Published online Dec 28, 2015. doi: 10.3748/wjg.v21.i48.13582
Peer-review started: May 7, 2015
First decision: July 19, 2015
Revised: July 24, 2015
Accepted: October 12, 2015
Article in press: October 13, 2015
Published online: December 28, 2015
Processing time: 238 Days and 5.4 Hours
Graves’ disease is an autoimmune disease, which can manifest with a variety of extrathyroidal clinical syndromes like ophthalmopathy, pretibial myxedema (dermopathy), acropathy, cardiomyopathy, and encephalopathy. Though quite rare, this disease can also manifest with gastrointestinal symptoms such as dysphagia, heartburn, nausea, vomiting and diarrhea. We report a clinical case of Graves’ disease manifesting with dysfunction of the esophagus and heartburn in a 61-year-old man. In the muscular layer of the esophagus we found dystrophic changes led to its atony, which was documented by endoscopy and high-resolution manometry. The pathology features of esophageal symptoms were: focal proliferation of the basal cells, vascular distension, and dystrophy of the epithelial cells. Antithyroid treatment led to decrease of all clinical symptoms after 5 d of Thiamazole administration. Complete restoration of peristalsis in the esophagus, according to manometry, was observed in 1 mo after initiation of treatment.
Core tip: We report a clinical case of Graves’ disease manifesting with dysfunction of the esophagus and heartburn in a 61-year-old man. In the muscular layer of the esophagus we found dystrophic changes led to its atony, which was documented by endoscopy and high-resolution manometry.
- Citation: Evsyutina Y, Trukhmanov A, Ivashkin V, Storonova O, Godjello E. Case report of Graves’ disease manifesting with odynophagia and heartburn. World J Gastroenterol 2015; 21(48): 13582-13586
- URL: https://www.wjgnet.com/1007-9327/full/v21/i48/13582.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i48.13582
Graves’ disease (diffused toxic goiter) is an autoimmune disease which is characterized by the presence of circulating autoantibodies that bind to and stimulate the TSH receptor, which eventually leads to hyperthyroidism and goiter[1]. It’s a rare disease which can manifest with gastrointestinal symptoms like dysphagia, nausea, vomiting and diarrhea[2]. We present a clinical case of Graves’ disease manifesting with odynophagia and heartburn in a 61-year-old man.
A 61-year-old-man was admitted to the Clinic of the First Moscow State Medical University on May 2014 with the following complaints: odynophagia arising on swallowing of both solid and liquid food, severe heartburn, tachycardia, dyspnea, general weakness, and weight loss of 15 kg over the past year.
From the medical history, it was noted that the patient was sick since June 2013, when he first noted the appearance of heartburn, which manifested in 15-20 min after eating and odynophagia, which arose on swallowing solid food. Based on the results of the conducted esophagogastroduodenoscopy (EGD), he was diagnosed with distal esophageal reflux and was prescribed therapy with proton pump inhibitor (PPI) -Omeprazole 20 mg per day and antacids. The prescribed therapy did not produce any positive effect as the patient noted an increase in the severity of the heartburn and odynophagia, which began to worsen further and emerged even while swallowing liquid food. Following a comprehensive survey performed in October 2013, a complete blood analysis was done, all his blood parameters were within normal values, in the general analysis of urine and feces-all indicators were normal too. A re-esophagogastroduodenoscopy was done which revealed distal reflux esophagitis, on basis of which the diagnosis was changed to refractory gastroesophageal reflux disease and the dose of omeprazole was increased to 20 mg 2 times a day. However, the patient's condition progressively worsened-with heartburn and odynophagia the patient also experienced general weakness, tachycardia and dyspnea on exertion. In January 2014 after a re-endoscopy performed on the patient it was decided to change the PPIs from omeprazole to rabeprazole 20 mg 2 times a day and to this was added itopride 50 mg three times a day. This change of therapy did not produce any positive clinical response, the patient noted a strong heartburn after every meal, in addition to the above mentioned symptoms, and the patient also lost 15 kg of weight during the course of the disease.
On admission to the clinic, the general condition of the patient was relatively satisfactory. BMI was 19.6 kg/m2. Skin and visible mucous layers-physiological color and moist. On auscultation, vesicular breathing, no pathologic lung sounds were heard. Cardiac sounds were rhythmic. Pulse 90 beats per minute. BP 130/70 mmHg. Upon abdominal palpation-soft and painless in all areas. Liver could be palpated along the edges of the right costal arch. The thyroid gland was not enlarged, nodules were not palpable. The patient tested positive for symptom Marie (tremor of the fingers of the hand). No edema.
