Published online Nov 7, 2016. doi: 10.3748/wjg.v22.i41.9235
Peer-review started: June 27, 2016
First decision: August 8, 2016
Revised: August 17, 2016
Accepted: September 6, 2016
Article in press: September 6, 2016
Published online: November 7, 2016
Processing time: 132 Days and 8.9 Hours
Hirschsprung’s disease (HD) is an intestinal malformation caused by the innate absence of ganglion cells in the neural plexus of the colorectal wall, and is most common in male infants. It is rare in adult, and is usually left-sided. Herein we reported based on the CARE guidelines a case of a 47-year-old adult female suffering from “right-sided” HD complicated by refractory hypertension and cough. The patient with a history of cesarean section and with digestive unfitness (abdominal pain, distention, and constipation) only since 20 years old had recurrence of HD after initial surgery due to the incomplete removal of the HD-affected bowel based on a diagnosis of “chronic ileus”, leading to the relapse of the digestive symptoms and the emergence of some intractable circulatory and respiratory complications which could be hardly controlled by conservative treatment. During the long interval before coming to our department for help, she had been re-hospitalized for several times with various misdiagnoses and supplied merely with symptomatic treatment which could only achieve temporary symptomatic relief. At her admission to our department, the imaging examinations strongly indicated recurrent HD which was further supported by pathological examinations, and right hemi-colectomy was performed to remove the remnant aganglionic intestinal segment. Intraoperative and postoperative pathology supported the completeness of the definitive resection. Post-operation, the patient’s bowel motility significantly improved, and interestingly, the complications disappeared. For adult patients with long-term constipation combined with cough and hypertension, rare diseases like HD which requires definite surgery and which could be “right-sided” should not be overlooked. It is vital to diagnose and cure HD patients in childhood. Through the comparison of the two surgeries, it is noteworthy that for diagnosed HD, sufficient removal of the non-functional intestine confirmed by intraoperative pathology is essential.
Core tip: Hirschsprung’s disease (HD) is most common in male infant, and is usually left-sided. Herein we reported a case of a 47-year-old adult female suffering from “right-sided” recurrent HD complicated by refractory hypertension and cough and receiving reoperation. The patient with digestive unfitnesses only since 20 years old had recurrence of HD after the initial surgery due to the incomplete removal of the HD-affected bowel. At her admission to our department, right hemi-colectomy was performed to completely remove the remnant aganglionic intestinal segment, which was confirmed by intraoperative pathology. Post-operation, the patient’s bowel motility significantly improved, and interestingly, the complications disappeared.
- Citation: Wei ZJ, Huang L, Xu AM. Reoperation in an adult female with "right-sided" Hirschsprung's disease complicated by refractory hypertension and cough. World J Gastroenterol 2016; 22(41): 9235-9241
- URL: https://www.wjgnet.com/1007-9327/full/v22/i41/9235.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i41.9235
Congenital megacolon (Hirschsprung’s disease, HD) is an intestinal malformation caused by the innate absence or decrease of ganglion cells in the submucosal (Meissner) and myenteric (Auerbach) neural plexuses of the colorectal wall, and dates back to a defect in the craniocaudal migration of the neuroblast originating from the neural crest that occurs during the first 3 mo of gestation[1]. It is most common in male neonates and infants, and usually affects the left colon and part of the rectum. Rarely the whole colon could be aganglionic, which is known as the Zuelzer-Wilson syndrome[2]. HD patients mostly suffer from long-term constipation, distention, and bellyache which are not relevant to diet. Adult HD, which is rare, often develops from misdiagnosed infant HD with mild symptoms, and is easily considered intractable constipation[3]. Conservative treatment does not work satisfactorily for adult HD, which usually requires surgery[4].
Herein we report a case of a female adult patient with ‘right-sided’ HD complicated by refractory hypertension and cough who had undergone several misdiagnoses and who received re-surgery in our department 17 years after the initial operation due to continuous digestive, circulatory and respiratory unfitness, which, to the best of our knowledge, has not been previously reported.
Written informed consent was obtained from the patient, and this report was approved by the Institutional Review Board of the First Affiliated Hospital of Anhui Medical University and was in accordance with the Declaration of Helsinki[5], the Good Clinical Practice[6], and the CARE Statement[7] for clinical case reports.
On April 23rd 2015, a 47-year-old female patient with a surgical history of cesarean section in 1992 was admitted to our department complaining about postprandial pain and distention of the right lower abdomen for 17 years after the resection of most part of the transverse colon. She suffered from constipation since 1988, with the average defecation frequency once 3-4 d, and the lowest once a week, and received no special treatment then. However, she did not experience any abdominal symptoms during the first 20 years of her life.
On 10th February 1998, she was hospitalized in Department of Emergency Surgery in our hospital because of bellyache and constipation, and was discharged after conservative treatment. However, she was re-hospitalized due to intestinal obstruction and was suspected as “adhesive ileus” based on her operation history only 6 d later. The transverse colon resection was planned. The pre-surgical blood and urine tests were normal. The endoscopic pathological examination and the routine fecal examination were not conducted. The surgery was conducted on 12th March. During surgery, it was observed that the middle of the transverse colon was significantly distended to approximately 10 cm in diameter. Around 25 cm of the dilated colon was removed, and the splenic flexure was rectified. The post-operational pathological examination showed infiltration of acute and chronic inflammation cells and focal hemorrhage (the immunohistochemistry and specific staining tests were not performed, possibly due to the fact that HD was not considered, or to the unavailability of such a test then). However, after the first surgery, she still experienced constipation, and postprandial bloating and bellyache, and soon felt obvious aggravation of the symptoms. She was then prescribed with laxatives. She was hospitalized to our hospital again in 2000 due to ileus, and refused the suggested reoperation. She was discharged when feeling better after conservative management, and depended on laxatives thereafter. From 2000 to 2015, the patient was admitted to hospital for several times due to intestinal obstruction, and the symptoms were relieved after symptomatic treatment like gastrointestinal decompression, enema, and anti-inflammation. Unfortunately, during this period, she had not been proposed the diagnosis of HD.
The patient had hypertension since 2002, and the blood pressure (BP) could be initially well-controlled by oral nitrendipine treatment. However, later on the BP gradually elevated, and had to be antagonized by the addition of captopril. In recent 2 years, the patient experienced aggravated anorexia and post-meal symptoms, obvious weight loss (about 20 kg), progressive continuous cough, and significantly elevated BP (146/100 mmHg at admission, and 180/110 mmHg as the highest level during drug administration), which could be poorly controlled by oral symptomatic treatment drugs. On April 21st 2015, the colon contrast pneumobarium conducted in the Fourth Affiliated Hospital of Anhui Medical University indicated giant right hemi-colon, and she came to our department seeking for medical management. The patient weighed 44 kg at admission. The physical examination showed a bulging abdomen with an about 15 cm-long old surgical scar on the right upper abdomen. The drum sound was obvious during percussion, and the frequency of the bowel sound was 5 times per min. All the other physical examinations were normal.
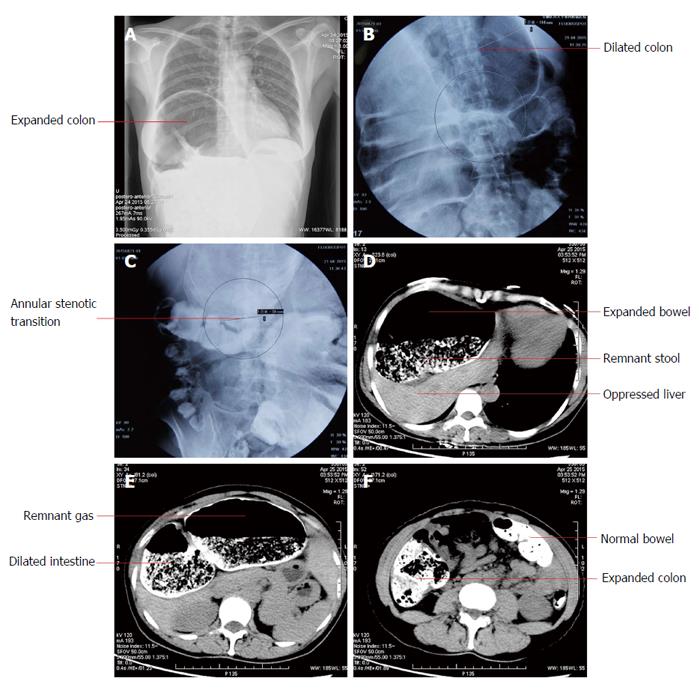
For the hospitalization in our department, the routine blood and fecal tests were normal, and the urine test showed the presence of bacteria (429/μL). Imaging examinations offered informative clues for diagnosis (Figure 1). The chest radiography showed right pleural effusion and thickening, and potential colon interposition. The abdominopelvic computed tomography (CT) and the colon double contract pneumobarium radiography revealed significant expansion of the cecum, the ascending colon, the hepatic flexure of colon, and the remnant transverse colon, with the most dilated area 13.6 cm wide. Abundant residual stool, gas, and liquid existed. An annular stenotic transitional segment (only 3.8 cm wide) could be perceived, and the original transverse-descending colon anastomosis was slightly narrow with limited distension capability. All the other intestines were normal. The neighboring organs and tissues underwent marked displacement and deformation under pressure.
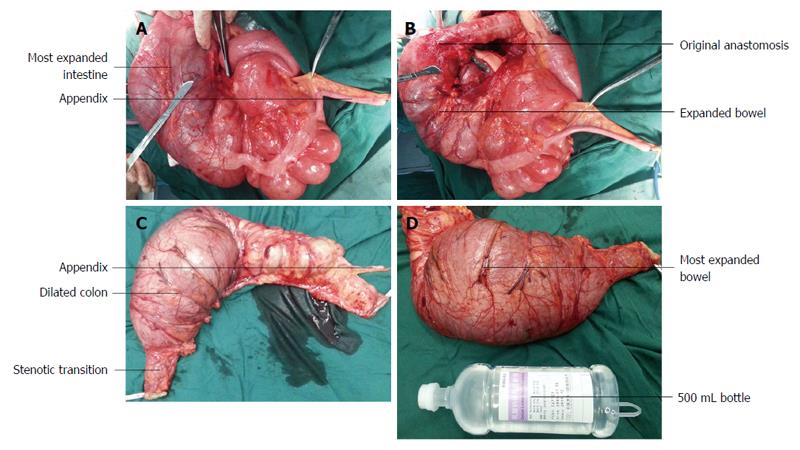
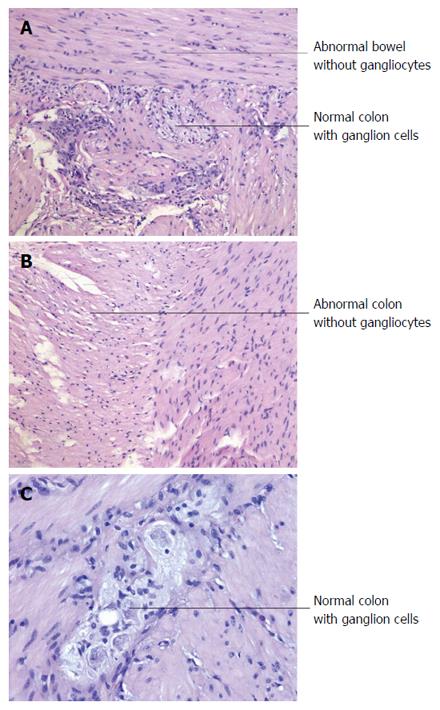
Right colectomy was conducted for the patient to remove the aganglionic and the dilated fragments based on the initial consideration of HD followed by ileum-colon anastomosis, and the resected intestine included the non-dilated bowel 6 cm beyond the anastomosis of the initial surgery. The intraoperative frozen section pathological examination convinced us of the completeness and definitiveness of the eradication of all the remnant aganglionic bowel segment. An intestine segment with normal ganglion cells could be seen in the resected specimen pathologically. During surgery, we observed mild adhesion of the abdominal cavity, the obviously outstretched colon, and the deformed liver due to extrusion (Figure 2). The right lobe of the liver markedly shifted upwards, and the left lobe underwent compensatory enlargement. The left colon and rectum were all fine in morphology and motility with satisfactory tension perceived and without abnormal dilation or constriction, and the intraoperative pathology further supported that they were normal in structure with sufficient ganglion cells and should not be removed, which seems different from the common understanding that they are usually affected in HD[1]. The postsurgical pathological report supported the HD diagnosis, showed the remnant aganglionic section left behind by the first surgery, and importantly, confirmed the definitiveness of the reoperation based on the presence of normal bowel segment with normal ganglion cells in the resected specimen (Figure 3).
Interestingly, after reoperation, the BP dropped to 138/69 mmHg at discharge without the assistance of any drug, and cough was also cured. Symptomatic treatment has thus been ceased since then. Up till now, the patient has been followed up once every month. No adverse event was observed. She reported satisfactory diet, without distention and ache of the abdomen, cough, or hypertension. The defecation frequency is 3-4 times per day without the assistance of laxative, the bowel movement is active and smooth, and she gains weight of about 6 kg with satisfactory fecal control. She feels much better concerning quality of life (QoL), especially in the digestive aspect. Contrary to the initial surgery, the patient did not feel recurrence/worsening of any HD-related symptoms. The abdominal CT scan and X-ray examination conducted in May 2016 did not reveal abnormality. Her condition was still closely and carefully watched on, and she expressed great willingness to share her case.
Adult HD was first described by Rosin et al[8] in 1950 concerning a 54-year-old man with absence of colorectal gangliocytes. Most of the HD patients take laxatives or receive enemas to facilitate defecation, with the hope to reduce the digestive unfitness, which they suffer since childhood, and which could provide key clues for diagnosis. HD could lead to serious and even lethal complications like enterocolitis, bowel volvulus and necrosis, which require urgent surgical intervention[9]. The major diagnostic method of HD is barium enema with the mark of a narrowed transition zone, which might however worsen ileus at the initial stage of the disease[10]. Nowadays, CT scan has become a commonly used diagnostic approach, and could reveal the thickening extent of the colon and the uniformity during enhancement scanning[11]. The golden diagnostic standard is endoscopic biopsy. A multimodal investigation approach is usually required for diagnosis[12].
Rectum and distal sigmoid colon are usually affected by HD which is mostly a left-sided disease[4,13], while in this case only the right hemi-colon was the influenced bowel as confirmed by pathology and intraoperative observation, which is scarce compared to the previous literature reports, and the initial suspicious diagnosis was even “colon interposition” by experts based on the imaging. Hypoganglionosis and intestinal neuronal dysplasia are the common allied disorders of HD, and the whole digestive tract might be affected to be disordered in motility, causing refractory anorexia and constipation[14,15], which however slightly affects the QoL in the long term[16]. The tolerance of HD is relatively good due to a usually short aganglionic bowel segment[17]. Unfortunately, the initial surgery in this case only removed most part of the dilated colon, and ignored the silent aganglionic part just adjacent to the structurally-abnormal bowel. Older female HD patients with a longer aganglionic segment might have a poorer bowel function and QoL[4,18,19]. The patient in this case experienced apparent unfitness after her adolescence presenting like the pseudo-HD[20], which could be explained by the gradual proceeding of the disease, or by the fact that adult HD might be acquired rather than congenital[21]. Interestingly, she did not experience obvious discomfort during her first 20 years of life. The defecation frequency of this HD adult was more frequently than reported by literature (1/7-10 d)[22].
