Published online Feb 14, 2015. doi: 10.3748/wjg.v21.i6.1759
Peer-review started: May 22, 2014
First decision: June 10, 2014
Revised: July 8, 2014
Accepted: July 24, 2014
Article in press: July 25, 2014
Published online: February 14, 2015
Processing time: 265 Days and 17.4 Hours
AIM: To hypothesize that beta-7 integrin affects cellular migration of both, lymphocytes and enterocytes.
METHODS: The nucleoside analog BrdU was ip injected in beta-7-deficient mice (C57BL/6-Itgbtmlcgn/J) of male gender and age-matched male C57BL/J J mice (wild type) 4, 20, or 40 h before analysis. The total small intestine was isolated, dissected, and used for morphometrical studies. BrdU-positive epithelial cells were numbered in at least 15 hemi-crypts per duodenum, jejunum, and ileum of each animal. The outer most BrdU-positive cell (cellmax) was determined per hemi-crypt, numerically documented, and statistically analysed.
RESULTS: Integrins containing the beta-7-chain were exclusively expressed on leukocytes. In the small intestinal mucosa of beta-7 integrin-deficient mice the number of intraepithelial lymphocytes was drastically decreased. Moreover, the Peyer’s patches of beta-7 integrin-deficient mice appeared hypoplastic. In beta-7 integrin-deficient mice the location of cellmax was found in a higher position than it was the case for the controls. The difference was already detected at 4 h after BrdU application, but significantly increased with time (40 h after BrdU injection) in all small intestinal segments investigated, i.e., duodenum, jejunum, and ileum. Migration of small intestinal enterocytes was different between the experimental groups measured by cellmax locations.
CONCLUSION: The E-cadherin beta-7 integrin pathway probably controls migration of enterocytes within the small intestinal surface lining epithelial layer.
Core tip: Integrins are involved in migration of epithelial and non-epithelial cells. beta-7-chain integrins are exclusively expressed on leukocytes and important for homing of lymphocytes into the intestinal mucosa. In beta-7 integrin-deficient mice, the number of intraepithelial lymphocytes is drastically decreased and accompanied by a significant increase in enterocyte migration along the crypt-villus axis. This phenomenon is probably mediated by the E-cadherin beta-7 integrin pathway.
- Citation: Kaemmerer E, Kuhn P, Schneider U, Clahsen T, Jeon MK, Klaus C, Andruszkow J, Härer M, Ernst S, Schippers A, Wagner N, Gassler N. Beta-7 integrin controls enterocyte migration in the small intestine. World J Gastroenterol 2015; 21(6): 1759-1764
- URL: https://www.wjgnet.com/1007-9327/full/v21/i6/1759.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i6.1759
Intestinal surface lining epithelial cells include enterocytes, goblet cells, enterochromaffine cells, M-cells, and Paneth cells. All of these cell types are continuously replaced within a couple of days. This process is supported by cellular migration along the crypt-villus axis (CVA) or crypt-plateau axis[1-3]. Enterocyte migration essentially contributes to configuration and homeostasis of the intestinal mucosal barrier and plays a pivotal role in mucosal healing after inflammatory or non-inflammatory injuries[4]. It is suggested that in the intestine differentiation and behaviour of epithelial cells are modified by lymphoid cells[5,6].
A plethora of molecular mechanisms and pathways is involved in coordination of epithelial and non-epithelial cell movement[7,8]. Important steps in cellular migration are G-protein-mediated cellular polarisation with local increase in phosphatidylinositol-3,4,5-triphosphate, activation of Rho GTPases, and a synergism of actin polymerisation with the Wiskott-Aldrich syndrome protein/WASP-family verprolin-homologous protein and Arp2/3-complex forming lamellipodia, filopodia, podosomes or invadopodia[9-12].
Integrins are trans-membrane cell adhesion receptors connecting the extra- and intracellular environments by binding to ligands or structures outside the cell and cytoskeletal components or signalling molecules inside the cell[13]. They are heterodimers, consisting of non-covalently associated alpha and beta chains. The composition of diverse alpha and beta subunits determines the plasticity and diversity in ligand recognition and signalling of integrins[14]. The integrin binding specificity is determined by the extracellular domain recognizing diverse matrix ligands including fibronectin, collagen, and laminin. Modification of the integrin heterodimer repertoire can cause altered cellular migration, including more invasive phenotypes[8]. Size, morphology, and location of integrin-based adhesions strongly depend on the cell type and its environment. Several beta subunits are preferentially expressed by immune cells. Especially, beta-2 and beta-7 integrins are exclusively found on leukocytes[13].
