Published online Jan 28, 2016. doi: 10.3748/wjg.v22.i4.1607
Peer-review started: May 31, 2015
First decision: September 11, 2015
Revised: October 14, 2015
Accepted: November 24, 2015
Article in press: November 24, 2015
Published online: January 28, 2016
Processing time: 237 Days and 3 Hours
Liver transplantation is an effective treatment for patients with end-stage liver disease. Accurate imaging evaluation of the transplanted patient is critical for ensuring that the limited donor liver is functioning appropriately. Ultrasound contrast agents (UCAs), in combination with contrast-specific imaging techniques, are increasingly accepted in clinical use for the assessment of the hepatic vasculature, bile ducts and liver parenchyma in pre-, intra- and post-transplant patients. We describe UCAs, their technical requirements, the recommended clinical indications, image interpretation and the limitations for contrast-enhanced ultrasound applications in liver transplantation.
Core tip: We performed a review of the recent literature on the current status and perspectives of contrast-enhanced ultrasound (CEUS) for liver transplantation. We emphasize some evidence-based diagnostic algorithms to guide clinicians in the assessment of complications. CEUS reduces the need for invasive procedures. Ultrasound is useful for screening for liver transplantation, and the use of CEUS provides more information to enhance the operator’s diagnostic confidence.
- Citation: Ren J, Wu T, Zheng BW, Tan YY, Zheng RQ, Chen GH. Application of contrast-enhanced ultrasound after liver transplantation: Current status and perspectives. World J Gastroenterol 2016; 22(4): 1607-1616
- URL: https://www.wjgnet.com/1007-9327/full/v22/i4/1607.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i4.1607
Liver transplantation is the definitive effective treatment for end-stage liver diseases resulting from various causes[1]. Improvements in surgical techniques, immune-suppressive drug therapy and peri-operative care have improved the success of liver transplantation[2,3]. Accurate imaging evaluation in liver transplantation cases is crucial for the success of the operation. Ultrasound is the primary screening technique in the post-operative period. Ultrasound contrast agents (UCAs), in combination with contrast-specific imaging techniques, are increasingly accepted in clinical use for the assessment of the hepatic vasculature in both pre- and post-transplant patients. Several reviews of the use of contrast-enhanced ultrasound (CEUS) in liver transplantation have been published[4,5]. Since their publication, the types of UCAs and the recommended applications for the assessment of bile ducts and the liver parenchyma in liver transplantation cases have been expanded[6-12]. Therefore, this review is necessary to provide a description of UCAs, their technical requirements, the recommended clinical indications, image interpretation and the limitations for CEUS applications in the pre-, intra- and post-transplant phases.
Three UCAs have previously been described in liver transplantation reports[6-32]. The dynamic enhancement pattern of UCAs is visualized during continuous or intermittent imaging, and UCAs are recommended for various applications: (1) Levovist (air with a galactose and palmitic acid as the surfactant) (Schering, introduced in 1996) was used in initial studies of the assessment of the hepatic vasculature, usually requiring High Mechanical Index (MI) contrast-specific imaging modes or color Doppler ultrasound (CDUS); (2) Optison [octafluoropropane (perflutren) with an albumin shell] (GE Healthcare, introduced in 1998) was introduced to visualize vascular complications in Hom’s report, in which low MI contrast-specific imaging modes were used[24]; and (3) SonoVue (sulfur hexafluoride with a phospholipid shell) (Bracco, introduced in 2001) is the main agent in general use, in combination with low MI contrast-specific imaging modes. Most clinical studies for the hepatic vasculature, liver parenchyma and bile duct examinations have been published using SonoVue.
In addition to intravenous use, UCAs are suitable for intracavitary administration for contrast-enhanced ultrasonic cholangiography (CEUSC)[8-10,33]. However, a standard UCA dosage has not yet been established[34].
The assessment of portal venous system patency and the characterization of portal vein thrombosis (PVT) have evolved into the most important application of CEUS[13,14]. Moreover, the evaluation of hepatic vein (HV) and inferior vena cava (IVC) patency has also been assessed in several reviews[4,5].
Liver transplantation is the appropriate surgical modification for PVT or HCC cases with macrovascular invasion by the tumor because of the high rate of operation failure or tumor recurrence[35-37]. In these cases, the accurate detection and characterization of PVT are very important.
Currently, baseline ultrasound is the preliminary imaging modality for the visualization of the portal venous system. However, this technique is influenced by multiple factors, such as the high reflectivity of cirrhotic liver, associated fatty change, the presence of ascites and overlying bowel gas[15]. Microbubble-enhanced color Doppler ultrasound may be utilized to improve the visualization of the portal vein in up to 94% of patients with inadequate CDUS with a sensitivity of 89% and a specificity of 83%, and the mean diagnosis confidence increases from 45% to 83% following the administration of Levovist[13]. Furthermore, CEUS has also been shown to be very reliable for the characterization of PVT[14]. The superiority of CEUS over contrast-enhanced computed tomography (CT) in the detection (100% vs 68%) and characterization (98% vs 68%) of PVT has been reported by Rossi et al[38].
After the administration of UCAs, the patent portal vein should be visualized adequately in CDUS imaging or low MI contrast-specific imaging, and should be incompletely visualized in the presence of an embolus[13]. The performance differs in benign vs malignant PVT; the former involves a lack of vascularization of the thrombus and an absence of mass-forming features of the thrombus[14], and the latter involves enhancement of the thrombus in the early arterial phase and intrathrombus pulsating enhanced signals with arterial waveforms on Doppler spectral examination[39,40]. A marked washout in the portal and late phases may occur in malignant PVT[41].
CEUS is recommended in clinical situations that involve portal venous thrombosis suspected on the baseline ultrasound. With typical enhancement patterns on CEUS, the characterization of PVT can be performed with a high level of probability and confidence. However, if the baseline ultrasound is very suboptimal, CEUS may be disappointing, and in our preliminary study, 3 in 17 patients with PVT had been missed on CEUS because of the small PVT[42].
