Published online Jun 14, 2016. doi: 10.3748/wjg.v22.i22.5293
Peer-review started: March 16, 2016
First decision: March 31, 2016
Revised: April 12, 2016
Accepted: May 4, 2016
Article in press: May 4, 2016
Published online: June 14, 2016
Processing time: 78 Days and 15.5 Hours
We report on a patient diagnosed with Peutz-Jeghers syndrome (PJS) with synchronous rectal cancer who was treated with laparoscopic restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA). PJS is an autosomal dominant syndrome characterized by multiple hamartomatous polyps in the gastrointestinal tract, mucocutaneous pigmentation, and increased risks of gastrointestinal and nongastrointestinal cancer. This report presents a patient with a 20-year history of intermittent bloody stool, mucocutaneous pigmentation and a family history of PJS, which together led to a diagnosis of PJS. Moreover, colonoscopy and biopsy revealed the presence of multiple serried giant pedunculated polyps and rectal adenocarcinoma. Currently, few options exist for the therapeutic management of PJS with synchronous rectal cancer. For this case, we adopted an unconventional surgical strategy and ultimately performed laparoscopic restorative proctocolectomy with IPAA. This procedure is widely considered to be the first-line treatment option for patients with ulcerative colitis or familial adenomatous polyposis. However, there are no previous reports of treating PJS patients with laparoscopic IPAA. Since the operation, the patient has experienced no further episodes of gastrointestinal bleeding and has demonstrated satisfactory bowel control. Laparoscopic restorative proctocolectomy with IPAA may be a safe and effective treatment for patients with PJS with synchronous rectal cancer.
Core tip: Few options currently exist for the therapeutic management of Peutz-Jeghers syndrome with synchronous rectal cancer. Here, we present a patient diagnosed with Peutz-Jeghers syndrome with synchronous rectal cancer treated with laparoscopic restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA). The patient has experienced no further episodes of gastrointestinal bleeding and has demonstrated satisfactory bowel control. To our knowledge, this is the first report on laparoscopic restorative proctocolectomy with IPAA performed for the treatment of Peutz-Jeghers syndrome with synchronous rectal cancer.
- Citation: Zhong ME, Niu BZ, Ji WY, Wu B. Laparoscopic restorative proctocolectomy with ileal pouch-anal anastomosis for Peutz-Jeghers syndrome with synchronous rectal cancer. World J Gastroenterol 2016; 22(22): 5293-5296
- URL: https://www.wjgnet.com/1007-9327/full/v22/i22/5293.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i22.5293
Peutz-Jeghers syndrome (PJS) is a rare, hereditary, autosomal dominant disorder characterized by multiple hamartomatous polyps in the gastrointestinal tract (mainly in the jejunoileum but also in the stomach and colon) and mucocutaneous pigmentation. It has also been reported to be associated with a high risk of malignancy, with a lifetime cancer risk of up to 93%, and it is caused by a germline mutation in the STK11 gene[1,2].
Few options currently exist for the therapeutic management of PJS with synchronous rectal cancer. Surgical strategies are commonly used to treat the sequelae of PJS, such as small bowel intussusception or neoplastic lesions, which may require enterectomy. To date, no studies have focused on PJS patients treated with laparoscopic restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA).
Here, we present a patient diagnosed with PJS with synchronous rectal cancer that was treated with laparoscopic restorative proctocolectomy with IPAA.
A 42-year-old female patient presented with a 20-year history of intermittent bloody stool, poor appetite, abdominal pain and body-weight loss. Twenty years prior, she had experienced occasional abdominal pain, which subsided without treatment. Her family history confirmed that her father and children had similar symptoms. She had presented to our emergency department one month prior with acute gastrointestinal hemorrhaging.
Physical examination showed scattered, punctate, dark-blue areas of pigmentation on her lips (Figure 1) and the distal parts of her fingers. The patient was pale and extremely emaciated. Her body mass index (BMI) was 16. Rectal examination (in the knee-chest position) revealed the presence of a soft mass in the rectal lumen that was 6 cm from the anal verge, approximately 3 cm in diameter, located at nine o’clock, and difficult to move.
