Published online Apr 14, 2016. doi: 10.3748/wjg.v22.i14.3869
Peer-review started: December 12, 2015
First decision: December 21, 2015
Revised: January 4, 2016
Accepted: January 30, 2016
Article in press: January 30, 2016
Published online: April 14, 2016
Processing time: 108 Days and 12.1 Hours
Esophageal reconstruction can be challenging when stomach and colon are not anatomically intact and their use as esophageal substitutes is therefore limited. Innovative individual approaches are then necessary to restore the intestinal passage. We describe a technique in which a short stump of the right hemicolon and 25 cm of ileum on a long, non-supercharged, fully mobilized ileocolic arterial pedicle were used for esophageal reconstruction to the neck. In this case, a 65 year-old male patient had accidentally indigested hydrochloric acid which caused necrosis of his upper digestive tract. An emergency esophagectomy, gastrectomy, duodenectomy, pancreatectomy and splenectomy had been performed in an outside hospital. A cervical esophagostomy and a biliodigestive anastomosis had been created and a jejunal catheter for enteral feeding had been placed. After the patient had recovered, a reconstruction of his food passage via the left and transverse colon failed for technical reasons due to an intraoperative necrotic demarcation of the colon. Our team then faced the situation that only a short stump of the right hemi-colon was left in situ when the patient was referred to our center. After intensified nutritional therapy, we reconstructed this patient’s food passage with the right hemicolon-approach described herein. After treatment of a postoperative pneumonia, the patient was discharged from hospital on the 26th postoperative day in a good clinical condition on an oral-only diet. In conclusion, individual approaches for long-segment reconstruction of the esophagus can be technically feasible in experienced hands. They do not always require arterial supercharging or free intestinal transplantation.
Core tip: Esophageal reconstructions are more challenging than usual when the stomach and the colon are not available as substitutes for esophageal replacement. In this case, hydrochloric acid had caused severe caustic injuries to the upper digestive tract requiring esophagectomy, gastrectomy, duodenectomy, pancreatectomy and splenectomy in a 65-year-old patient. The initial reconstruction failed, leaving only a short stump of the right hemicolon in situ. We then reconstructed the intestinal passage utilizing this short part of the right hemicolon and 25 cm of ileum on a long, non-supercharged, fully mobilized ileocolic arterial pedicle.
- Citation: Weiss AR, Hackl C, Soeder Y, Schlitt HJ, Dahlke MH. Ileo-right hemi-colonic cervical pull-up on a non-supercharged ileocolic arterial pedicle: A technical and case report. World J Gastroenterol 2016; 22(14): 3869-3874
- URL: https://www.wjgnet.com/1007-9327/full/v22/i14/3869.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i14.3869
Malignant tumors of the esophagus and the esophagogastric junction, as well as caustic injuries and perforations are among the prime indications for resections of the esophagus. All esophagogastric resections with reconstruction are associated with significant morbidity and mortality. A gastric tube is preferably used to reconstruct the food passage after esophagectomy as it usally comes along with a reliable blood supply and only one single anastomosis is necessary for reconstruction. The situation becomes more difficult when the stomach is not available for reconstruction. In these cases, either a pedicled colonic or jejunal interposition or a free jejunal graft can be used. Pedicled interposition grafts always come along with limitations of the blood supply. This is especially relevant towards the oral part of the graft, which - if insufficient - can lead to anastomotic leakage or, in the worst case, to partial or complete necrosis of the pull-up. Necrotic complications then frequently lead to life threatening secondary problems. Recently published studies demonstrate the benefit of additional arterial and venous supercharging, which may improve the blood supply of the graft or pull-up and can therefore reduce the incidence of graft loss and anastomotic leakage[1-4].
When the initial reconstruction fails and a salvage operation with limited intestinal resources for reconstruction has to be planned, the situation can be further complicated. This case report introduces an individual approach of a secondary reconstruction of the food passage with an ileo-right hemi-colonic cervical pull-up on a non-supercharged ileocolic arterial pedicle after a first colonic reconstruction had failed.
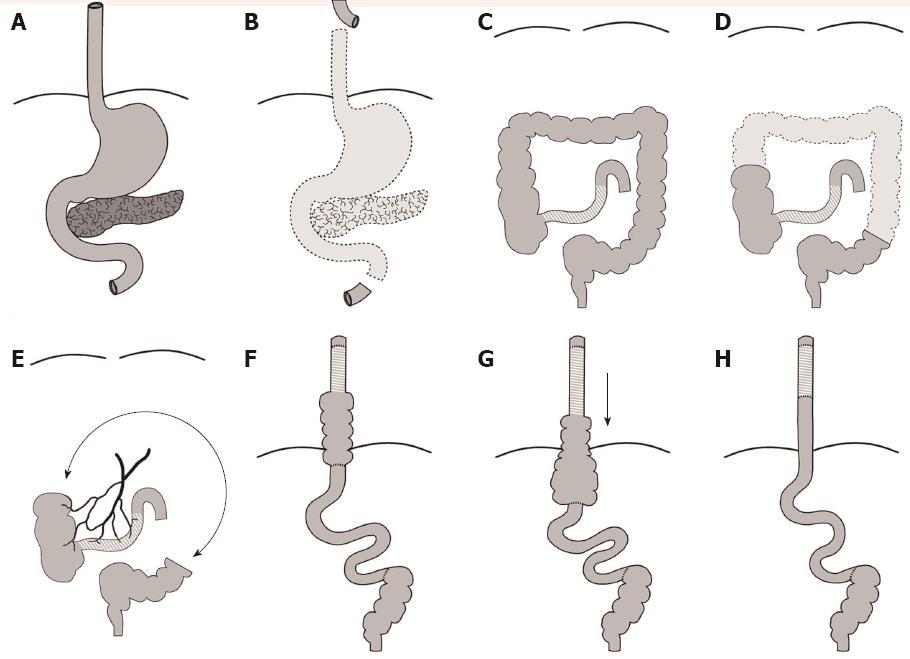
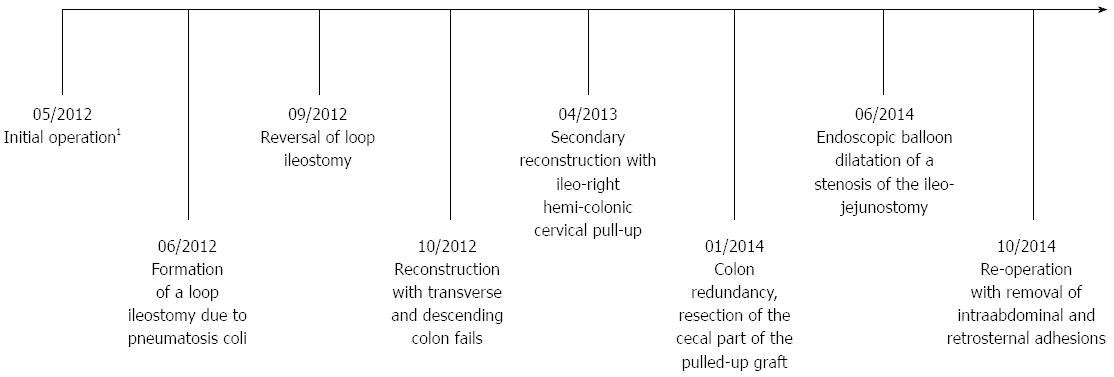
A 65-year-old male patient had accidentally indigested hydrochloric acid which caused a necrosis of his upper digestive tract. In an emergency surgery, an esophagectomy, gastrectomy, duodenectomy, pancreatectomy and splenectomy were performed (Figure 1A and B). At the end of this first operation, a cervical esophagostomy and a choledocho-jejunostomy were created. Furthermore, a jejunal catheter for enteral feeding was inserted.
One month later, an exploratory laparotomy was performed due to a massive pneumoperitoneum and suspected bowel perforation diagnosed in a routine chest X-ray after the placement of a central venous catheter. During surgery, pneumatosis coli without perforation were detected, most likely based on an antibiotic-associated colitis (C. difficile toxin negative). Colon resection was renounced due to missing clinical symptoms and a planned esophageal reconstruction via a colonic interposition. Instead, a protective loop ileostomy was formed and reversed three months later.
After the patient had recovered, five months after the first surgery, a reconstruction of the food passage with a colonic pull-up using the transverse and descending colon was attempted. The reconstruction failed due to an intraoperative ischemic demarcation of the colon, leaving only a short oral part of the ascending colon and approximately 40 cm of the descending colon in situ (Figure 1C, D and E). The colonic remnants were connected via a colo-colonic anastomosis.
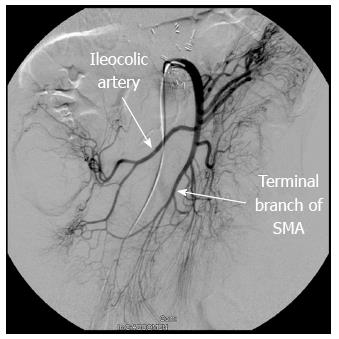
Eight months after the first surgery, the patient contacted our team seeking alternative reconstruction options for his intestinal passage. In the meantime, the patient was in a poor nutritional condition (BMI 16.1) and was fed exclusively via the jejunal catheter. The patient was admitted to our surgical ward for an intensified nutritional therapy to improve his body weight and constitution. Furthermore, an angiography of the patient’s mesenteric arteries was performed, which revealed a sufficient blood supply of the remaining right hemicolon and the terminal ileum via the ileocolic artery (Figure 2). Fortunately, the ileocolic artery formed a tight loop with the terminal jejunal branch of the superior mesenteric artery, which was used later as described below. The patient was discharged from hospital for further home-based nutritional therapy and readmitted for surgery two months later.
After readmission, the patient’s food passage was reconstructed via a retrosternal ileo-right hemi-colonic cervical pull-up on a non-supercharged ileocolic arterial pedicle. During surgery, the ileocecal region and the remaining ascending colon were mobilized and the ileum was transected about 25 cm proximal to Bauhin’s valve. The ileocolic artery was fully mobilized to its origin from the superior mesenteric artery by meticulous micro-preparation and then dissected to use the full length of both branches of the artery. After a sufficient blood supply of the pedicled graft was ensured, the ileum was pulled up to the neck retrosternally and anastomosed end-to-side in an iso-peristaltic fashion to the esophageal stump with a tension-free running manual suture. To achieve this position, the ileocolic artery was turned upwards to a 180° angle. The stump of the ascending colon was then anastomosed end-to-side to the proximal end of the jejunum. Finally, the neo-terminal ileum was anastomosed to the stump of the remaining descending colon (Figure 1F).
The following day, a scheduled second look laparotomy was performed to confirm a sufficient blood supply of the interposition graft. During the postoperative course on the intensive care unit the patient developed severe pneumonia, which was treated with antibiotics, chest tubes and intensified respiratory and positioning therapy. After further stabilization, the patient could be transferred to the general ward on the 13th postoperative day. Stepwise return to a normal diet was well tolerated. A contrast X-ray swallow showed a smooth passage of a soft bolus. The patient was discharged from hospital in a good clinical condition on the 26th postoperative day on an oral-only diet.
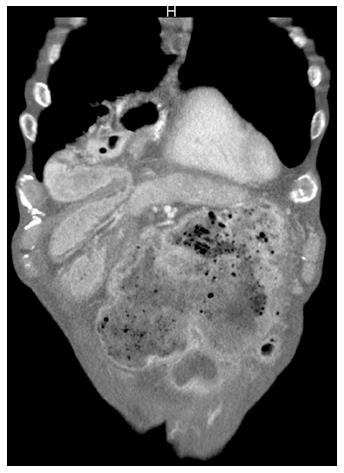
During the following months, the patient suffered from episodes of dysphagia, recurrent nausea and air regurgitation. Additional work-up showed significant dilatation of the pulled-up cecum so that another operation became necessary. Intraoperative assessment revealed that the cecal part of the pulled-up pedicled graft had moved downwards significantly (likely due to gravital challenge in an upright position) from the thoracic cavity through the diaphragm into the abdomen. The cecum was massively dilated and seen as the cause for dysphagia and bowel obstruction as the distal anastomosis was kinked (Figures 3 and 1G). Hence, the ileocecal region was resected and an ileo-jejunostomy was created (Figure 1H). No further complications occurred in the postoperative course and the patient was discharged from hospital on the 12th postoperative day.
A few months later, the patient complained about new symptoms of dysphagia, which were due to a stenosis of the ileo-jejunostomy. The stenosis could successfully be dilated by endoscopic balloon dilatation. Similar symptoms reappeared, this time due to intraabdominal and retrosternal adhesions that were removed in yet another reoperation via a re-laparotomy and a lower partial sternotomy.
During the whole treatment episode at our hospital, the patient had regular appointments with our nutritional experts who adjusted his diet to his special needs (including the substitution of pancreatic enzymes and vitamins). In the last outpatient follow-up examination 32 mo after reconstruction, the patient’s bodyweight was still below average (BMI 17.5) but stable under oral-only food intake without the need for additional enteral or parenteral nutrition and no symptoms of dysphagia (see timeline, Figure 4). He lives an independent life.
In selected cases where the stomach cannot be used for reconstruction of the enteric passageway after esophagectomy, several techniques have been described: pedicled colonic grafts have the advantage that longer conduits can be formed to reconstruct the passage up to the neck when compared to pedicled jejunal grafts. On the downside, colonic enterobacteria pose a higher risk for pulmonary complications in the postoperative course and stenoses and graft redundancy are more frequent in colonic than in jejunal interpositions[1,5,6]. Pedicled jejunal grafts are limited in length due to the shorter mesenteric arcades[7]. Moreover, the diameter of the jejunum is usually more congruent to the diameter of the esophagus and jejunal grafts fit easier through the thoracic inlet in case of retrosternal pull-up. Other advantages of jejunal grafts are a better food transit due to the physiologic peristalsis of the jejunum and a lower risk for intrinsic disease such as hemorrhage or the development of graft carcinoma[8].
All grafts to restore the intestinal continuity after near-total esophagectomy need to be moved up to the cervical esophagus without major tension. This is usually more difficult for jejunal than for colonic grafts and becomes the more complicated the longer the distance to the esophageal stump is. Tension to the anastomosis regularly results in an insufficient blood supply of the graft and can lead to anastomotic leakage or graft necrosis, the most feared complications of these procedures. Thus, supercharging techniques have been introduced using additional arterial and venous anastomoses to vessels located in the neck or chest regions. Several studies demonstrated the benefit of this approach showing that it can improve blood supply to the graft and consequently reduce the incidence of graft necrosis and anastomotic leakage[1-4,7,9]. Since the introduction of the supercharging technique, pedicled jejunal grafts with these anastomoses have become more relevant in the reconstruction of esophageal defects and some authors prefer the jejunum instead of the colon for these purposes[1,7]. However, supercharging is technically challenging and requires microvascular anastomoses, which come along with another array of possible vascular complications.
In case of limited esophageal defects, free jenunal or colonic grafts are an alternative with good postoperative results[10-13]. Right hemi-colonic pull-ups can also be used for esophageal replacement when long enough[14]. In our case, only a short stump of the right hemi-colon was left. Hence, a far longer segment of the terminal ileum had to be chosen to gain enough length for a pull-up to the neck. Accomplishing this without arterial supercharging would have been inconceivable without a previous angiography of the mesenteric arteries with meticulous planning on how to gain maximum length out of it. Using the full length of the ileocolic artery finally made this pull-up possible in the reported case. We thus suggest that preoperative angiography of the mesenteric vessels should be regularly used to ensure a reliable blood supply of the graft and therefore reduce the incidence of graft necrosis and anastomotic leakage[15].
Long-segment esophageal reconstructions without the stomach are demanding and need individual planning of the experienced surgeon and his team. Such reconstructions do not always require arterial supercharging. To prevent graft loss and anastomotic leakage due to insufficient blood supply, preoperative angiography with thorough planning of the expected circulatory situation and vessel length can be recommended. Individual approaches for esophageal reconstructions can then be feasible and restore quality of life.
A 65-year-old patient with caustic injury requiring emergency esophagectomy, gastrectomy, duodenectomy, pancreatectomy and splenectomy.
Inability of oral food intake due to discontinuity resection of the esophagus and failed reconstruction with left and transverse colon.
Signs of malnutrition with hypoalbuminemia and vitamin B12 deficiency.
Angiography of the superior mesenteric artery reveals blood supply of the ileocecal region with the formation of a tight loop between the ileocolic artery and the terminal jejunal branch of the superior mesenteric artery.
Secondary reconstruction of the food passage with ileo-right hemi-colonic cervical pull-up after the initial reconstruction with left and transverse colon failed, followed by resection of the cecal part of the pulled-up graft due to colon redundancy, endoscopic balloon dilatation of a stenosis of the ileo-jejunostomy and re-operation with removal of retrosternal and intraabdominal adhesions.
A preoperative angiography of the mesenteric arteries might show different or new aspects of possible esophageal substitutes.
Pedicled grafts remain connected to their original blood supply and are therefore limited in length. Supercharging describes a method to improve the blood supply of a pedicled graft by adding an additional blood supply via microvascular anastomoses to local vessels in the area of application.
Esophageal reconstructions are still associated with a high morbidity and mortality. In complicated cases with limited intestinal resources, individual approaches can be feasible to restore the patient´s quality of life.
This is a very good clinical case report with an interesting topic.
P- Reviewer: Can G, Majbar MA S- Editor: Qi Y L- Editor: A E- Editor: Ma S
| 1. | Blackmon SH, Correa AM, Skoracki R, Chevray PM, Kim MP, Mehran RJ, Rice DC, Roth JA, Swisher SG, Vaporciyan AA. Supercharged pedicled jejunal interposition for esophageal replacement: a 10-year experience. Ann Thorac Surg. 2012;94:1104-1111; discussion 1111-1113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Fujita H, Yamana H, Sueyoshi S, Shima I, Fujii T, Shirouzu K, Inoue Y, Kiyokawa K, Tanabe HY, Tai Y. Impact on outcome of additional microvascular anastomosis--supercharge--on colon interposition for esophageal replacement: comparative and multivariate analysis. World J Surg. 1997;21:998-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 3. | Kesler KA, Pillai ST, Birdas TJ, Rieger KM, Okereke IC, Ceppa D, Socas J, Starnes SL. “Supercharged” isoperistaltic colon interposition for long-segment esophageal reconstruction. Ann Thorac Surg. 2013;95:1162-1168; discussion 1168-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Sekido M, Yamamoto Y, Minakawa H, Sasaki S, Furukawa H, Sugihara T, Nohira K, Yajima K, Shintomi Y, Okushiba S. Use of the “supercharge” technique in esophageal and pharyngeal reconstruction to augment microvascular blood flow. Surgery. 2003;134:420-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Chirica M, Veyrie N, Munoz-Bongrand N, Zohar S, Halimi B, Celerier M, Cattan P, Sarfati E. Late morbidity after colon interposition for corrosive esophageal injury: risk factors, management, and outcome. A 20-years experience. Ann Surg. 2010;252:271-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 6. | Greene CL, DeMeester SR, Augustin F, Worrell SG, Oh DS, Hagen JA, DeMeester TR. Long-term quality of life and alimentary satisfaction after esophagectomy with colon interposition. Ann Thorac Surg. 2014;98:1713-1719; discussion 1719-1720. [PubMed] |
| 7. | Doki Y, Okada K, Miyata H, Yamasaki M, Fujiwara Y, Takiguchi S, Yasuda T, Hirao T, Nagano H, Monden M. Long-term and short-term evaluation of esophageal reconstruction using the colon or the jejunum in esophageal cancer patients after gastrectomy. Dis Esophagus. 2008;21:132-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Jeyasingham K, Lerut T, Belsey RH. Revisional surgery after colon interposition for benign oesophageal disease. Dis Esophagus. 1999;12:7-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 9. | Poh M, Selber JC, Skoracki R, Walsh GL, Yu P. Technical challenges of total esophageal reconstruction using a supercharged jejunal flap. Ann Surg. 2011;253:1122-1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Hackl C, Popp FC, Ehehalt K, Dendl LM, Benseler V, Renner P, Loss M, Dolderer J, Prantl L, Kühnel T. Retrograde stapling of a free cervical jejunal interposition graft: a technical innovation and case report. BMC Surg. 2014;14:78. [PubMed] |
| 11. | Okumura Y, Mori K, Yamagata Y, Fukuda T, Wada I, Shimizu N, Nomura S, Iida T, Mihara M, Seto Y. Two-stage operation for thoracic esophageal cancer: esophagectomy and subsequent reconstruction by a free jejunal flap. Surg Today. 2014;44:395-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Shirakawa Y, Naomoto Y, Noma K, Ono R, Nobuhisa T, Kobayashi M, Fujiwara T, Noguchi H, Ohkawa T, Yamatsuji T. Free jejunal graft for hypopharyngeal and esophageal reconstruction. Langenbecks Arch Surg. 2004;389:387-390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Noguchi T, Uchida Y, Hashimoto T, Wada S, Takeno S, Suzuki M. Reconstruction of the cervical esophagus using a free transverse colonic graft: report of a case with upper esophageal web and carcinoma. Dis Esophagus. 2003;16:135-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Hamai Y, Hihara J, Emi M, Aoki Y, Okada M. Esophageal reconstruction using the terminal ileum and right colon in esophageal cancer surgery. Surg Today. 2012;42:342-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Predescu D, Popa B, Gheorghe M, Predescu I, Jinescu G, Boeriu M, Constantinoiu S. The vascularization pattern of the colon and surgical decision in esophageal reconstruction with colon. A selective SMA and IMA arteriographic study. Chirurgia (Bucur). 2013;108:161-171. [PubMed] |