In addition to intravascular use, UCAs are suitable for intracavitary administration. Intrabiliary administration of UCAs is performed to intraoperatively visualize the biliary anatomy and variations of living liver donors[8,9].
More than 42% of the population exhibits anatomical biliary tree variations[43]. The evaluation of the biliary anatomy is important for surgical planning and for excluding unsuitable liver donors for living donor liver transplantation (LDLT)[44,45]. However, conventional ultrasound is limited for demonstrating nondilated biliary duct.
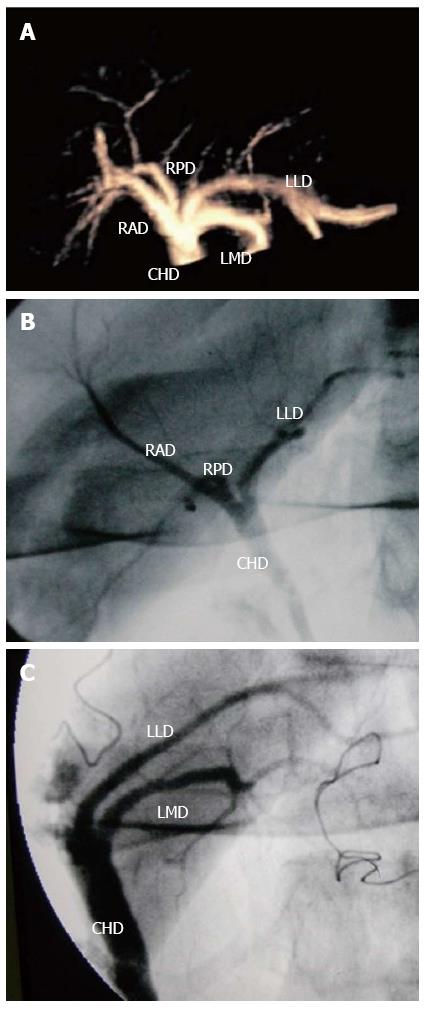
Two-dimensional (2D) CEUSC had been reported to successfully visualize nondilated biliary trees after the injection of UCAs into the bile ducts; this approach represents a potential safe method for the visualization of intrahepatic bile ducts after liver transplantation[10,46]. Xu et al[9] and Zheng et al[8] proposed 3D CEUSC to overcome the limitations of the planar display mode and restricted field of 2D CEUSC in analyzing the biliary spatial relationship and anatomical variations. Their results suggested that 3D CEUSC could visualize the biliary tree from the common hepatic duct to the fifth-order branches, including biliary anatomical variations. Moreover, when the biliary anatomy is unclear on intraoperative cholangiography (IOC), 3D CEUSC might provide a 3-D map of the biliary anatomy and help to reduce the risk of bile duct injury during graft harvesting in LDLT.
After diluted UCA is injected into the common hepatic ducts intraoperatively, the biliary tree from the common hepatic duct (CHD) to the fifth-order branch in the right lobe and fourth-order branch in the left lobe of the liver can be visualized on 3D CEUSC (Figure 1). By varying the angles, overlapped intrahepatic biliary branches could be observed on the 3D CEUSC.
3D CEUSC appears to be appropriate for assessing the biliary spatial relationship and the anatomical variations intra-operationally. However, further studies in larger series of patients are needed, and this technique should be related temporally to other techniques. The image quality and visibility of the left lobe, especially the lateral segment, are poorer than those of the right lobe. Methods of improving the visibility of the left biliary tree will need to be explored.
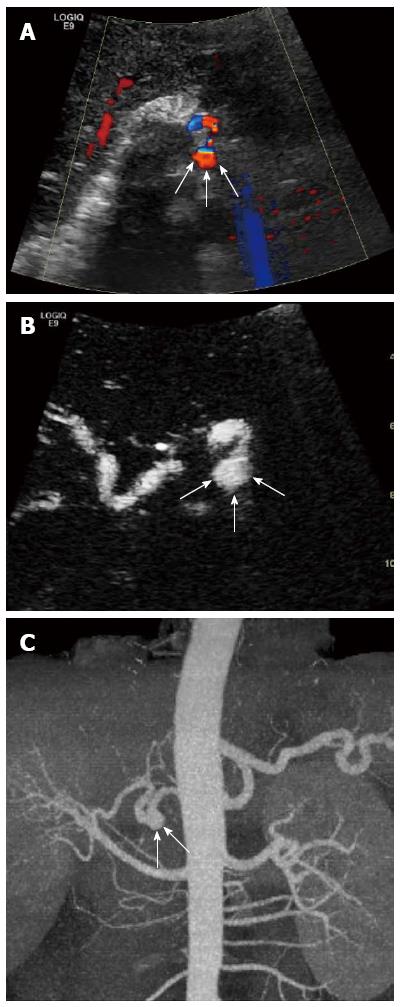
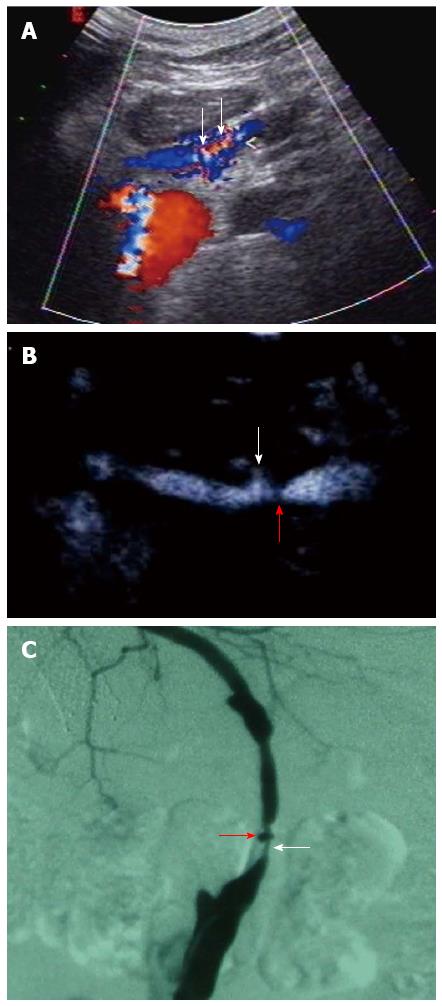
Based on the published literature[12,16,18,19], there is clear evidence that CEUS improves the diagnostic assessment of hepatic artery thrombosis (HAT), hepatic artery stenosis (HAS), and focal liver diseases compared with conventional ultrasound. Some studies have demonstrated that CEUS might be a potential alternative for the evaluation of arterial steal syndrome (ASS), HV obstruction and biliary complications[6,7,20,21,23]. Hepatic artery pseudo-aneurysms assessed using CEUS have only been mentioned in reviews[4,5] (Figures 2 and 3).
HAT is a major cause of graft loss and patient mortality, with an incidence between 2.5% and 9% in adult transplant recipients[47-49]. Early detection of HAT is critical because urgent revascularization is required to avoid severe graft loss. Although ultrasound is the preferred first-line imaging modality in patients with suspected HAT, the accuracy and positive predictive value of HAT on CDUS are reported to be only 64%-82% and 64%-68%, respectively[50-52]. Moreover, Doppler examination of the hepatic vasculature is time-consuming and requires a high level of operator skill.
CEUS has been reported to effectively improve flow visualization of the hepatic artery[24,32] and to shorten the scanning time from 27.4 ± 13.9 min to 9.3 ± 4.5 min compared with CDUS[28], with a 100% sensitivity and 97.8% accuracy for the detection of HAT[16]. The use of CEUS can avoid the need for invasive arteriography in 62.9% of such cases[17]. Thus, HAT has evolved into the most important CEUS application in liver transplantation.
The absence of contrast signal in the arterial phase relative to the adjacent hepatic parenchyma characterizes most HAT cases[16]. It is noteworthy that collateralization around the thrombosed hepatic artery can occur; this feature can be detected on CDUS of the intra-hepatic arterial branches in liver grafts[53] and appears as the intrahepatic artery and a cluster of small vessels at the porta hepatis on CEUS[16].
CEUS has been accepted to be a very reliable modality for the detection of HAT. When CDUS does not provide sufficient visualization of HA after liver transplantation, CEUS should be performed immediately. A negative CEUS result may avoid unnecessary invasive angiography.
HAS is a common complication in 4% to 11% of liver transplant recipients[54,55]. Detecting HAS is important to avoid bile duct injury[56]. The presence of intrahepatic artery tardus parvus waveform is a good screening test for formal arteriography in cases of suspected stenosis, with a 64% specificity and 97% sensitivity[50]. However, it is noteworthy that the tardus parvus waveform is non-specific for HAS and is also observed in severe aorto-celiac atherosclerotic disease, arterial-venous fistula, arterial-biliary fistula, extensive collateralization and massive liver necrosis or systemic hypotension[57]. Therefore, direct visualization of a focal area of stenosis with an increase in velocity measurement (defined as > 2 m/s) on spectral Doppler would be helpful for further diagnosis. The administration of Levovist enhances backscatter signals from the hepatic arteries and thus aids the identification of the elevated velocity associated with extrahepatic artery stenosis[18]. Zheng et al[19] used low MI contrast-specific imaging modes and SonoVue to produce angiographic-like images of the hepatic artery and proposed that CEUS allows the detection of HAS with a sensitivity of 92.3% and a specificity of 87.5%, and also facilitates the identification of the degree and type of stenosis.
After the intravenous administration of SonoVue in combination with low MI contrast-specific imaging modes, CEUS can produce angiographic-like hepatic artery images in the arterial phase. The location, degree and type of vessel stenosis can be visualized (Figure 3).
Although some studies have demonstrated that CEUS is effective for improving diagnostic confidence and providing more HAS information relative to CDUS, inconsistent findings have been published[26]. Several factors may have contributed to the inconsistent results, such as the level of operator skill, the equipment, obesity and overlying bowel gas. Therefore, further studies on this application are needed in a larger series of patients.
ASS is a rare complication after liver transplantation that occurs in 2.9% to 8.4% of patients[20,21]. Due to excessive celiac axis flow diversion to the splenic artery or gastroduodenal artery, patients with ASS may suffer from hepatocyte damage, biliary ischemic damage and acute graft failure. The prompt diagnosis of ASS before the development of clinical manifestations improves the prognosis of these patients[58]. Conventional ultrasound is insufficiently sensitive for distinguishing structural abnormalities in the hepatic artery from low-flow hepatic artery perfusion. Zhu et al[21] proposed that CEUS is an effective imaging modality for the detection of ASS. The appearance of ASS on CEUS was a delayed enhancement of the hepatic artery with a weak contrast peak and prompt enhancement of the portal vein. In contrast to Zhu et al, based on Garcia-Criado’s experience[20], these findings can also be present in patients with other arterial hypoperfusion conditions. It is impossible to differentiate ASS from other causes of hypoperfusion based on the former criteria. In addition to the enhancement patterns of the hepatic artery, small systolic peak waveforms without a diastolic phase on the Doppler after CEUS may be helpful for characterizing ASS.
Recently, Garcia-Criado et al[20] performed a prospective study on 675 consecutive liver transplant patients to establish algorithms to assess the use of CEUS for evaluating the hepatic artery in the immediate post-transplant period. Their results demonstrated that when CDUS cannot detect arterial flow, CEUS should be performed immediately in the same session, even at the bedside. This approach both avoids unnecessary invasive procedures and saves time, which is vital if HAT is present. Moreover, CDUS performed after CEUS in patent hepatic arteries provides functional information to help distinguish HAS from hepatic artery hypoperfusion syndromes. In the latter cases, ASS could be suspected if there is persistence of low arterial flow or abnormal liver function tests.
Biliary complications after liver transplantation, with an incidence between 10% and 30% of patients, are potentially severe complications resulting in liver dysfunction and eventual graft loss[59]. The morphological abnormalities of the biliary tree with dilatation, stenosis, and cholelithiasis detected using imaging methods currently form the main diagnostic basis for biliary complications. However, conventional ultrasound exhibits a sensitivity of only 38% to 68.4% in identifying the main sign of biliary dilatation in liver grafts.
Using a novel application involving injection of UCAs into the bile ducts, CEUS can produce cholangiographic-like images of the biliary tree, which might overcome the limited depiction of the biliary tree morphology on conventional ultrasound. Daneshi et al[11] presented a case report of a biliary-arterial communication in a transplanted liver based on percutaneous CEUSC that was not identified on the baseline ultrasound and subsequent CT examination. Further studies[10] explored the clinical value of CEUSC compared with conventional radiography as a reference method in patients after liver transplantation. CEUSC exhibited comparable results in the detection of all biliary pathologies (including encompassing delayed duodenal outflow, anastomotic stenosis and anastomotic leakage) and image quality. Although CEUSC appears to be a potential bedside test for the visualization of the bile ducts of liver grafts, its diagnostic value remains unknown.
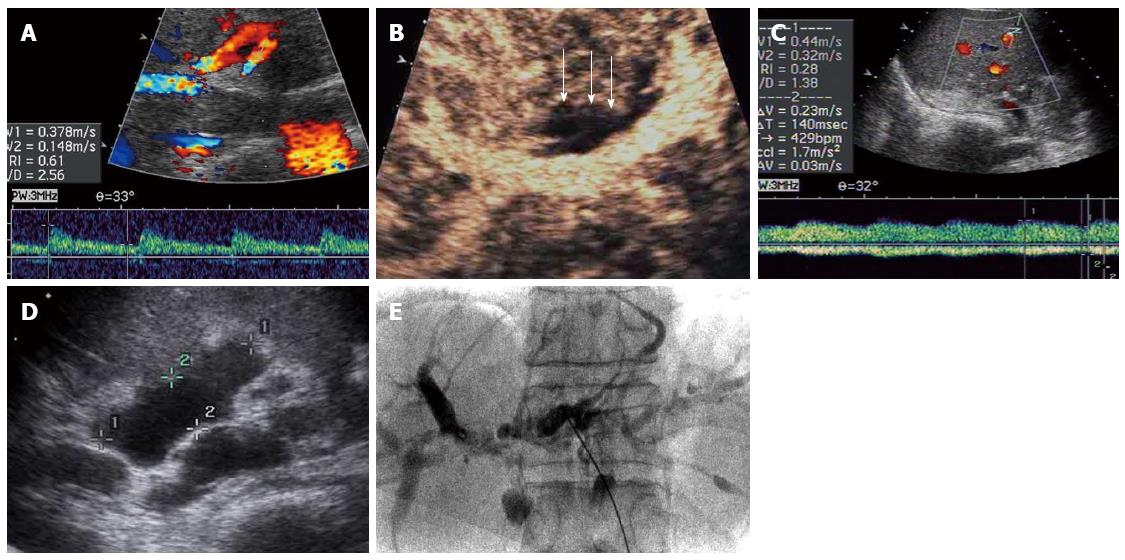
In addition, it is worth noting the shortage of early diagnostic methods for ischemic-type biliary lesions (ITBLs), which are some of the most serious complications. ITBLs vary in incidence from 1% to 19% and exhibit a graft loss rate of 23% and a mortality rate of 7.1%[60-64]. The detection and treatment of early ITBLs could be beneficial to clinical outcomes. However, current biliary morphological signs can be usually visualized in severe ITBLs compared with subtle or mild cases. The biliary tree is supplied solely by the hepatic artery through a network of arterioles and capillaries known as the peribiliary vascular plexus (PBP)[65]. Decreased perfusion caused by injury to the PBP is considered the histological basis of ITBLs. Ren et al proposed that depicting the enhancement patterns of bile duct walls to reveal the microcirculatory changes of the PBP based on intravenous CEUS may help detect early ITBLs. The perfusion of the hilar bile duct wall was successfully demonstrated on CEUS. The main feature differentiating ITBLs from healthy volunteers, recipients without complications and patients without ITBLs was no or low contrast enhancement of the bile duct wall in the arterial phase. This sign might reflect the impaired blood supply to the bile ducts, which was selected as the primary criterion for the diagnosis of ITBLs; the sensitivity, specificity and accuracy were 62.5%-66.7%, 88.9% and 73.8%-76.2%, respectively[7].
On CEUSC, the intra- and extra-hepatic bile duct can be visualized similarly to radiographic cholangiography. The delayed duodenal outflow has been described as decreased signal intensity in the duodenum and persistent high signal intensity in the biliary tree 10 min after the intraductal administration of UCAs. The biliary leakage from the anastomotic region is identified by microbubble accumulation outside of the lumen of the extrahepatic bile duct. The anastomotic stricture represents a diameter discrepancy between the dilated donor and the regular recipient bile duct[10].
On intravenous CEUS, the hilar bile duct walls in patients with ITBLs are characterized by non- or hypo-enhancement relative to the surrounding liver parenchyma in three phases; in healthy volunteers, recipients without complications and patients without ITBLs, hyper-enhancement relative to the normal liver parenchyma in the arterial phase and a similar or lower enhancement in the portal venous and late phases are observed[6,7] (Figure 4).
CEUSC appears to be a potential bedside test for the visualization of the bile ducts of liver grafts, but its diagnostic value should to be determined in further studies.