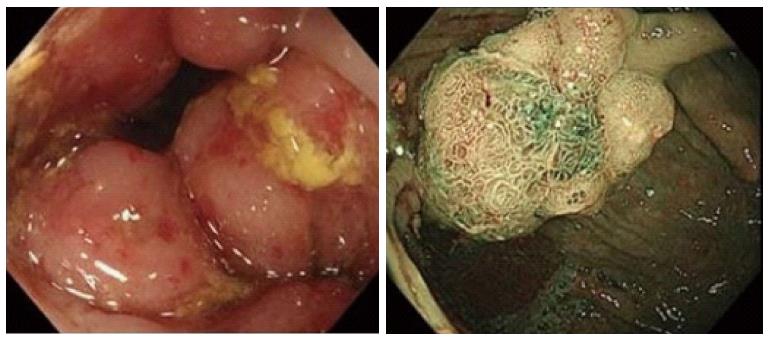
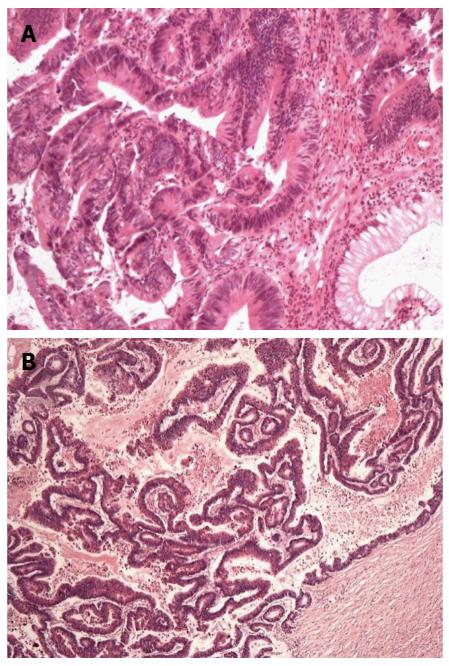
Laboratory tests revealed that she had iron deficiency anemia (69 g/L hemoglobin). Her serum CA125 and serum CEA levels were within the normal limits. A computed tomography scan of the abdomen and pelvis revealed the presence of multiple polyps in the ileum and colorectum. Colonoscopy revealed the presence of multiple serried giant pedunculated polyps, with involvement of the rectum, sigmoid colon, descending colon, transverse colon and part of the ascending colon. In addition, a large cauliflower-like mass was identified at 7 cm from the anal verge (Figure 2). Biopsy of the tumor was performed, which revealed that the cauliflower-like mass was rectal adenocarcinoma (Figure 3A).
Finally, PJS with synchronous rectal adenocarcinoma was diagnosed. Surgical intervention consisting of laparoscopic restorative proctocolectomy and IPAA with a covering ileostomy was performed. During the operation, the patient was noted to have areas of intussusception of the small bowel secondary to the giant polyps. Several adenomatoid polyps were found at locations 30, 50 and 70 cm from the Treitz ligament, and consequently, enterotomy and polypectomy were performed.
The final pathological examination confirmed the diagnosis of moderately differentiated rectal adenocarcinoma (Figure 3B). Of the 37 lymph nodes examined, metastatic adenocarcinoma was detected in 3, and hamartomas with atypical hyperplasia were identified in the polyps, thereby confirming the diagnosis of PJS.
The patient underwent ileostomy closure 6 mo later. After 14 mo of follow-up, no further episodes of gastrointestinal bleeding occurred. This patient has demonstrated satisfactory bowel control to date. Her Wexner incontinence score is zero, indicating that she has no fecal incontinence. Her defecation frequency is 1-2/d. In addition, she is very satisfied with the cosmetic results.
One month ago, this patient underwent gastroenterography, and several polyps were found in the small bowel. As a result, double balloon enteroscopy (DBE) was performed. The ileal polyps were removed using an endoscopic snare.
PJS is an inherited, autosomal dominant disorder with variable inheritance and is characterized by hamartomatous polyps in the gastrointestinal tract, mainly in the small bowel, as well as pigmented mucocutaneous lesions. It is also characterized by increased risks for gastrointestinal and nongastrointestinal cancer. The prevalence of PJS is estimated to be between 1 in 50000 and 1 in 200000 individuals[2].
In this case, the patient had typical manifestations and a family history of PJS. Thus, it was not difficult to diagnose her. In addition, colonoscopy and biopsy revealed the presence of synchronous midrectal cancer.
Few options currently exist for the therapeutic management of PJS with synchronous rectal cancer. Surgical strategies are commonly used to treat the sequelae of PJS, such as small bowel intussusception or neoplastic lesions. Enterotomy and polypectomy or limited resection is considered to be the procedures of choice. Polypectomy using DBE is now recommended for small bowel polyps[3]. DBE is well recognized as a new enteroscopic method that allows for the examination and treatment of the jejunum and ileum in almost all patients. However, it cannot completely replace the surgical treatment of malignancies.
In the present case, we adopted an unconventional surgical strategy and performed laparoscopic restorative proctocolectomy and IPAA with a covering ileostomy.
Laparoscopic restorative proctocolectomy with IPAA is generally considered to be the first-line treatment option for patients with ulcerative colitis or familial adenomatous polyposis (FAP)[4]. However, no previous reports have focused on treating PJS patients with laparoscopic IPAA.