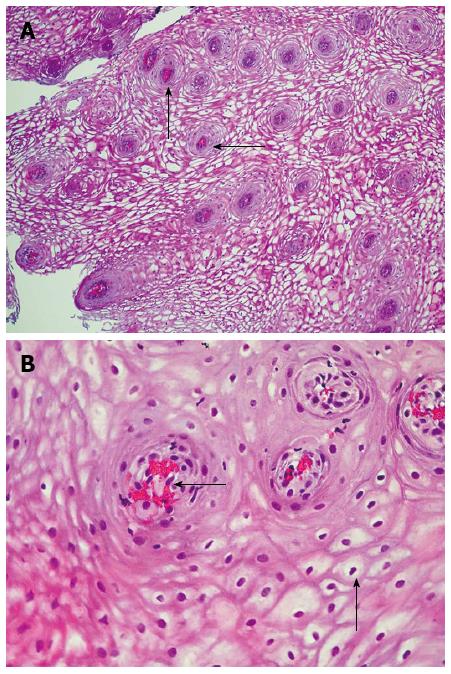
On examination: in complete analysis of blood-hemoglobin 143 g/L, erythrocytes 5.27 × 1012, leukocytes 6.34 × 109, platelets 258 × 109, ESR 10 mm/h. In the biochemical analysis of blood: total protein 76.0 g/L, albumin 47.0 g/L, creatinine 64.0 U/L, glucose 5.9 mmol/L, sodium 145.0 mmol/L, potassium 4.8 mmol/L, calcium 2. 53 mmol/L, total cholesterol 4.9 mmol/L, creatine kinase 50.0 U/L, AST 24.0 U/l, ALT 40.0 U/L, total bilirubin 14.5 U/L, iron 17.63 mmol/L. Overall urine analysis and stool showed no abnormalities. According to the electrocardiogram-sinus tachycardia with a heart rate of 96 beats per minute, intervals PQ 0.18’, QRS 0.08’, QT 0.34’ and normal electrical axis of the heart. Given tachycardia and dyspnea on exertion for a long period of time, the patient underwent echocardiography, the results of which revealed atherosclerosis of the aorta, mitral regurgitation of 1st degree, contractile function of which is satisfactory (ejection fraction 61%, stroke volume 80 mL). According to the results of the endoscopy it was noted that the patient suffered from esophageal dysmotility problem with severe hypotonia of the upper and middle third and segmental spasm in the lower third of the esophagus. Based on the results of the endoscopy and long-term course of the disease a decision was taken to do multiple biopsies of the esophagus. Morphological examination of the biopsy specimens revealed the following changes: Focal proliferation of the basal cells, plethora of vessels and stasis of erythrocytes in the vessels of lamina propria papillae, and dystrophy of the epithelial cells (Figure 1A and B).
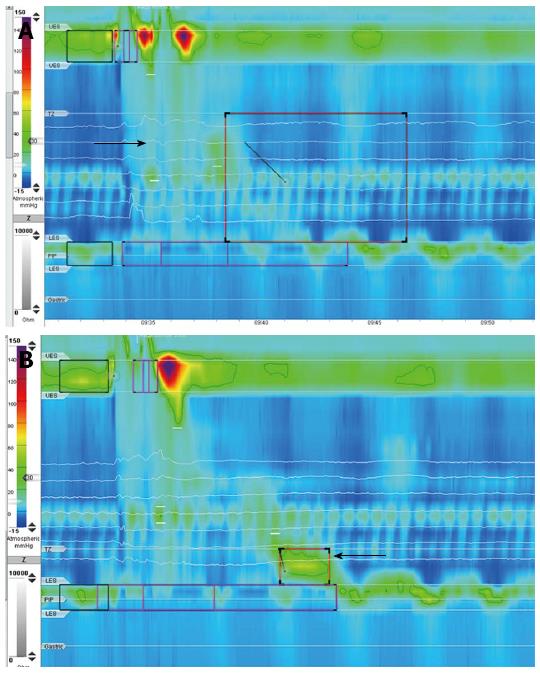
The patient also underwent high-resolution manometry, the results of which: the resting pressure upper esophageal sphincter (UES) 47 mmHg (normal 46-81 mmHg), resting pressure lower esophageal sphincter (LES) 29 mmHg (normal 10-35 mmHg), the opening of the UES and LESs in response to swallowing of water was normal. In thoracic esophageal peristaltic contractions were absent. This marked an increase in the intraesophageal pressure at the time of the passage of the liquid bolus and 1-2 s later in the distal part of the esophagus was registered spastic contraction with low amplitude (19 mmHg) (Figure 2A and B).