Although intravenous CEUS exhibits promise for the detection of ITBLs by demonstrating low enhancement patterns of the bile duct walls, whether CEUS could be used for the early diagnosis of ITBLs in the stage of perfusion function changes prior to the appearance of marked morphological changes remains unknown[6]. Animal experiments to explore the correlation between the enhancement patterns and the pathology of the bile duct wall are necessary. In addition, prospective studies should be performed in a series of consecutive patients to detect patients with biliary lesions caused by PBP changes.
LDLT is commonly used and requires the radiologic evaluation of middle hepatic vein (MHV) tributaries to identify hepatic venous obstruction after transplantation. CDUS is the primary screening modality for hepatic venous obstruction, but CDUS often leads to a relatively high false-positive rate in the diagnosis of this disease[65,66]. CEUS has been increasingly applied to the evaluation of hepatic vascular structure after liver transplantation[16-22], and CEUS has been reported to be a promising diagnostic method to detect obstruction of the MHV tributaries[23]. The changes in hepatic parenchymal perfusion on CEUS help to reduce the false-positive rate from 14% to 3% relative to CDUS. CEUS exhibits a diagnostic sensitivity, specificity, and accuracy of 91%, 97%, and 95%, respectively, which is significantly more specific and accurate than CDUS[23].
The detection of hepatic venous obstruction on CEUS is based on the high echogenicity in the arterial phase and low echogenicity or isoechogenicity in the portal venous phase; in the non-obstruction group, the isoechogenicity is observed in the arterial and portal venous phases. Arterial hyperenhancement in the affected area is specific to hepatic venous obstruction[23].
The study used CT as the reference standard for hepatic venous obstruction rather than pathological proof or venography, which may limit the reliability of the diagnostic performance of CDUS or CEUS[23]. Further study should be performed in a nonbiased population to confirm the diagnostic performance of CEUS with respect to hepatic venous obstruction.
Recurrent malignancy, infarction, fluid collections and abscesses are main indications for CEUS.
Patients transplanted for HCC are at a high risk of recurrent malignancy after liver transplantation. CEUS is recommended for the diagnostic strategy for focal liver lesions, including malignant liver lesions[33,67]. Recurrent malignancy characterizes as solid lesions with hypoenhancing in the late phases corresponding to the washout phenomenon.
Parenchymal infarction is the likely complication in suspected vascular compromise such as acute thrombosis, hepatic artery stenosis or iatrogenic restriction of portal flow[5,12]. The diagnosis of infarction is difficult using conventional ultrasound, as the lesions are inconspicuous and as the absence of flow is impossible to detect. CEUS can be used to overcome the limitations of CDUS. The CEUS performance in infarction cases is based on parenchymal geographic areas with a lack of enhancement in three phases, well-defined borders and no peripheral enhancement[12]. In the 2012 update of the guidelines and recommendations for CEUS in the liver[68], CEUS is recommended to exclude perfusion defects when infarction is suspected after liver transplantation and for evaluation of the presence and nature of fluid collections, which may appear as either hyper- or hypo-echoic areas on B-mode imaging.
As the types of UCAs and the contrast-specific imaging modes have increased, CEUS has also been increasingly used in a growing number of clinical settings in pre-, intra- and post-transplant patients. CEUS is a potential safe method even at the bedside avoiding unnecessary invasive tests and saving time, which allows greater diagnostic confidence and provides more information on the basis of conventional ultrasound. Thus, CEUS should be included into the clinical algorithms after liver transplantation. But the CEUS examination may be limited because of surgical wound, subcutaneous emphysema, intervening bowel gas or complex anatomy in patients with split liver transplantation.
P- Reviewer: Morioka D S- Editor: Ma YJ L- Editor: Wang TQ E- Editor: Zhang DN
| 1. | Liou IW. Management of end-stage liver disease. Med Clin North Am. 2014;98:119-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Starzl TE, Demetris AJ, Van Thiel D. Liver transplantation (1). N Engl J Med. 1989;321:1014-1022. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 444] [Cited by in RCA: 393] [Article Influence: 10.9] [Reference Citation Analysis (3)] |
| 3. | Starzl TE, Demetris AJ, Van Thiel D. Liver transplantation (2). N Engl J Med. 1989;321:1092-1099. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 189] [Article Influence: 5.3] [Reference Citation Analysis (3)] |
| 4. | Berry JD, Sidhu PS. Microbubble contrast-enhanced ultrasound in liver transplantation. Eur Radiol. 2004;14 Suppl 8:P96-P103. [PubMed] |
| 5. | Sidhu PS, Marshall MM, Ryan SM, Ellis SM. Clinical use of Levovist, an ultrasound contrast agent, in the imaging of liver transplantation: assessment of the pre- and post-transplant patient. Eur Radiol. 2000;10:1114-1126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Ren J, Lu MD, Zheng RQ, Lu MQ, Liao M, Mao YJ, Zheng ZJ, Lu Y. Evaluation of the microcirculatory disturbance of biliary ischemia after liver transplantation with contrast-enhanced ultrasound: preliminary experience. Liver Transpl. 2009;15:1703-1708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Ren J, Zheng BW, Wang P, Liao M, Zheng RQ, Lu MD, Lu Y, Zeng J, Zhang YL. Revealing impaired blood supply to the bile ducts on contrast-enhanced ultrasound: a novel diagnosis method to ischemic-type biliary lesions after orthotropic liver transplantation. Ultrasound Med Biol. 2013;39:753-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Zheng RQ, Chen GH, Xu EJ, Mao R, Lu MQ, Liao M, Ren J, Kai L, Yi SH. Evaluating biliary anatomy and variations in living liver donors by a new technique: three-dimensional contrast-enhanced ultrasonic cholangiography. Ultrasound Med Biol. 2010;36:1282-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Xu EJ, Mao R, Zheng RQ, Lu MQ, Liao M, Ren J, Li K. Three-dimensional contrast-enhanced ultrasonic cholangiography: a new technique for delineation of the biliary tract in a liver donor. Liver Transpl. 