Beta-7 integrin can form heterodimers with either the alpha4 or the alphaE subunit. Beta-7 integrins were characterized as important molecular structures in formation of the gut-associated lymphoid tissue (GALT)[15]. Alpha-4 beta-7 integrin binds to mucosal addressin cell adhesion molecule-1 (MAdCAM-1), which is constitutively expressed on intestinal endothelial cells and facilitates the retention of lymphocytes in the gut epithelium via E-cadherin[16]. Whereas beta-7 integrin-deficient mice display a significant reduction of intra-epithelial lymphocytes (IELs), lamina propria lymphocytes, hypoplasia of Peyer’s patches, and a reduced number of IgA- and IgM-producing cells in the small intestine, alphaE integrin-deficient mice exhibit reduced numbers of IELs[17].
Here we concentrate on a detailed evaluation of the impact of beta-7 integrin on enterocyte migration in the small intestinal mucosa of mice.
For the present study beta-7-deficient mice (C57BL/6-Itgbtmlcgn/J[15]) of male gender and age-matched male C57BL/J J mice (wild type) were used. All animals were bred at the core facility of the University Hospital Aachen under specific pathogen-free conditions. In order to analyse intestinal epithelial cellular migration, all mice received a single ip injection of the nucleoside analog BrdU (30 μg/g mouse; Applichem, Cheshire, CT) 4, 20, or 40 h before sacrificing. All procedures were approved by the authority for environment conservation and consumer protection of the state North Rhine-Westfalia (LANUV, Germany).
After sacrificing, the total small intestine was isolated and dissected. Afterwards, the intestinal tissues (duodenum, jejunum, and ileum) were fixed for 24 h in neutral buffered formalin and automatically processed to paraffin. A binocular loupe was used for orthogonal orientation of tissues in paraffin. From each paraffin-embedded tissue block, sections of 3-5 μm were performed and stained with hematoxylin-eosin (HE).
For morphometric procedures, tissue sections were inspected with a Nikon Eclipse 80i microscope (Nikon, Düsseldorf, Germany). Up to 50 hemi-crypts per animal were evaluated (about 15 hemi-crypts per duodenum, jejunum, and ileum). Criteria for small intestinal hemi-crypts were adapted from a previously published study[18]: (1) a single epithelial layer is visible from crypt basis to villus tip; (2) crypt basis without any distension; (3) open crypt lumen; (4) between crypt and villus a small plateau is visible; (5) crypt height 1/4 to 1/3 of the total CVA; and (6) in each villus, the lamina propria mucosae is visible.
Serial sections of morphologically proved intestinal tissues were prepared and immunostained against BrdU[2]. After blocking, DNA-incorporated BrdU was detected with anti-BrdU antibodies (GE Healthcare, Freiburg, Germany). Antibody-binding was visualized with the MOM Kit and DAB as a chromogen (both from Vector, Burlingame, United States). Anti-CD3 immunostainings were performed using a rabbit polyclonal anti-CD3 antibody (Abcam, Cambridge, United Kingdom) in a dilution 1:100. For antibody detection the ImmPRESS system (Vector, Burlingame, CA) and DAB as chromogen were applied.
For each animal BrdU-positive, epithelial cells were numbered in 50 hemi-crypts per animal along the small intestine (about 15 hemi-crypts per duodenum, jejunum, and ileum) following previously published procedures[1,2]. BrdU-positive epithelial cells were characterized with “1”, BrdU-negative epithelial cells with “0”. In each hemi-crypt, the outer most BrdU-positive cell (cellmax) was determined and numerically documented. Histomorphological evaluations were performed by two morphologically experienced investigators (Kuhn P and Gassler N) using a Nikon Eclipse 80i microscope (Nikon).
For each time point of the study three animals per group (nij = 3) were used. Data of 50 hemi-crypts per small intestine (about 15 hemi-crypts per duodenum, jejunum, and ileum) and animal were summarized and the median was calculated. The same data were used for the analysis of variance reflecting mouse type and time course (4, 20 or 40 h). Data were processed using Excel-based algorithms and SAS-based procedures. Standard deviations of the means were indicated by error bars. P-values of less than 0.05 were considered significant.
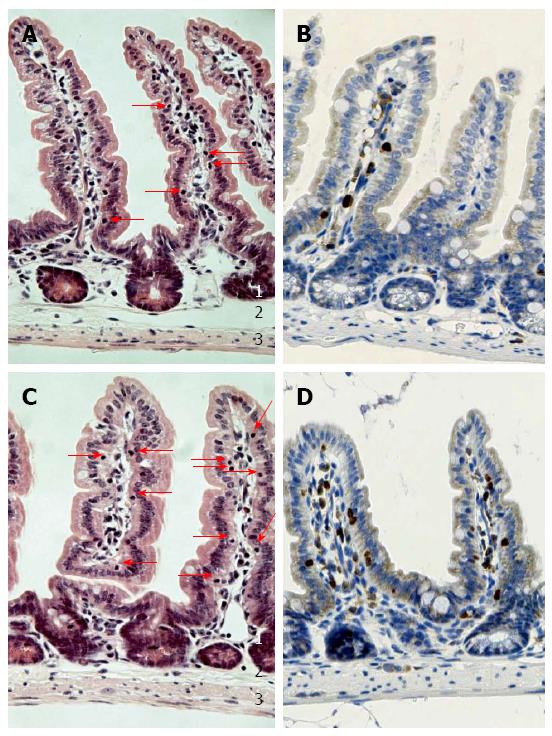
Using HE-stained tissue sections, small intestinal histomorphology of beta-7 integrin-deficient mice and wild types littermates was compared. In both groups, the basal tissue architecture was preserved throughout the small intestine (duodenum, jejunum, and ileum) including mucosa, submucosa, muscularis propria, and serosa. However, the number of IELs was significantly reduced in all small intestinal segments of beta-7 integrin-deficient mice when compared to controls (Figure 1). In addition, the Peyer’s patches of beta-7 integrin-deficient mice appeared hypoplastic. These findings were in high accordance with the original description of an injured GALT in beta-7 integrin-deficient mice[15].
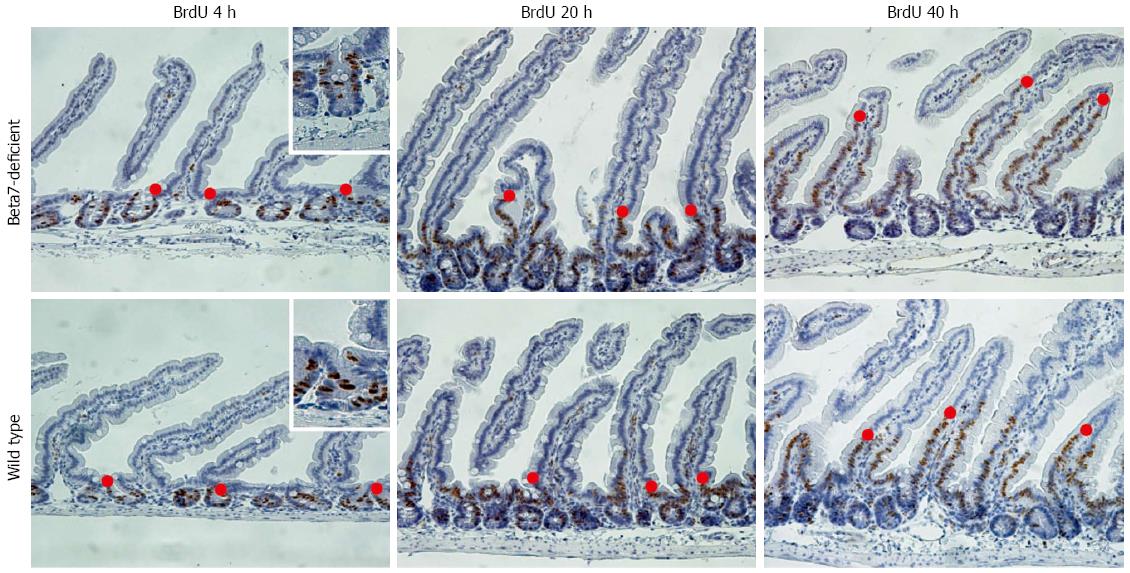
To evaluate migration of small intestinal enterocytes in vivo we used the BrdU-assay established by Potten et al[1,2]. Beta-7 integrin-deficient mice and controls were sacrificed 4, 20 or 40 h after BrdU application. Location of cellmax along the CVA was morphometrically evaluated in 50 hemi-crypts throughout the small intestine of each animal (about 15 hemi-crypts per duodenum, jejunum, and ileum) (Figure 2).