This report describes a patient who presented with severe gastrointestinal hemorrhage. Multiple polyps were found in her gastrointestinal tract, most of which were located in the colorectum and not the small bowl. Giant pedunculated polyps covered the patient’s rectum, sigmoid colon, descending colon, transverse colon and part of the ascending colon, and surgery was necessary. In addition, colonoscopy and biopsy indicated the presence of a midrectal malignancy. Due to the locations of the giant polyps and the midrectal malignancy, restorative proctocolectomy with IPAA was considered. This procedure effectively minimizes the risk of recurrence through the maximal removal of the involved bowel tissue while maintaining bowel continence. A large, retrospective cohort study from the Cleveland Clinic has shown that IPAA is a relatively safe and effective procedure with a low perioperative mortality rate of 0.1%[5]. Compared to conventional laparotomy, laparoscopic restorative proctocolectomy with IPAA is associated with less blood loss, fewer respiratory complications, a faster return of bowel function and a shorter hospital stay[6,7]. In addition, patients are satisfied with laparoscopic surgery[5], which significantly improves cosmesis and quality of life. In this case, the patient has not suffered from further episodes of gastrointestinal bleeding or fecal incontinence since the operation, and she is satisfied with the cosmetic results and the therapeutic effects.
We suggest that laparoscopic restorative proctocolectomy with IPAA may be a safe and effective treatment for PJS with synchronous rectal cancer in patients similar to the one presented in this report. However, this procedure cannot be applied to all patients with PJS. Polyps in the small intestine still require endoscopic polypectomy or resection of the involved regions of the small intestine.
A 42-year-old female patient presented with a 20-year history of intermittent bloody stool. Physical examination showed areas of pigmentation on the lips and extremities.
Peutz-Jeghers syndrome (PJS) with synchronous rectal cancer.
Familial adenomatous polyposis.
The hemoglobin level was 69 g/L, CEA, CA19-9 levels and metabolic panel and liver function test results were within the normal limits.
CT scan revealed the presence of multiple polyps in the ileum and colorectum.
Colonoscopy and biopsy revealed that the rectal mass was an adenoma with high-grade intraepithelial neoplastic changes. The final pathological examination confirmed the diagnosis of moderately differentiated rectal adenocarcinoma.
The patient was treated with laparoscopic restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA).
The authors suggest that laparoscopic restorative proctocolectomy with IPAA may be a safe and effective treatment for treating patients with PJS with synchronous rectal cancer, with the advantage of minimal invasiveness.
In this manuscript, the authors reported a patient with PJS with synchronous rectal cancer who was treated with laparoscopic restorative proctocolectomy with ileal pouch-anal anastomosis. Overall, this case report is very interesting, and worthy to be published.
P- Reviewer: Suzuki A, Tjandra JJ S- Editor: Gong ZM L- Editor: A E- Editor: Wang CH
| 1. | van Lier MG, Wagner A, Mathus-Vliegen EM, Kuipers EJ, Steyerberg EW, van Leerdam ME. High cancer risk in Peutz-Jeghers syndrome: a systematic review and surveillance recommendations. Am J Gastroenterol. 2010;105:1258-1264; author reply 1265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 413] [Cited by in RCA: 329] [Article Influence: 21.9] [Reference Citation Analysis (0)] |
| 2. | Syngal S, Brand RE, Church JM, Giardiello FM, Hampel HL, Burt RW; American College of Gastroenterology. ACG clinical guideline: Genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol. 2015;110:223-262; quiz 263. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 957] [Cited by in RCA: 1090] [Article Influence: 109.0] [Reference Citation Analysis (0)] |
| 3. | Korsse SE, Dewint P, Kuipers EJ, van Leerdam ME. Small bowel endoscopy and Peutz-Jeghers syndrome. Best Pract Res Clin Gastroenterol. 2012;26:263-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Kennedy RD, Zarroug AE, Moir CR, Mao SA, El-Youssef M, Potter DD. Ileal pouch anal anastomosis in pediatric familial adenomatous polyposis: a 24-year review of operative technique and patient outcomes. J Pediatr Surg. 2014;49:1409-1412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Fazio VW, Kiran RP, Remzi FH, Coffey JC, Heneghan HM, Kirat HT, Manilich E, Shen B, Martin ST. Ileal pouch anal anastomosis: analysis of outcome and quality of life in 3707 patients. Ann Surg. 2013;257:679-685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 449] [Cited by in RCA: 527] [Article Influence: 43.9] [Reference Citation Analysis (0)] |
| 6. | Singh P, Bhangu A, Nicholls RJ, Tekkis P. A systematic review and meta-analysis of laparoscopic vs open restorative proctocolectomy. Colorectal Dis. 2013;15:e340-e351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 7. | Buskens CJ, Sahami S, Tanis PJ, Bemelman WA. The potential benefits and disadvantages of laparoscopic surgery for ulcerative colitis: A review of current evidence. Best Pract Res Clin Gastroenterol. 2014;28:19-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |