Published online Dec 28, 2015. doi: 10.3748/wjg.v21.i48.13587
Peer-review started: April 16, 2015
First decision: June 19, 2015
Revised: June 25, 2015
Accepted: August 30, 2015
Article in press: August 31, 2015
Published online: December 28, 2015
Processing time: 253 Days and 10 Hours
This paper reports our experience with a new over-the-scope clip in the setting of recurrent bleeding and oesophageal fistula. We treated five patients with the over-the-scope Padlock Clip™. It is a nitinol ring, with six inner needles preassembled on an applicator cap, thumb press displaced by the Lock-It™ delivery system. The trigger wire is located alongside the shaft of the endoscope, and does not require the working channel. Three patients had recurrent bleeding lesions (bleeding rectal ulcer, post polypectomy delayed bleeding and duodenal Dieulafoy’s lesion) and two patients had a persistent respiratory-esophageal fistula. In all patients a previous endoscopic attempt with standard techniques had been useless. All procedures were conducted under conscious sedation but for one patient that required general anaesthesia due to multiple comorbidities. We used one Padlock Clip™ for each patient in a single session. Simple suction was enough in all of our patients to obtain tissue adhesion to the instrument tip. A remarkably short application time was recorded for all cases (mean duration of the procedure: 8 min). We obtained technical and immediate clinical success for every patient. No major immediate, early or late (within 24 h, 7 d or 4 wk) adverse events were observed, over follow-up durations lasting a mean of 109.4 d. One patient, treated for duodenal bulb bleeding from a Dieulafoy's lesion, developed signs of mild pancreatitis 24 h after the procedure. The new over-the-scope Padlock Clip™ seems to be simple to use and effective in different clinical settings, particularly in “difficult” scenarios, like recurrent bleeding and respiratory-oesophageal fistulas.
Core tip: We report our experience with the novel over-the-scope Padlock Clip™, applied in five patients in the clinical settings of oesophageal fistulas and refractory gastrointestinal bleeding. The Padlock ClipTM has shown reliable closure of wall defects in a porcine survival study, although clinical usage remains limited. As yet, there are no published data regarding its application in the management of non-variceal gastrointestinal bleeding. We provide a comprehensive iconographic documentation and two videos showing its application. We also accurately describe the device and its release system, pointing out the differences with the well-known over-the-scope clip system.
- Citation: Armellini E, Crinò SF, Orsello M, Ballarè M, Tari R, Saettone S, Montino F, Occhipinti P. Novel endoscopic over-the-scope clip system. World J Gastroenterol 2015; 21(48): 13587-13592
- URL: https://www.wjgnet.com/1007-9327/full/v21/i48/13587.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i48.13587
Given improvements in therapeutic endoscopy techniques and devices, endoscopists are being confronted with clinical complex situations such as perforations, anastomotic leakage and fistulas.
The incidence of perforations in diagnostic endoscopies is approximately 0.03%, with a mortality rate of up to 17% and a morbidity rate of up to 40%[1]; when interventional procedures are included, the incidence of perforations increases to 5%[2]. It is well known that a surgical approach to perforations, as well as to respiratory-esophageal fistulas, has relevant morbidity and mortality. This is the reason that prompted endoscopists to deal with such conditions[3].
Another complex and demanding condition is non-variceal gastrointestinal bleeding (NVGIB), which cannot be managed using conventional endoscopic therapies. Deeply penetrating fibrotic ulcers are an example of such a condition. Despite adequate initial endoscopic therapy, recurrent upper gastrointestinal (GI) bleeding can occur in up to 24% of high-risk patients[4]. Surgery or selective radiological embolization may represent the salvage therapeutic option, but surgical management in such patients is often difficult, time-consuming and related to non-negligible levels of morbidity and mortality[5].
In past years, an over-the-scope clip system (OTSC, Ovesco Endoscopy AG, Tubingen, Germany) has been tested in large studies for closing GI defects[6] and in smaller studies for refractory bleeding[7], so its clinical efficacy has been established. Recently a new OTS clip (Padlock Clip™, Aponos Medical, Kingston, NH, United States) has been developed and tested in porcine models for closing wall defects[8,9]. As of yet, data regarding its application in clinical practise are lacking.