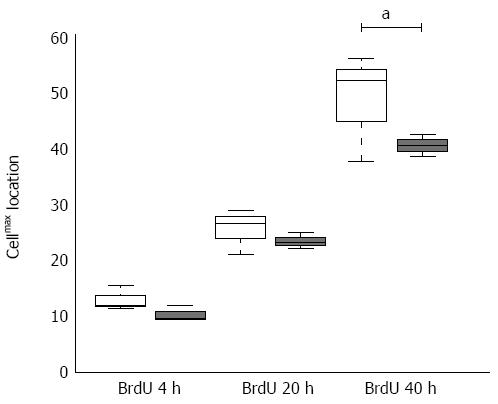
In the small intestinal mucosa of beta-7 integrin-deficient mice, the location of cellmax was found in a significantly higher position than it was the case for the controls (Figure 3). The difference was already detected at 4 h after BrdU application, but significantly increased with time (40 h after BrdU injection; P-value < 0.05). The differences observed were identical in all small intestinal segments investigated, i.e., duodenum, jejunum, and ileum.
Cellular migration is a fundamental phenomenon which is determined by a plethora of molecules and regulated by diverse molecular pathways[10]. In the intestine, migration of epithelial and non-epithelial cells is essential for integrity as well as maintenance of the intestinal mucosal barrier and important to establish intestinal immunity[19-21].
Integrins are important players in establishment of cellular migration[8,13]. Integrins containing the beta-7 subunit are exclusively expressed on leukocytes and important for cell trafficking as well as homing and retention of lymphocytes into the intestinal mucosa[13,15,22]. It has been shown that beta-7 integrins bind MAdCAM-1, which is found on endothelial cells in small venules, and E-cadherin, which is strongly expressed by enterocytes[23].
In the present study we evaluated the influence of a loss of beta-7 integrin, which is essential for homing and retention of lymphocytes within the mucosal epithelial layer, on the continuous migration of enterocytes. The study was focussed on the small intestine where configuration of the GALT is more essential than in the colorectum.
Our study gives evidence that both establishment of the GALT and enterocyte migration are affected in the small intestinal mucosa of beta-7 integrin-deficient mice. The finding that these animals display diminished numbers of IELs is in line with several previous studies[13,15,23]. The finding that the injured configuration of IELs in the mucosa of beta-7 integrin knockout mice is additionally associated with a significant increase in enterocyte migration, which is likely secondary to the lymphocyte homing defect, is new.
In view with the literature, the E-cadherin beta-7 integrin pathway could be a molecular basis for an increased enterocyte migration in beta-7 integrin knockout mice[23]. Binding of lymphocytes to epithelial cells is strongly mediated by a molecular link between alphaE beta-7 integrin and E-cadherin[16]. In addition, E-cadherin - the major constituent of adherens junctions - is preferentially involved in the configuration of apical junctional complexes and a major prerequisite for cell as well as tissue polarization. Ultra-structurally, E-cadherin binds intracellular to catenins (e.g., beta-catenin, p120, and plakoglobin) which link E-cadherin activities to the actin cytoskeleton[24]. Disturbed E-cadherin function has been linked to diverse pathological processes and diseases involving an injured intestinal homeostasis and barrier function[25,26].
A crucial role of E-cadherin in migration of enterocytes was recently shown[27]. Using the BrdU technique they demonstrated that loss of E-cadherin was associated with a significant increase in cell migration and development of cell death. In view with these data, epithelial cell migration within the intestinal mucosa is probably modified by several mechanisms including the composition of epithelial and non-epithelial cell types and the integrity of E-cadherin/adherens junctions. In a putative dynamic model, epithelial migration at the intestinal surface is probably lower in heterologue systems (epithelium with normal or increased IELs; e.g., wild type mice) than in homologue systems (epithelium without or low IELs; e.g., beta-7 integrin knockout mice) or adherens junction-defect systems (loss of E-cadherin/catenins; e.g., conditionally inactivated Cdh1 gene in intestinal epithelia). This point of view is further substantiated by the observation that with an increasing content of goblet cells within the surface epithelial layer (heterologue system) enterocyte migration diminishes from the small intestine (turnover time 48.3 h) to colon (83.5 h) and rectum (101.2 h)[2]. The present study does not rule out the possibility that other molecular mechanisms than a disturbed beta-7 integrin-mediated enterocyte - lymphocyte communication exists determining the migration defects. However, further studies are necessary to investigate the impact of cellular composition within the intestinal epithelial layer to enterocyte migration and its putative role in pathophysiological circumstances including inflammatory and non-inflammatory intestinal disorders.
In conclusion, our study demonstrates that beta-7 integrin is not only involved in regulating homing and retention of lymphocytes but also in regulating migration of enterocytes within the small intestine surface lining epithelium.
Beta-7 integrins determine the migration of lymphocytes into the lamina propria and facilitate formation of the gut-associated lymphoid tissue. AlphaE beta-7 integrin mediates the retention of lymphocytes in the gut epithelium via E-cadherin. The intercellular protein is strongly synthesized by enterocytes.
A significant reduction of intra-epithelial lymphocytes, lamina propria lymphocytes, hypoplasia of Peyer’s patches, and a reduced number of IgA- and IgM-producing cells are found in the small intestine of beta-7 integrin-deficient mice. In this study, the authors demonstrate that beta-7 integrin deficiency probably affects enterocyte migration.
Recent reports have highlighted the importance of beta-7 integrins in configuration the gut-associated lymphoid tissue and lymphocyte migration. This is the first study demonstrating that beta-7 integrin deficiency is associated with a disturbed enterocyte migration. Loss of beta-7 integrin accelerates enterocyte migration along the crypt-villus axis probably mediated via the E-cadherin beta-7 integrin pathway.
The observation that beta-7 integrin affects enterocyte migration could be crucial for the better understanding how immunological mechanisms modulate intestinal barrier configuration.
Integrins are proteins involved in cell-cell as well as cell-matrix cross talks. They are found in several classes and isoforms. Beta-7 integrins are exclusively expressed on leukocytes and important for cell trafficking as well as homing and retention of lymphocytes.
In this study, the authors attempt to demonstrate that beta-7 integrin controls enterocyte migration within the small intestinal surface lining epithelial layer. They have used beta-7 integrin deficient mice for this study.
P- Reviewer: Nihalani D, Yang PC S- Editor: Gou SX L- Editor: A E- Editor: Zhang DN
| 1. | Potten CS, Loeffler M. Stem cells: attributes, cycles, spirals, pitfalls and uncertainties. Lessons for and from the crypt. Development. 1990;110:1001-1020. [PubMed] |
| 2. | Potten CS, Kellett M, Roberts SA, Rew DA, Wilson GD. Measurement of in vivo proliferation in human colorectal mucosa using bromodeoxyuridine. Gut. 1992;33:71-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 149] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 3. | Stange DE, Clevers H. Concise review: the yin and yang of intestinal (cancer) stem cells and their progenitors. Stem Cells. 2013;31:2287-2295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 4. | Becker C, Watson AJ, Neurath MF. Complex roles of caspases in the pathogenesis of inflammatory bowel disease. Gastroenterology. 2013;144:283-293. [PubMed] |
| 5. | Kernéis S, Bogdanova A, Kraehenbuhl JP, Pringault E. Conversion by Peyer’s patch lymphocytes of human enterocytes into M cells that transport bacteria. Science. 1997;277:949-952. [PubMed] |
| 6. | Corr SC, Gahan CC, Hill C. M-cells: origin, morphology and role in mucosal immunity and microbial pathogenesis. FEMS Immunol Med Microbiol. 2008;52:2-12. [PubMed] |
| 7. | Friedl P, Wolf K. Plasticity of cell migration: a multiscale tuning model. J Cell Biol. 2010;188:11-19. [PubMed] |
| 8. | Huttenlocher A, Horwitz AR. Integrins in cell migration. Cold Spring Harb Perspect Biol. 2011;3:a005074. [PubMed] |
| 10. | Vicente-Manzanares M, Webb DJ, Horwitz AR. Cell migration at a glance. J Cell Sci. 2005;118:4917-4919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 283] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 11. | Kölsch V, Charest PG, Firtel RA. The regulation of cell motility and chemotaxis by phospholipid signaling. J Cell Sci. 2008;121:551-559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 293] [Cited by in RCA: 284] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 12. | Cain RJ, Ridley AJ. Phosphoinositide 3-kinases in cell migration. Biol Cell. 2009;101:13-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 176] [Cited by in RCA: 196] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 13. | Luo BH, Carman CV, Springer TA. Structural basis of integrin regulation and signaling. Annu Rev Immunol. 2007;25:619-647. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1327] [Cited by in RCA: 1229] [Article Influence: 68.3] [Reference Citation Analysis (0)] |
