous biopsy. A relatively good prognosis was achieved in this patient after surgical resection of the isolated pelvic implantation metastasis.
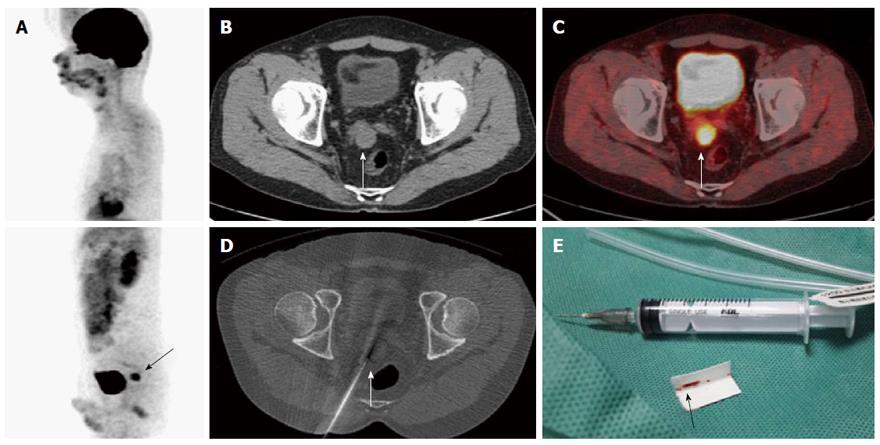
Two years ago, a 38-year-old man with a family history of HCC was referred to our hospital after an episode of sudden upper abdominal pain. Laboratory examination revealed that he was a hepatitis B virus (HBV) carrier and his alpha-fetoprotein (AFP) level was more than 1000 ng/mL. Contrast-enhanced CT showed multiple nodules in the right lobe of the liver (Figure 1) and segments V-VI-VII hepatectomy was performed in October 2013. Histology showed an HCC (Edmondson-Steiner grade III) with a diameter of 12.0 cm and early cirrhosis. No microscopic vascular invasion was found. After partial liver resection, his AFP level returned to normal. During 25 mo of follow-up, contrast-enhanced magnetic resonance imaging (MRI) every 3 mo did not reveal any evidence of intrahepatic recurrence or extrahepatic metastasis; however, his AFP level gradually increased to 418.18 ng/mL. To find out the reason for the AFP increase, the patient was referred to our center for a whole body 18F-FDGPET/CT examination. 18F-FDG PET/CT detected an isolated hypermetabolic lesion with a diameter of 2.4 cm between the right side of the seminal vesicle and the rectum, which suggested a pelvic implantation metastasis. A PET/CT-guided percutaneous biopsy of the hypermetabolic lesion (Figure 2) was performed and confirmed a real pelvic implantation metastasis of the spontaneously ruptured HCC. After the isolated hypermetabolic metastasis was resected, his AFP level decreased to the accepted level. There was no recurrence or metastasis in the 6-mo follow-up period after resection of the isolated pelvic implantation metastasis.
Spontaneous rupture is one of the most serious complications of HCC, and its mortality rates range from 25% to 75%[4]. Early-stage elective hepatectomy is the first-choice treatment for patients with spontaneously ruptured HCC, with 1-, 3- and 5-year overall survival rates being 85.4%, 63.2% and 46.3%, respectively, compared with 66.3%, 23.4% and 10.1% in non-surgical patients[5]. The prognosis of spontaneously ruptured HCC has been reported to be poor, and most (30%-70%) of the patients died within 30 d after resection of the spontaneous ruptured HCC[6]. The patients with younger age, better liver function and earlier tumor stage after resection have a good prognosis[7]. In our case, the 38-year-old patient with good liver function underwent a curative hepatectomy and achieved a chance of long-term survival.
Intra-abdominal implantation metastasis is a significantly unfavorable factor for long-term survival in patients with spontaneously ruptured HCC. HCC rupture with intra-abdominal hemorrhage is accompanied with neoplastic cell implantation metastasis. Intra-abdominal implantation metastases are divided into two types: isolated and diffuse. The isolated implantation metastasis of spontaneously ruptured HCC is suitable for curative surgical treatment while diffuse metastasis does not. Most reported cases of peritoneal metastases were documented months after HCC rupture[8]. Hung et al[9] and Yunoki et al[10] reported peritoneal metastasis in the omentum occurring one year after HCC rupture. Shirabe et al[11] reported a patient who had previously undergone hepatic resection for ruptured HCC but developed a solitary peritoneal recurrence at the incision site 105 mo later. Lin et al[12] reported a patient who had diffuse intraperitoneal metastasis after spontaneous rupture of HCC. In contrast, pelvic implantation metastasis is rarely reported. Nakashima et al[13] noted that metastases to the pouch of Douglas occurred in 6.2% of 232 consecutive autopsy cases of HCC. We present here one patient with isolated implantation metastasis occurring two years after resection of the initial spontaneously ruptured HCC.
The early diagnosis of recurrence and metastasis of spontaneously ruptured HCC is very important for further treatment to improve the prognosis. At present, the main methods used for detecting recurrence and metastasis in clinical practice include monitoring serum AFP value and conventional imaging. An unexplained gradual rise of AFP after treatment is a sensitive early indicator of tumor recurrence or extrahepatic metastasis; however, AFP cannot localize the lesion. Although conventional imaging has been generally acknowledged in detecting intrahepatic recurrence, it has many limitations in detecting extrahepatic recurrence and metastasis. Nowdays, 18F-FDG PET/CT can not only detect the host residual liver recurrence, but also is the most effective imaging method for detecting distant metastasis of tumor[14].
18F-FDG PET/CT is a useful metabolic imaging tool for monitoring recurrence and re-staging when AFP is increasing again after the resection of spontaneously ruptured HCC, especially for the isolated extrahepatic implantation metastasis[15]. It is not only an effective whole-body imaging technique but also detects metabolic changes that differentiate malignant from benign tumors through the precise localization of suspected 18F-FDG uptake foci and their characterization compared to conventional imaging structural findings[16]. In our previous study[17], we have found that merged PET/CT images provide a complementary role in the assessment of whether the detected disease is resectable. It is crucial for our patient that the detected isolated pelvic implantation metastasis by 18F-FDG PET/CT scan was curatively re-resected two years after the resection of spontaneously ruptured HCC.
The isolated implantation metastasis, if possible, should be curatively resected after initial resection of spontaneously ruptured HCC, which might offer long-term survival benefit[18,19]. 18F-FDG PET/CT provide important information for the detection of extrahepatic implantation metastasis and precise location to complete preoperative re-staging. This case is sensationally practical for patient follow-up and re-staging after the resection of spontaneously ruptured HCC, especially when a gradual rise of AFP that conventional imaging cannot explain is present.
A 38-year-old man was in good condition and asymptomatic two years after the resection of spontaneously ruptured hepatocellular carcinoma (HCC).
It is highly suspected as recurrence after the resection of spontaneously ruptured HCC due to an AFP increase.
Pelvic primary benign tumor, pelvic malignant tumor, and germ cell tumor.
The AFP gradually increased from the normal level to 418.18 ng/mL.
18F-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) detected an isolated hypermetabolic lesion with a diameter of 2.4 cm between the right side of the seminal vesicle and the rectum.
PET/CT-guided percutaneous biopsy of the hypermetabolic lesion was performed and confirmed pelvic implantation metastasis of the spontaneously ruptured HCC.
The isolated hypermetabolic metastasis in the pelvic cavity was excised for curative surgical treatment.
Pelvic implantation metastasis has not been reported, and it only was noted that metastases to the pouch of Douglas occurred in autopsy cases of HCC.
Spontaneously ruptured hepatocellular carcinoma has a poor prognosis, and resection of isolated extrahepatic metastasis of HCC has been advocated to obtain a possibility of long-term survival.
18F-FDG PET/CT is a useful metabolic imaging tool for monitoring recurrence of spontaneous ruptured HCC and its re-staging when AFP is increasing again after the resection of spontaneously ruptured HCC, especially for the isolated extrahepatic implantation metastasis.