2009;15:1154-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Chopra SS, Eisele R, Stelter L, Seehofer D, Grieser C, Warnick P, Denecke T. Contrast enhanced ultrasound cholangiography via T-tube following liver transplantation. Ann Transplant. 2012;17:108-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 11. | Daneshi M, Rajayogeswaran B, Peddu P, Sidhu PS. Demonstration of an occult biliary-arterial fistula using percutaneous contrast-enhanced ultrasound cholangiography in a transplanted liver. J Clin Ultrasound. 2014;42:108-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Fontanilla T, Noblejas A, Cortes C, Minaya J, Mendez S, Van den Brule E, Hernando CG, Alfageme M, Baños I, Aguirre E. Contrast-enhanced ultrasound of liver lesions related to arterial thrombosis in adult liver transplantation. J Clin Ultrasound. 2013;41:493-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Marshall MM, Beese RC, Muiesan P, Sarma DI, O’Grady J, Sidhu PS. Assessment of portal venous system patency in the liver transplant candidate: a prospective study comparing ultrasound, microbubble-enhanced colour Doppler ultrasound, with arteriography and surgery. Clin Radiol. 2002;57:377-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Piscaglia F, Gianstefani A, Ravaioli M, Golfieri R, Cappelli A, Giampalma E, Sagrini E, Imbriaco G, Pinna AD, Bolondi L. Criteria for diagnosing benign portal vein thrombosis in the assessment of patients with cirrhosis and hepatocellular carcinoma for liver transplantation. Liver Transpl. 2010;16:658-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 77] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 15. | Zhang YC, Qu EZ, Ren J, Zhang Q, Zheng RQ, Yang Y, Chen GH. New diagnosis and therapy model for ischemic-type biliary lesions following liver transplantation--a retrospective cohort study. PLoS One. 2014;9:e105795. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Lu Q, Zhong XF, Huang ZX, Yu BY, Ma BY, Ling WW, Wu H, Yang JY, Luo Y. Role of contrast-enhanced ultrasound in decision support for diagnosis and treatment of hepatic artery thrombosis after liver transplantation. Eur J Radiol. 2012;81:e338-e343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Sidhu PS, Shaw AS, Ellis SM, Karani JB, Ryan SM. Microbubble ultrasound contrast in the assessment of hepatic artery patency following liver transplantation: role in reducing frequency of hepatic artery arteriography. Eur Radiol. 2004;14:21-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 51] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Sidhu PS, Ellis SM, Karani JB, Ryan SM. Hepatic artery stenosis following liver transplantation: significance of the tardus parvus waveform and the role of microbubble contrast media in the detection of a focal stenosis. Clin Radiol. 2002;57:789-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Zheng RQ, Mao R, Ren J, Xu EJ, Liao M, Wang P, Lu MQ, Yang Y, Cai CJ, Chen GH. Contrast-enhanced ultrasound for the evaluation of hepatic artery stenosis after liver transplantation: potential role in changing the clinical algorithm. Liver Transpl. 2010;16:729-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | García-Criado A, Gilabert R, Bianchi L, Vilana R, Burrel M, Barrufet M, Oliveira R, García-Valdecasas JC, Brú C. Impact of contrast-enhanced ultrasound in the study of hepatic artery hypoperfusion shortly after liver transplantation: contribution to the diagnosis of artery steal syndrome. Eur Radiol. 2015;25:196-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Zhu XS, Gao YH, Wang SS, Cheng Q, Ling Y, Fan L, Huo F, Pu MS, Li P. Contrast-enhanced ultrasound diagnosis of splenic artery steal syndrome after orthotopic liver transplantation. Liver Transpl. 2012;18:966-971. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Berstad AE, Brabrand K, Foss A. Clinical utility of microbubble contrast-enhanced ultrasound in the diagnosis of hepatic artery occlusion after liver transplantation. Transpl Int. 2009;22:954-960. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 23. | Park YS, Kim KW, Kim SY, Lee SJ, Lee J, Kim JH, Lee JS, Kim HJ, Song GW, Hwang S. Obstruction at middle hepatic venous tributaries in modified right lobe grafts after living-donor liver Transplantation: diagnosis with contrast-enhanced US. Radiology. 2012;265:617-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 24. | Hom BK, Shrestha R, Palmer SL, Katz MD, Selby RR, Asatryan Z, Wells JK, Grant EG. Prospective evaluation of vascular complications after liver transplantation: comparison of conventional and microbubble contrast-enhanced US. Radiology. 2006;241:267-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 68] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Rennert J, Dornia C, Georgieva M, Roehrl S, Fellner C, Schleder S, Stroszczynski C, Jung EM. Identification of early complications following liver transplantation using contrast enhanced ultrasound (CEUS). First results. J Gastrointestin Liver Dis. 2012;21:407-412. [PubMed] |
| 26. | Bonini G, Pezzotta G, Morzenti C, Agazzi R, Nani R. Contrast-enhanced ultrasound with SonoVue in the evaluation of postoperative complications in pediatric liver transplant recipients. J Ultrasound. 2007;10:99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Clevert DA, Stickel M, Minaifar N, Löhe F, Graeb C, Jauch KW, Reiser M. Contrast-enhanced ultrasound in liver transplant: first results and potential for complications in the postoperative period. Clin Hemorheol Microcirc. 2009;43:83-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Luo Y, Fan YT, Lu Q, Li B, Wen TF, Zhang ZW. CEUS: a new imaging approach for postoperative vascular complications after right-lobe LDLT. World J Gastroenterol. 2009;15:3670-3675. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 19] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Dai X, Zhao HQ, Liu RH, Xu CT, Zheng F, Yu LB, Li WM. Percutaneous radiofrequency ablation guided by contrast-enhanced ultrasound in treatment of metastatic hepatocellular carcinoma after liver transplantation. Asian Pac J Cancer Prev. 2012;13:3709-3712. [PubMed] |