For HD surgery, it is important to completely remove the bowel without functional ganglion cells[23]. The major surgical methods to treat distal HD include the one- or two-stage Duhamel, Swenson, Soave, Rehbein, and some modified approaches, and the choice was influenced by surgeons’ experience[4]. The laparoscopic approach could also be applied[24]. The modified Duhamel operation is considered satisfactory with a few manageable adverse events and nice functional outcomes when treating adult HD patients[16,25], and the subtotal colectomy combined with the modified Duhamel procedure is also effective and safe when dealing with adult distal HD[26]. However, few literatures have reported the surgical management of proximal/”right-sided” HD. In this case, the left colon and the rectum were normal, and it is obviously inappropriate to remove them as the reported surgical method for distal HD, since it is principle to preserve as many as healthy tissues for our patients, otherwise the postsurgical QoL would be very low with very poor fecal control. We herein reported our case with the hope to add some novel knowledge to the literature. For the second surgery of this patient, right colectomy was performed to resect the remnant aganglionic segment, which had not been carefully removed by the initial operation. It turns out to be successful based on the improvement of the patient’s syndromes and imaging findings. The biofeedback therapy could be additionally supplied post-surgery to further recover the intestinal function[27].
In this case, the patient’s colon was significantly aggrandized due to the long-term constipation. Her symptoms were not significantly relieved after the initial surgery, and later experienced refractory complications (hypertension and cough), which has been rarely reported before. The potential reasons for the recurrence are that the intraoperative frozen pathological examination, which should be highly demanded for such patients, and which could avoid insufficient extent of resection, was not conducted during the first surgery potentially due to the limited medical condition then, thus leading to the reoperation. The cough was possibly caused by the stimulation of the diaphragm elevated by the ectatic colon, and the hypertension might be attributed to the disturbed circulation due to the imbalanced pleuroperitoneal pressure and the oppressed liver. For the second surgery, the patient received right colectomy, which effectively eliminated the initial symptoms, as well as the hypertension and cough, and effectively increased the postoperative defecation frequency and QoL without causing any complications.
The lessons from this case are key to prevent patients with similar situations from unnecessary pain and suffering. Constipation is a common digestive symptom[28]. For adult patients with long-term constipation complicated by cough and hypertension, rare diseases like HD which requires curative and definitive surgery to remove all the aganglionic segment should not be overlooked. The potential reasons for specific symptoms should be actively explored, and notably, symptomatic treatment could not solve the fundamental problems. It is vital to diagnose and cure HD patients in childhood, which could significantly improve the satisfactory functional outcomes[13]. For diagnosed HD, sufficient removal of the non-functional intestineconfirmed by intraoperative frozen section pathology with regular follow-up is essential, and remaining aganglionic segment should be considered if symptoms persist or recur.
The authors would most sincerely thank the reviewer and the editors for critically reviewing this paper and for the constructive and thoughtful comments and suggestions. We are grateful to Ms. Leah Liu for the English language assistance.
A 47-year-old adult female with a history of cesarean section and with digestive unfitness (abdominal pain, distention, and constipation) only since 20 years old had recurrence of digestive symptoms after initial surgery due to the incomplete removal of the affected bowel based on a diagnosis of “chronic ileus”, leading to the relapse of the digestive symptoms and the emergence of some intractable circulatory and respiratory complications which could be hardly controlled by conservative treatment.
“Right-sided” Hirschsprung’s disease (HD) complicated by refractory hypertension and cough with incomplete removal of the affected bowel.
Chronic ileus, chronic constipation, intestinal tuberculosis, inflammatory bowel disease, and toxic megacolon could be differentiated from this case mainly based on pathological examinations.
All laboratory tests were within normal limits except the presence of bacteria in urine (429/μL).
The abdominopelvic computed tomography and the colon double contract pneumobarium radiography revealed significant expansion of the cecum, the ascending colon, the hepatic flexure of colon, and the remnant transverse colon, with the most dilated area 13.6 cm wide.
The pathological report supported the HD diagnosis, showing the remnant aganglionic bowel section left behind by the first surgery.
Right colectomy was conducted to remove the aganglionic and the dilated fragments followed by ileum-colon anastomosis, and the resected intestine included the non-dilated bowel 6 cm beyond the anastomosis of the initial surgery.