The aim of this series is to describe our experience with the novel OTS Padlock Clip™.
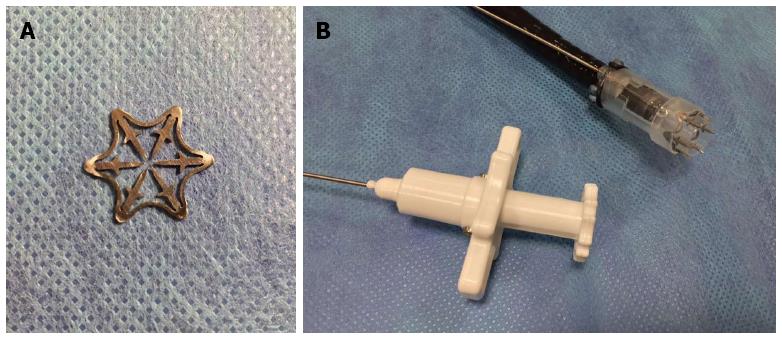
The Padlock Clip™ is a nitinol ring, with six inner needles preassembled on an applicator cap (available for 9.5-11 mm scope tips), thumb press displaced by the Lock-It™ delivery system (Aponos Medical, Kingston, NH, United States). The trigger wire is located alongside the shaft of the endoscope, and does not require the working channel (Figure 1, Video 1).
This design allows for more efficient suction that is sufficient to ensure tissue adhesion to the instrument tip into the cap, not requiring other instruments. Moreover, the suction of blood and secretions is always ensured.
When the clip is deployed, it instantly springs back to its original form, an 11 mm hexagonal ring, and gathers, folds and compresses the tissue. Proprietary radial compression technology provides even 360° tissue compression. Precise tissue controllers limit penetration and moderate tissue-on-tissue pressure. Effective tissue closure is obtained that is resistant to GI pressures, while still maintaining blood flow to promote healing.
In this series, we included all of the patients treated using the new Padlock Clip™ between October 2014 and December 2014. An overview of the patient demographic data, etiology, clinical condition, comorbidities and previous treatment attempts is listed in Table 1.
| No. | Age, yr | Etiology | Clinical condition | Comorbidities | Previous treatment |
| 1 | 61 | Endoscopic mucosal resection | Delayed rectal bleeding | Hypertension, HF, RF | Endoclip, injective therapy |
| 2 | 80 | Solitary rectal ulcer | Rectal bleeding | Hypertension | Endoclip, injective therapy |
| 3 | 85 | Duodenal Dieulafoy lesion | Duodenal bleeding | Hypertension, prosthetic aortic valve, HF | Injective and thermal therapy |
| 4 | 53 | Mediastinal lymphoma | Broncho-esophageal fistula | None | Endoclip |
| 5 | 66 | Post-laringectomy radio-chemoteraphy | Tracheo-esophageal fistula | COPD, HIV+, hypertension, HF | Endoclip, salivary stent |
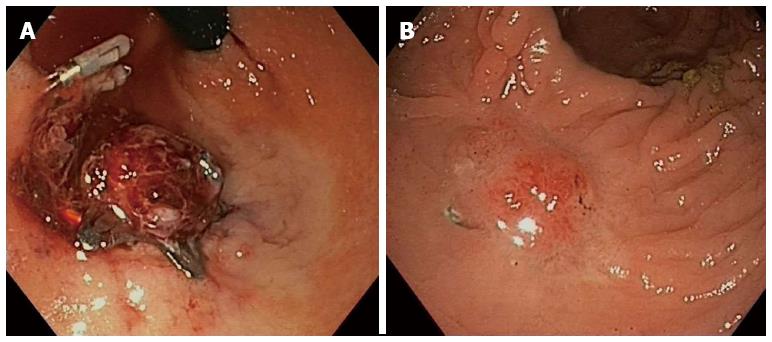
A 61-year-old patient with multiple comorbidities underwent a colonoscopy for positive faecal blood; a large laterally spreading tumor in the rectum was diagnosed and removed by piecemeal endoscopic mucosal resection (EMR). One week later, massive rectal bleeding and hypotension occurred. After an unsuccessful conventional endoscopic hemostasis (adrenaline injection plus endoscopic clipping), we decided to apply the Padlock Clip™ to obtain immediate control of the bleeding (Video 2). Clip retention was documented during the three-month endoscopic control (Figure 2) without clinical consequences.