| 30. | Zelinkova Z, Geurts-Giele I, Verheij J, Metselaar H, Dinjens W, Dubbink HJ, Taimr P. Donor-transmitted metastasis of colorectal carcinoma in a transplanted liver. Transpl Int. 2012;25:e10-e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Huang D, Chen Y, Li K, Zhang Q. Hemodynamic changes on color Doppler flow imaging and intravenous contrast-enhanced ultrasound for assessing transplanted liver and early diagnosis of complications. J Huazhong Univ Sci Technolog Med Sci. 2008;28:284-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 32. | Herold C, Reck T, Ott R, Schneider HT, Becker D, Schuppan D, Hahn EG. Contrast-enhanced ultrasound improves hepatic vessel visualization after orthotopic liver transplantation. Abdom Imaging. 2001;26:597-600. [PubMed] |
| 33. | Claudon M, Cosgrove D, Albrecht T, Bolondi L, Bosio M, Calliada F, Correas JM, Darge K, Dietrich C, D’Onofrio M. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) - update 2008. Ultraschall Med. 2008;29:28-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 556] [Cited by in RCA: 499] [Article Influence: 29.4] [Reference Citation Analysis (0)] |
| 34. | Piscaglia F, Nolsøe C, Dietrich CF, Cosgrove DO, Gilja OH, Bachmann Nielsen M, Albrecht T, Barozzi L, Bertolotto M, Catalano O. The EFSUMB Guidelines and Recommendations on the Clinical Practice of Contrast Enhanced Ultrasound (CEUS): update 2011 on non-hepatic applications. Ultraschall Med. 2012;33:33-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 721] [Cited by in RCA: 680] [Article Influence: 52.3] [Reference Citation Analysis (0)] |
| 35. | Kaihara S, Kiuchi T, Ueda M, Oike F, Fujimoto Y, Ogawa K, Kozaki K, Tanaka K. Living-donor liver transplantation for hepatocellular carcinoma. Transplantation. 2003;75:S37-S40. [PubMed] |
| 36. | Malagó M, Sotiropoulos GC, Nadalin S, Valentin-Gamazo C, Paul A, Lang H, Radtke A, Saner F, Molmenti E, Beckebaum S. Living donor liver transplantation for hepatocellular carcinoma: a single-center preliminary report. Liver Transpl. 2006;12:934-940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 44] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 37. | Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5110] [Cited by in RCA: 5310] [Article Influence: 183.1] [Reference Citation Analysis (0)] |
| 38. | Rossi S, Ghittoni G, Ravetta V, Torello Viera F, Rosa L, Serassi M, Scabini M, Vercelli A, Tinelli C, Dal Bello B. Contrast-enhanced ultrasonography and spiral computed tomography in the detection and characterization of portal vein thrombosis complicating hepatocellular carcinoma. Eur Radiol. 2008;18:1749-1756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 101] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 39. | Rossi S, Rosa L, Ravetta V, Cascina A, Quaretti P, Azzaretti A, Scagnelli P, Tinelli C, Dionigi P, Calliada F. Contrast-enhanced versus conventional and color Doppler sonography for the detection of thrombosis of the portal and hepatic venous systems. AJR Am J Roentgenol. 2006;186:763-773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 90] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 40. | Tarantino L, Francica G, Sordelli I, Esposito F, Giorgio A, Sorrentino P, de Stefano G, Di Sarno A, Ferraioli G, Sperlongano P. Diagnosis of benign and malignant portal vein thrombosis in cirrhotic patients with hepatocellular carcinoma: color Doppler US, contrast-enhanced US, and fine-needle biopsy. Abdom Imaging. 2006;31:537-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 116] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 41. | Venturi A, Piscaglia F, Silvagni E, Righini R, Fabbrizio B, Cescon M, Bolondi L. Role of real-time contrast-enhanced ultrasound in the assessment of metastatic portal vein thrombosis. Ultraschall Med. 2007;28:75-78. [PubMed] |
| 42. | Ren J, Zheng RQ, Yan P, Chen J, Mao YJ, Zhang B, Yuan XF. Assessment of portal vein system with contrast-enhanced ultrasound in the liver transplant candidates. Zhongguo Chaosheng Yixue Zazhi. 2007;23:46-48. |
| 43. | Puente SG, Bannura GC. Radiological anatomy of the biliary tract: variations and congenital abnormalities. World J Surg. 1983;7:271-276. [PubMed] |
| 44. | Marcos A, Ham JM, Fisher RA, Olzinski AT, Posner MP. Surgical management of anatomical variations of the right lobe in living donor liver transplantation. Ann Surg. 2000;231:824-831. [PubMed] |
| 45. | Lee VS, Morgan GR, Teperman LW, John D, Diflo T, Pandharipande PV, Berman PM, Lavelle MT, Krinsky GA, Rofsky NM. MR imaging as the sole preoperative imaging modality for right hepatectomy: a prospective study of living adult-to-adult liver donor candidates. AJR Am J Roentgenol. 2001;176:1475-1482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 96] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 46. | Roberts JP, Neill A, Goldstein R. The use of a micro-bubble contrast agent to allow visualization of the biliary tree. Clin Transplant. 2006;20:740-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 47. | Horrow MM, Blumenthal BM, Reich DJ, Manzarbeitia C. Sonographic diagnosis and outcome of hepatic artery thrombosis after orthotopic liver transplantation in adults. AJR Am J Roentgenol. 