Imaging supports the findings. It is well-documented, written and presented.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Sazci A, Zielinski J S- Editor: Qi Y L- Editor: Wang TQ E- Editor: Wang CH
| 1. | Kim JY, Lee JS, Oh DH, Yim YH, Lee HK. Transcatheter arterial chemoembolization confers survival benefit in patients with a spontaneously ruptured hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 2012;24:640-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 2. | Jin YJ, Lee JW, Park SW, Lee JI, Lee DH, Kim YS, Cho SG, Jeon YS, Lee KY, Ahn SI. Survival outcome of patients with spontaneously ruptured hepatocellular carcinoma treated surgically or by transarterial embolization. World J Gastroenterol. 2013;19:4537-4544. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 40] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 3. | Han XJ, Su HY, Shao HB, Xu K. Prognostic factors of spontaneously ruptured hepatocellular carcinoma. World J Gastroenterol. 2015;21:7488-7494. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Bassi N, Caratozzolo E, Bonariol L, Ruffolo C, Bridda A, Padoan L, Antoniutti M, Massani M. Management of ruptured hepatocellular carcinoma: implications for therapy. World J Gastroenterol. 2010;16:1221-1225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 41] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 5. | Bouliaris K, Christodoulidis G, Symeonidis D, Diamantis A, Tepetes K. Damage Control Surgery for Hepatocellular Cancer Rupture in an Elderly Patient: Survival and Quality of Life. Case Rep Emerg Med. 2015;2015:536029. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Hsueh KC, Fan HL, Chen TW, Chan DC, Yu JC, Tsou SS, Chang TM, Hsieh CB. Management of spontaneously ruptured hepatocellular carcinoma and hemoperitoneum manifested as acute abdomen in the emergency room. World J Surg. 2012;36:2670-2676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 47] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Sun P, Song ZF, Hu QG, Xiong J, Yang X, Zheng QC. Spontaneous rupture of hepatocellular carcinoma: a retrospective study of 87 patients in a teaching hospital. Zhongde Linchuang Zhongliu Zazhi. 2013;12:P175-P180. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | Li J, Huang L, Liu CF, Cao J, Yan JJ, Xu F, Wu MC, Yan YQ. Risk factors and surgical outcomes for spontaneous rupture of BCLC stages A and B hepatocellular carcinoma: a case-control study. World J Gastroenterol. 2014;20:9121-9127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 32] [Reference Citation Analysis (0)] |
| 9. | Hung MC, Wu HS, Lee YT, Hsu CH, Chou DA, Huang MH. Intraperitoneal metastasis of hepatocellular carcinoma after spontaneous rupture: a case report. World J Gastroenterol. 2008;14:3927-3931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Yunoki Y, Takeuchi H, Makino Y, Murakami I, Yasui Y, Tanakaya K, Kawaguchi K, Konaga E. Intraperitoneal seeding of ruptured hepatocellular carcinoma: case report. Abdom Imaging. 1999;24:398-400. [PubMed] |
| 11. | Shirabe K, Kitamura M, Tsutsui S, Maeda T, Matsumata T, Sugimachi K. A long-term survivor of ruptured hepatocellular carcinoma after hepatic resection. J Gastroenterol Hepatol. 1995;10:351-354. [PubMed] |
| 12. | Lin CC, Chen CH, Tsang YM, Jan IS, Sheu JC. Diffuse intraperitoneal metastasis after spontaneous rupture of hepatocellular carcinoma. J Formos Med Assoc. 2006;105:577-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Nakashima T, Okuda K, Kojiro M, Jimi A, Yamaguchi R, Sakamoto K, Ikari T. Pathology of hepatocellular carcinoma in Japan. 232 Consecutive cases autopsied in ten years. Cancer. 1983;51:863-877. [PubMed] |
| 14. | Chen Z, Liang H, Zhang X, Wang X, Chen W, Shi X, Yi C, Rao L. [Value of (18)F-FDG PET/CT and CECT in detecting postoperative recurrence and extrahepatic metastasis of hepatocellular carcinoma in patients with elevated serum alpha-fetoprotein]. Nan Fang Yi Ke Da Xue Xue Bao. 2012;32:1615-1619. [PubMed] |
| 15. | Yang SH, Suh KS, Lee HW, Cho EH, Cho JY, Cho YB, Yi NJ, Lee KU. The role of (18)F-FDG-PET imaging for the selection of liver transplantation candidates among hepatocellular carcinoma patients. Liver Transpl. 2006;12:1655-1660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 129] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 16. | Sacks A, Peller PJ, Surasi DS, Chatburn L, Mercier G, Subramaniam RM. Value of PET/CT in the management of primary hepatobiliary tumors, part 2. AJR Am J Roentgenol. 2011;197:W260-W265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 17. | Sun L, Guan YS, Pan WM, Chen GB, Luo ZM, Wu H. Positron emission tomography/computer tomography in guidance of extrahepatic hepatocellular carcinoma metastasis management. World J Gastroenterol. 2007;13:5413-5415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 19] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Hong DF, Liu YB, Peng SY, Pang JZ, Wang ZF, Cheng J, Shen GL, Zhang YB. Management of hepatocellular carcinoma rupture in the caudate lobe. World J Gastroenterol. 2015;21:8163-8169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Aoki T, Kokudo N, Matsuyama Y, Izumi N, Ichida T, Kudo M, Ku Y, Sakamoto M, Nakashima O, Matsui O. Prognostic impact of spontaneous tumor rupture in patients with hepatocellular carcinoma: an analysis of 1160 cases from a nationwide survey. Ann Surg. 2014;259:532-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 126] [Article Influence: 11.5] [Reference Citation Analysis (0)] |