HD is an intestinal malformation caused by the innate absence of ganglion cells in the neural plexus of the colorectal wall, and is most common in male infants. It is rare in adult, and is usually left-sided. HD patients mostly suffer from long-term constipation, distention, and bellyache which are not relevant to diet. Conservative treatment does not work satisfactorily for adult HD, which usually requires surgery.
Congenital megacolon (Hirschsprung’s disease) is an intestinal malformation caused by the innate absence or decrease of ganglion cells in the submucosal (Meissner) and myenteric (Auerbach) neural plexuses of the colorectal wall, and dates back to a defect in the craniocaudal migration of the neuroblast originating from the neural crest that occurs during the first 3 mo of gestation. Rarely the whole colon could be aganglionic, which is known as the Zuelzer-Wilson syndrome.
For adult patients with long-term constipation combined with cough and hypertension, rare diseases like HD which requires definite surgery and which could be “right-sided” should not be overlooked, and it is noteworthy that for diagnosed HD, sufficient removal of the non-functional intestine confirmed by intraoperative pathology is essential.
In this case report, the authors reported a case of a female adult patient with “right-sided” congenital megacolon HD complicated by refractory hypertension and cough. It could be helpful to clinical study.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cheng TH, Garcia-Olmo D S- Editor: Qi Y L- Editor: Filipodia E- Editor: Wang CH
| 1. | McCabe ER. Hirschsprung’s disease: dissecting complexity in a pathogenetic network. Lancet. 2002;359:1169-1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | O’Dell K, Staren E, Bassuk A. Total colonic aganglionosis (Zuelzer-Wilson syndrome) and congenital failure of automatic control of ventilation (Ondine’s curse). J Pediatr Surg. 1987;22:1019-1020. [PubMed] |
| 3. | Arshad A, Powell C, Tighe MP. Hirschsprung’s disease. BMJ. 2012;345:e5521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Jarvi K, Laitakari EM, Koivusalo A, Rintala RJ, Pakarinen MP. Bowel function and gastrointestinal quality of life among adults operated for Hirschsprung disease during childhood: a population-based study. Ann Surg. 2010;252:977-981. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 123] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 5. | World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191-2194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16597] [Cited by in RCA: 18258] [Article Influence: 1521.5] [Reference Citation Analysis (0)] |
| 6. | Grimes DA, Hubacher D, Nanda K, Schulz KF, Moher D, Altman DG. The Good Clinical Practice guideline: a bronze standard for clinical research. Lancet. 2005;366:172-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 111] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D. The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol. 2014;67:46-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 407] [Article Influence: 33.9] [Reference Citation Analysis (0)] |
| 8. | Rosin JD, Bargen JA, Waugh JM. Congenital megacolon of a man 54 years of age: report of case. Proc Staff Meet Mayo Clin. 1950;25:710-715. [PubMed] |
| 9. | Sorelli P, Blunt D, Buchanan G. Large bowel obstruction in an adult after Soave for Hirschsprung’s disease in childhood. J Pediatr Surg. 2008;43:546-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Do MY, Myung SJ, Park HJ, Chung JW, Kim IW, Lee SM, Yu CS, Lee HK, Lee JK, Park YS. Novel classification and pathogenetic analysis of hypoganglionosis and adult-onset Hirschsprung’s disease. Dig Dis Sci. 2011;56:1818-1827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Kim HJ, Kim AY, Lee CW, Yu CS, Kim JS, Kim PN, Lee MG, Ha HK. Hirschsprung disease and hypoganglionosis in adults: radiologic findings and differentiation. Radiology. 