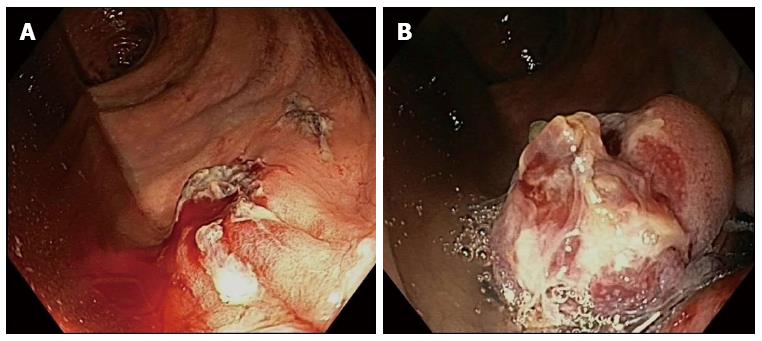
A solitary rectal ulcer showing overt bleeding was diagnosed in an 80-year-old male with hemorrhagic shock. Due to the large, deeply penetrating hard base of the ulcer, we considered that using a conventional through-the-scope clip would likely be unsuccessful. Injective and thermal devices were insufficient for controlling bleeding and, therefore, a Padlock Clip™ was deployed obtaining durable hemostasis (Figure 3).
The patient was referred for shock due to massive gastrointestinal bleeding on the third day after major cardiac surgery for prosthetic thoracic aorta replacement. An inferior duodenal bulb wall Dieulafoy lesion was treated with adrenalin injection and argon plasma coagulator. Twenty four hours later, massive rebleeding occurred and was successfully controlled by a Padlock Clip™.
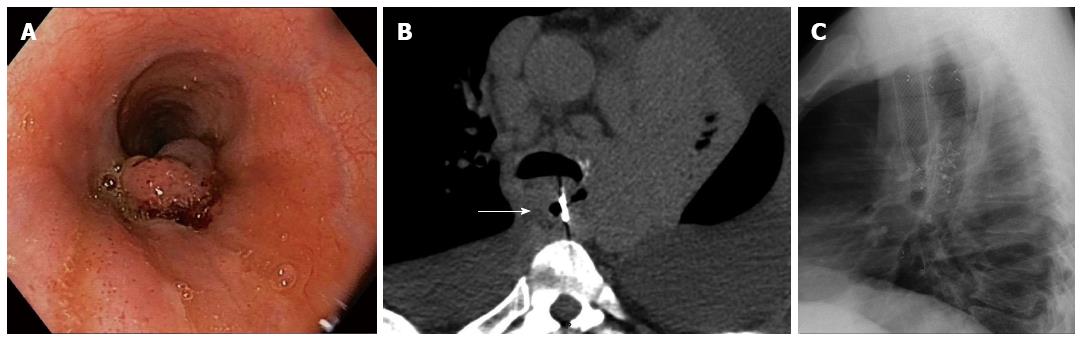
A 53-year-old male exhibiting recent onset of a cough and fever underwent a thoracic and abdominal computed tomography (CT) scan that revealed a bulky mediastinal lymphoma complicated by a broncho-esophageal fistula. An upper endoscopy was performed and after a failed attempt with traditional clipping, the absence of esophageal stenosis and the adequate accessibility of the esophageal edge prompted us to use the Padlock Clip™ system (Video 3). A tracheal prosthesis was then placed. One month later, persisting the bulky lymphoma, two new fistula tracts developed proximally and distally to the first one; we accordingly implanted a fully covered, self-expandable metal stent (Figure 4). No clip retention was documented during follow-up.