| 14. | Bouchard V, Harnois C, Demers MJ, Thibodeau S, Laquerre V, Gauthier R, Vézina A, Noël D, Fujita N, Tsuruo T. B1 integrin/Fak/Src signaling in intestinal epithelial crypt cell survival: integration of complex regulatory mechanisms. Apoptosis. 2008;13:531-542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 65] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 15. | Wagner N, Löhler J, Kunkel EJ, Ley K, Leung E, Krissansen G, Rajewsky K, Müller W. Critical role for beta7 integrins in formation of the gut-associated lymphoid tissue. Nature. 1996;382:366-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 434] [Cited by in RCA: 433] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 16. | Cepek KL, Shaw SK, Parker CM, Russell GJ, Morrow JS, Rimm DL, Brenner MB. Adhesion between epithelial cells and T lymphocytes mediated by E-cadherin and the alpha E beta 7 integrin. Nature. 1994;372:190-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 875] [Cited by in RCA: 887] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 17. | Schön MP, Schön M, Warren HB, Donohue JP, Parker CM. Cutaneous inflammatory disorder in integrin alphaE (CD103)-deficient mice. J Immunol. 2000;165:6583-6589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Trbojević-Stanković JB, Milićević NM, Milosević DP, Despotović N, Davidović M, Erceg P, Bojić B, Bojić D, Svorcan P, Protić M. Morphometric study of healthy jejunal and ileal mucosa in adult and aged subjects. Histol Histopathol. 2010;25:153-158. [PubMed] |
| 19. | Bibiloni R, Schiffrin EJ. Intestinal Host-Microbe Interactions under Physiological and Pathological Conditions. Int J Inflam. 2010;2010:386956. [PubMed] |
| 20. | Ivanov AI, Parkos CA, Nusrat A. Cytoskeletal regulation of epithelial barrier function during inflammation. Am J Pathol. 2010;177:512-524. [PubMed] |
| 21. | Arciero JC, Mi Q, Branca MF, Hackam DJ, Swigon D. Continuum model of collective cell migration in wound healing and colony expansion. Biophys J. 2011;100:535-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 81] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 22. | Agace WW, Higgins JM, Sadasivan B, Brenner MB, Parker CM. T-lymphocyte-epithelial-cell interactions: integrin alpha(E) CD103)beta(7), LEEP-CAM and chemokines. Curr Opin Cell Biol. 2000;12:563-568. [PubMed] |
| 23. | Gorfu G, Rivera-Nieves J, Ley K. Role of beta7 integrins in intestinal lymphocyte homing and retention. Curr Mol Med. 2009;9:836-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 216] [Cited by in RCA: 244] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 24. | Halbleib JM, Nelson WJ. Cadherins in development: cell adhesion, sorting, and tissue morphogenesis. Genes Dev. 2006;20:3199-3214. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 760] [Cited by in RCA: 762] [Article Influence: 42.3] [Reference Citation Analysis (0)] |
| 25. | Gassler N, Rohr C, Schneider A, Kartenbeck J, Bach A, Obermüller N, Otto HF, Autschbach F. Inflammatory bowel disease is associated with changes of enterocytic junctions. Am J Physiol Gastrointest Liver Physiol. 2001;281:G216-G228. [PubMed] |
| 26. | Schulzke JD, Ploeger S, Amasheh M, Fromm A, Zeissig S, Troeger H, Richter J, Bojarski C, Schumann M, Fromm M. Epithelial tight junctions in intestinal inflammation. Ann N Y Acad Sci. 2009;1165:294-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 299] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 27. | Schneider MR, Dahlhoff M, Horst D, Hirschi B, Trülzsch K, Müller-Höcker J, Vogelmann R, Allgäuer M, Gerhard M, Steininger S. A key role for E-cadherin in intestinal homeostasis and Paneth cell maturation. PLoS One. 2010;5:e14325. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 130] [Cited by in RCA: 154] [Article Influence: 10.3] [Reference Citation Analysis (0)] |