2008;247:428-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Vorobyov GI, Achkasov SI, Biryukov OM. Clinical features’ diagnostics and treatment of Hirschsprung’s disease in adults. Colorectal Dis. 2010;12:1242-1248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Conway SJ, Craigie RJ, Cooper LH, Turner K, Turnock RR, Lamont GL, Newton S, Baillie CT, Kenny SE. Early adult outcome of the Duhamel procedure for left-sided Hirschsprung disease--a prospective serial assessment study. J Pediatr Surg. 2007;42:1429-1432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Medhus AW, Bjørnland K, Emblem R, Husebye E. Liquid and solid gastric emptying in adults treated for Hirschsprung’s disease during early childhood. Scand J Gastroenterol. 2007;42:34-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Medhus AW, Bjørnland K, Emblem R, Husebye E. Motility of the oesophagus and small bowel in adults treated for Hirschsprung’s disease during early childhood. Neurogastroenterol Motil. 2010;22:154-60, e49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Hartman EE, Oort FJ, Aronson DC, Hanneman MJ, van der Zee DC, Rieu PN, Madern GC, De Langen ZJ, van Heurn LW, van Silfhout-Bezemer M. Critical factors affecting quality of life of adult patients with anorectal malformations or Hirschsprung’s disease. Am J Gastroenterol. 2004;99:907-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 58] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Granström AL, Danielson J, Husberg B, Nordenskjöld A, Wester T. Adult outcomes after surgery for Hirschsprung’s disease: Evaluation of bowel function and quality of life. J Pediatr Surg. 2015;50:1865-1869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Hartman EE, Oort FJ, Visser MR, Sprangers MA, Hanneman MJ, de Langen ZJ, va Heurn LW, Rieu PN, Madern GC, van der Zee DC. Explaining change over time in quality of life of adult patients with anorectal malformations or Hirschsprung’s disease. Dis Colon Rectum. 2006;49:96-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Gunnarsdóttir A, Sandblom G, Arnbjörnsson E, Larsson LT. Quality of life in adults operated on for Hirschsprung disease in childhood. J Pediatr Gastroenterol Nutr. 2010;51:160-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Ito T, Kimura T, Yagami T, Maeda N, Komura M, Ohnishi N, Fujita N, Arai K, Tomioka H, Miyatake S. Megacolon in an adult case of hypoganglionosis, a pseudo-Hirschsprung’s disease: an autopsy study. Intern Med. 2008;47:421-425. [PubMed] |
| 21. | Munakata K, Fukuzawa M, Nemoto N. Histologic criteria for the diagnosis of allied diseases of Hirschsprung’s disease in adults. Eur J Pediatr Surg. 2002;12:186-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Tomita R, Ikeda T, Fujisaki S, Tanjoh K, Munakata K. Hirschsprung’s disease and its allied disorders in adults’ histological and clinical studies. Hepatogastroenterology. 2003;50:1050-1053. [PubMed] |
| 23. | Wilkinson D, Kenny S. Anorectal function is not always normal after surgery in Hirschsprung’s disease. BMJ. 2012;345:e8192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 24. | Jarry J, Faucheron JL. Laparoscopic rectosigmoid resection with transanal colonic pull-through and delayed coloanal anastomosis: a new approach to adult Hirschsprung disease. Dis Colon Rectum. 2011;54:1313-1319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 25. | Duncan ND, Plummer J, Dundas SE, Martin A, McDonald AH. Adult Hirschsprung’s disease in Jamaica: operative treatment and outcome. Colorectal Dis. 2011;13:454-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 26. | Wang L, He Q, Jiang J, Li N. Long-term outcomes and quality of life after subtotal colectomy combined with modified Duhamel procedure for adult Hirschsprung’s disease. Pediatr Surg Int. 2014;30:55-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 27. | Tantiphlachiva K, Rao S. Biofeedback therapy for bowel problems in adults after surgical treatment for childhood Hirschsprung’s disease. Dev Neurorehabil. 2009;12:442-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 28. | Lembo AJ, Schneier HA, Shiff SJ, Kurtz CB, MacDougall JE, Jia XD, Shao JZ, Lavins BJ, Currie MG, Fitch DA. Two randomized trials of linaclotide for chronic constipation. N Engl J Med. 2011;365:527-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 265] [Article Influence: 18.9] [Reference Citation Analysis (0)] |