A 65-year-old male received a laryngectomy, followed by radio-chemotherapy for laryngeal cancer. He was re-admitted to our hospital because of recurrent bronchitis and cough. A diagnosis of a tracheoesophageal fistula was achieved. After several therapies failed, we successfully used the Padlock Clip™ at the esophageal edge of the fistula.
All patients were male with a mean age of 69 years. Conscious sedation was used for four out of the five patients; one (case 3) required general anaesthesia due to multiple comorbidities. All patients had already been treated with standard endoscopic techniques, which had failed. We used one Padlock Clip™ for each patient in a single session. Simple suction was enough in all of our patients to obtain tissue adhesion to the instrument tip. A remarkably short application time was recorded for all cases (mean duration of the procedure: 8 min). We obtained technical and immediate clinical success for every patient (Table 2). Bleeding control was persistent. No rescue therapies, surgeries or interventional radiologies were necessary. The fistulous tract was closed in both of our patients. However, in patient number 4, we observed two new broncho-esophageal fistulas after one month due to the persistence of the mediastinal colliquated nodes. It is worth noting that the recurrences occurred in close proximity, below and on top of the first opening of the fistula, which showed the persistence of the fully deployed Padlock Clip™. Therefore, we decided to place an esophageal fully covered, self-expandable metal stent. No major immediate, early or late (within 24 h, 7 d or 4 wk) adverse events were observed, over follow-up durations lasting a mean of 109.4 d. Patient number 3, treated for duodenal bulb bleeding from a Dieulafoy lesion, developed signs of mild pancreatitis 24 h after the procedure. An abdominal CT-scan did not show transmural penetration of the clip.
| No. | Technical success | Operation time (min) | Treatment outcome | Salvage procedure (surgery, interventional radiology) | Adverse events/morbidity | Follow up (d) |
| 1 | Yes | 11 | Persistent control of the bleeding | No | None | 102 |
| 2 | Yes | 6 | Persistent control of the bleeding | No | None | 142 |
| 3 | Yes | 7 | Persistent control of the bleeding | No | Mild pancreatitis | 90 |
| 4 | Yes | 6 | New fistulas development | No | None | 60 |
| 5 | Yes | 8 | Fistula healing | No | None | 153 |
In the case of rectal post-polypectomy delayed bleeding, the 3-mo endoscopic control revealed a mucosal proliferation hiding the Padlock Clip™. A biopsy of the redundant tissue was performed and revealed a foreign body granuloma (Figure 2).
The increasing number of gastrointestinal endoscopic examinations and more advanced operative techniques, including EMR and endoscopic submucosal dissection (largely applied in the field of oncology) has yielded a larger number of adverse events. Perforation during upper and lower GI endoscopies is relatively rare, but its occurrence is associated with significant morbidity and potential mortality for the affected patient.
Furthermore, given recent advancements in equipment, the role of therapeutic endoscopies in dealing with complex clinical conditions, such as GI perforations and acquired fistulas, is being increasingly tested on an every-day basis.
In terms of GI bleeding, mechanical hemostatic methods have been shown to achieve a higher rate of permanent hemostasis than injections or thermal methods alone[10] and endoclips have been increasingly adopted. Unfortunately, the rebleeding rate after endoclipping ranges from 7% to 10%. The application of a standard through-the-scope clip on a large fibrotic ulcer base is often technically difficult or impossible. The OTSC clip has advantages of a larger jaw width and a greater strength[7].
To date, the most commonly used over-the-scope system is the OTSC, which has already been tested in large series for closure of GI defects[6] and in a smaller series for refractory bleeding. It has demonstrated good technical and clinical success due to its stronger closure than regular through-the-scope clips, due to its wider mouth and ability to grip larger amounts of tissue. The OTSC is associated with only a few adverse events[7].
In our series, we used the new Padlock over-the-scope system in three patients with refractory GI bleeding and two patients affected by esophageal fistulas, according to the indications already tested in large series for the OTSC. Although the working mechanism of the systems are similar, these two systems differ in some relevant details. Both are made of nitinol and do not preclude magnetic resonance imaging. However, the OTSC “bear claw” design differs from the round-hexagonal Padlock Clip™. Both are preloaded on an applicator cap. The OTSC is available in three diameters (11, 12, and 14 mm), two working depths (3 and 6 mm) and three types of teeth (atraumatic, traumatic and gastrostomy closure). On the other hand, the Padlock Clip™ is produced as a single model. Another important difference is in the delivery system. The OTSC deployment, similar to a band ligator, is achieved by triggering a string wire connected to a rotating hand wheel that is fastened to the entrance port of the working channel.
Invaginating the tissue inside the cap is obtained by suction alone or by the additional use of the OTSC Twin Grasper or the OTSC Anchor (both Ovesco Endoscopy AG), inserted through the operative channel. While the string wire alone does not hamper the suction trough the operative channel, this may be hampered by such additional devices.
The novel Padlock Clip™ is displaced with a thumb press using the Lock-It™ delivery system, which is located parallel to the endoscope, and does not require the working channel at all (Figure 1). No tissue grasper device is available for this over-the-scope clip.
The target tissue is invaginated inside the cap by simple suction, which allows also for continuous removal of blood and secretions.
The push-button system is not connected to the scope and the possibility of easy release by a nurse is necessary, but it prevents the endoscopists from having to remove their hands from the scope.
Up to now the novel Padlock Clip™ has been tested in survival porcine models for the closure of wall defects[8,9].
We used the Padlock Clip™ for the management of clinical conditions that have been largely tested to date with the OTSC: refractory NVGIB and GI wall defects. Standard endoscopic therapy was attempted in all of our cases; no major adverse events have been observed.
The OTSC remains attached longer than through-the-scope clips, likely due to its attachment to the submucosa and muscularis propria. In a recent series, the mean retention time of the OTSC was 28 d (range: 0-42 d)[11]. In a larger retrospective study of the OTSC system, clip retention occurred in approximately 2/3 of patients[12].
We documented Padlock Clip™ retention for three months in patient number 1 and for one month in patient number 4. We did not determine the mean retention time in the other patients.
In patient number 3, we used the Padlock Clip™ on a Dieulafoy lesion of the duodenum with technical and clinical success at stopping the bleeding. However, 24 h later, we observed the onset of mild pancreatitis, which was resolved with medical therapy. The connection between this event and the application of the clip is not clear in a critically ill patient, although the strict time relationship may suggest a cause-effect relation; deep transmural penetration of the clip was excluded by an abdominal CT-scan.
Described cases, while confirming a role for the OTS systems in operative endoscopy (compression of large tissue areas, non-variceal bleedings difficult to control and lesions or perforations of the GI tract), show the Padlock Clip™ to be safe and efficient, with a short application time.
Particularly it has been effective in "difficult" clinical settings like recurrent bleeding and respiratory-oesophageal fistulas. Although other studies are needed, in our experience the new over-the-scope Padlock Clip™ seems to be simple to use and effective. This system may represent a new and alternative therapeutic option for the management of different clinical scenarios.
Three patients presented with overt gastrointestinal bleeding (one upper and two lower) and two patients presented with dysphagia and cough.
Bleeding patients had hypotension and hemorrhagic shock; fistula patients had pathologic thoracic physical examination.
Other causes of upper and lower gastrointestinal bleeding (peptic ulcer, variceal bleeding, diverticulas); mediastinal malignancy, esophageal cancer.
Severe anaemia in three patients affected by refractory bleeding and elevated white cells count and C-reactive protein in patients affected by respiratory-esophageal fistulas.
For fistula patients, thoracic computed tomography-scan and X-ray confirmed the fistulous tract.
The authors treated all patients using the Padlock Clip™.
Endoscopic over-the-scope clips (OTS) systems have showed good performance in the treatment of recurrent bleeding and oesophageal fistulas. Few experience with the new over-the-scope Padlock Clip™ are reported.
OTS are endoscopic devices loaded on the tip of the scope and not passed through the scope as for traditional endoscopic clips.
OTS is effective in different clinical settings, particularly in “difficult” scenarios like recurrent bleeding and respiratory-oesophageal fistulas.
The study reports initial experiences with the new OTS Padlock Clip™ system, with comprehensive documentation supported by videos.
P- Reviewer: Kopacova M, Lakatos PL, Thomopoulos KC S- Editor: Ma YJ L- Editor: Filipodia E- Editor: Ma S
| 1. | Merchea A, Cullinane DC, Sawyer MD, Iqbal CW, Baron TH, Wigle D, Sarr MG, Zielinski MD. Esophagogastroduodenoscopy-associated gastrointestinal perforations: a single-center experience. Surgery. 2010;148:876-880; discussion 881-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 68] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 2. | Oda I, Suzuki H, Nonaka S, Yoshinaga S. Complications of gastric endoscopic submucosal dissection. Dig Endosc. 2013;25 Suppl 1:71-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 163] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 3. | Reed MF, Mathisen DJ. Tracheoesophageal fistula. Chest Surg Clin N Am. 2003;13:271-289. [PubMed] |
| 4. | Hwang JH, Fisher DA, Ben-Menachem T, Chandrasekhara V, Chathadi K, Decker GA, Early DS, Evans JA, Fanelli RD, Foley K. The role of endoscopy in the management of acute non-variceal upper GI bleeding. Gastrointest Endosc. 2012;75:1132-1138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 232] [Cited by in RCA: 218] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 5. | Wong TC, Wong KT, Chiu PW, Teoh AY, Yu SC, Au KW, Lau JY. A comparison of angiographic embolization with surgery after failed endoscopic hemostasis to bleeding peptic ulcers. Gastrointest Endosc. 2011;73:900-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 78] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Haito-Chavez Y, Law JK, Kratt T, Arezzo A, Verra M, Morino M, Sharaiha RZ, Poley JW, Kahaleh M, Thompson CC. International multicenter experience with an over-the-scope clipping device for endoscopic management of GI defects (with video). Gastrointest Endosc. 2014;80:610-622. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 207] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 7. | Manta R, Galloro G, Mangiavillano B, Conigliaro R, Pasquale L, Arezzo A, Masci E, Bassotti G, Frazzoni M. Over-the-scope clip (OTSC) represents an effective endoscopic treatment for acute GI bleeding after failure of conventional techniques. Surg Endosc. 2013;27:3162-3164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 77] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 8. | Desilets DJ, Romanelli JR, Earle DB, Chapman CN. Gastrotomy closure with the lock-it system and the Padlock-G clip: a survival study in a porcine model. J Laparoendosc Adv Surg Tech A. 2010;20:671-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Guarner-Argente C, Córdova H, Martínez-Pallí G, Navarro R, Cuatrecasas M, Rodríguez de Miguel C, Beltrán M, Lacy AM, Ginès A, Pellisé M. Yes, we can: reliable colonic closure with the Padlock-G clip in a survival porcine study (with video). Gastrointest Endosc. 2010;72:841-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Sung JJ, Tsoi KK, Lai LH, Wu JC, Lau JY. Endoscopic clipping versus injection and thermo-coagulation in the treatment of non-variceal upper gastrointestinal bleeding: a meta-analysis. Gut. 2007;56:1364-1373. [PubMed] |
| 11. | Chan SM, Chiu PW, Teoh AY, Lau JY. Use of the Over-The-Scope Clip for treatment of refractory upper gastrointestinal bleeding: a case series. Endoscopy. 2014;46:428-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 12. | Law R, Irani S, Wong Kee Song LM, Baron TH. Clip Retention Following Endoscopic Placement of the Over-the-Scope Clip (OTSC). Gastrointest Endosc. 2013;77 Supplement:AB221-AB222. |