2007;189:346-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 48. | Stange B, Settmacher U, Glanemann M, Nüssler NC, Bechstein WO, Neuhaus P. Hepatic artery thrombosis after orthotopic liver transplantation. Transplant Proc. 2001;33:1408-1409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 49. | Vivarelli M, Cucchetti A, La Barba G, Bellusci R, De Vivo A, Nardo B, Cavallari A, Pinna AD. Ischemic arterial complications after liver transplantation in the adult: multivariate analysis of risk factors. Arch Surg. 2004;139:1069-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 74] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 50. | Dodd GD, Memel DS, Zajko AB, Baron RL, Santaguida LA. Hepatic artery stenosis and thrombosis in transplant recipients: Doppler diagnosis with resistive index and systolic acceleration time. Radiology. 1994;192:657-661. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 265] [Cited by in RCA: 232] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 51. | Nolten A, Sproat IA. Hepatic artery thrombosis after liver transplantation: temporal accuracy of diagnosis with duplex US and the syndrome of impending thrombosis. Radiology. 1996;198:553-559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 91] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 52. | Harihara Y, Makuuchi M, Takayama T, Kawarasaki H, Kubota K, Ito M, Tanaka H, Aoyanagi N, Matsukura A, Kita Y. Arterial waveforms on Doppler ultrasonography predicting or supporting hepatic arterial thrombosis in liver transplantation. Transplant Proc. 1998;30:3188-3189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 53. | Hall TR, McDiarmid SV, Grant EG, Boechat MI, Busuttil RW. False-negative duplex Doppler studies in children with hepatic artery thrombosis after liver transplantation. AJR Am J Roentgenol. 1990;154:573-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 71] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 54. | Abbasoglu O, Levy MF, Vodapally MS, Goldstein RM, Husberg BS, Gonwa TA, Klintmalm GB. Hepatic artery stenosis after liver transplantation--incidence, presentation, treatment, and long term outcome. Transplantation. 1997;63:250-255. [PubMed] |
| 55. | Wozney P, Zajko AB, Bron KM, Point S, Starzl TE. Vascular complications after liver transplantation: a 5-year experience. AJR Am J Roentgenol. 1986;147:657-663. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 344] [Cited by in RCA: 310] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 56. | Orons PD, Sheng R, Zajko AB. Hepatic artery stenosis in liver transplant recipients: prevalence and cholangiographic appearance of associated biliary complications. AJR Am J Roentgenol. 1995;165:1145-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 88] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 57. | Dravid VS, Shapiro MJ, Needleman L, Bonn J, Sullivan KL, Moritz MJ, Gardiner GA. Arterial abnormalities following orthotopic liver transplantation: arteriographic findings and correlation with Doppler sonographic findings. AJR Am J Roentgenol. 1994;163:585-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 58. | García-Criado A, Gilabert R, Nicolau C, Real I, Arguis P, Bianchi L, Vilana R, Salmerón JM, García-Valdecasas JC, Brú C. Early detection of hepatic artery thrombosis after liver transplantation by Doppler ultrasonography: prognostic implications. J Ultrasound Med. 2001;20:51-58. [PubMed] |
| 59. | Wojcicki M, Milkiewicz P, Silva M. Biliary tract complications after liver transplantation: a review. Dig Surg. 2008;25:245-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 137] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 60. | Hintze RE, Abou-Rebyeh H, Adler A, Veltzke W, Langrehr J, Wiedenmann B, Neuhaus P. [Endoscopic therapy of ischemia-type biliary lesions in patients following orthotopic liver transplantation]. Z Gastroenterol. 1999;37:13-20. [PubMed] |
| 61. | Nakamura N, Nishida S, Neff GR, Vaidya A, Levi DM, Kato T, Ruiz P, Tzakis AG, Madariaga JR. Intrahepatic biliary strictures without hepatic artery thrombosis after liver transplantation: an analysis of 1,113 liver transplantations at a single center. Transplantation. 2005;79:427-432. [PubMed] |
| 62. | Thethy S, Thomson BNj, Pleass H, Wigmore SJ, Madhavan K, Akyol M, Forsythe JL, James Garden O. Management of biliary tract complications after orthotopic liver transplantation. Clin Transplant. 2004;18:647-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 173] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 63. | Sanchez-Urdazpal L, Gores GJ, Ward EM, Maus TP, Buckel EG, Steers JL, Wiesner RH, Krom RA. Diagnostic features and clinical outcome of ischemic-type biliary complications after liver transplantation. Hepatology. 1993;17:605-609. [PubMed] |
| 64. | Dong JH, Zhang LD, Wang SG, Bie P, Yang ZY. [Prophylaxis and management of ischemic-type biliary lesion after orthotopic liver transplantation]. Zhonghua Yi Xue Zazhi. 2006;86:1236-1239. [PubMed] |
| 65. | Takasaki S, Hano H. Three-dimensional observations of the human hepatic artery (Arterial system in the liver). J Hepatol. 2001;34:455-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 45] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 66. | Hwang HJ, Kim KW, Jeong WK, Kim SY, Song GW, Hwang S, Lee SG. Hepatic outflow obstruction at middle hepatic vein tributaries or inferior right hepatic veins after living donor liver transplantation with modified right lobe graft: comparison of CT and Doppler ultrasound. AJR Am J Roentgenol. 2009;193:745-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 67. | Hwang HJ, Kim KW, Jeong WK, Song GW, Ko GY, Sung KB, Shin YM, Kim PN, Ha TY, Moon DB. Right hepatic vein stenosis at anastomosis in patients after living donor liver transplantation: optimal Doppler US venous pulsatility index and CT criteria--receiver operating characteristic analysis. Radiology. 2009;253:543-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 68. | Claudon M, Dietrich CF, Choi BI, Cosgrove DO, Kudo M, Nolsøe CP, Piscaglia F, Wilson SR, Barr RG, Chammas MC. Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver--update 2012: a WFUMB-EFSUMB initiative in cooperation with representatives of AFSUMB, AIUM, ASUM, FLAUS and ICUS. Ultraschall Med. 2013;34:11-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 224] [Article Influence: 18.7] [Reference Citation Analysis (0)] |