Taking into account the patient's complaints: tachycardia, dyspnea, general weakness, weight loss, as well as positive symptom of Marie, the patient’s blood was checked for the levels of the thyroid hormones. The analysis revealed the following changes: thyrotropin-releasing hormone 0.0025 mU/L (normal 0.4-4.0 mU/L), triiodothyronine 14.3 pmol/L (normal 3.5-6.5 pmol/L), thyroxine 39.3 pmol/L (normal 11.5-23.2 pmol/L), antibodies to the TSH receptor 7.6 IU/L (normal 0-1 IU/L), anti-thyroid peroxidase antibodies 39 IU/L (normal 0-30 IU/L). Thus, the patient showed signs of marked thyrotoxicosis. In order clarify the exact causes of thyrotoxicosis an ultrasound of the thyroid gland was done, the results of which showed: enlargement of the thyroid gland, the right lobe 22 mm × 23 mm × 53 mm, left lobe 21 mm × 23 mm × 51 mm isthmus 4.5 mm, thyroid volume 24.6 cm3; the contours of the gland capsule were clear, smooth, and the structure of the parenchyma was heterogeneous with the formation of zones reduced and increased echogenicity. To eliminate the diagnosis of toxic adenoma was done thyroid scintigraphy with 99th Tc-pertechnetate. The intake of radioactive isotope of the thyroid gland were significantly higher than normal (15.1%) (normal 3%-7%), which was of uneven-diffused character; was observed asymmetric distribution of radiopharmaceuticals between the lobes, with some of its predominance in the right lobe; local sources of hypo-and hyperfixation indicator were not detected.
Based on the results of this survey, the patient was diagnosed with 1st degree Graves’ disease of average severity in the stage of decompensation and was prescribed treatment with antithyroid drug Thiamazole 10 mg 3 times a day, and β-blocker Bisoprolol 2.5 mg in the morning. Following the therapy after 5 d, the patient noted a decrease in heartburn and odynophagia, and a complete disappearance of the above mentioned symptoms after a month.
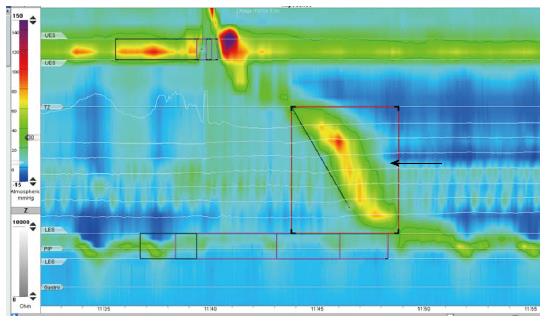
The patient underwent a re-manometry a month later. There was a complete restoration of peristalsis in the thoracic region of the esophagus; he showed no signs of esophageal spasm (Figure 3).
The patient continues to receive antithyroid drug therapy at a dose of 10 mg 3 times a day, on achieving the euthyroidic state, its planned to reduce the daily dose by 5 mg every week to a maintenance dose of 10 mg per day.
Graves’ disease can manifest with a variety of extrathyroidal clinical syndromes like ophthalmopathy, pretibial myxedema (dermopathy), acropathy[3], cardiomyopathy[4], encephalopathy[5]. Though quite rare, this disease can also manifest with gastrointestinal symptoms such as dysphagia, heartburn, nausea, vomiting and diarrhea[2].
The lesion of the esophagus in patients with Graves’ disease may be caused by various reasons. The first being extrinsic enlargement of the thyroid gland, however, for our patient, his thyroid gland was not that enlarged, eliminating the above mentioned mechanism. On the other hand, the excess production of thyroid hormones can lead to the dysfunction of bulbar muscles, which is manifested by symptoms such as dysphagia, dysarthria and dysphonia[6,7]. As for our patient, none of the above mentioned symptoms were present, indicating a completely different mechanism of esophageal complaints.
In the present case, its most likely that there is is a direct effect of excess amount of thyroxine and triiodothyronine on the mitochondria of the muscle cells of the esophagus, leading to the dissociation of oxidative phosphorylation, which in turn causes a disruption of synthesis of the ATP and deenergization tissues[8]. Triiodothyronine and thyroxine are mitochondria-targeting protonophores that can cross the lipid bilayer membrane and transmit the protons through the inner membrane back to the matrix. It leads to loss of electrochemical gradient and cessation of ATP synthesis[8]. Due to the reduction of oxidative phosphorylation dystrophic lesions in esophageal muscles and atonic esophagus were developed.
In this patient dystrophic changes in the muscular layer of the esophagus led to its atony, which was confirmed by endoscopy and manometry, and clinical equivalent of this changes was odynophagia.
Another key symptom of the patient was strongly expressed heartburn. In this case, it could be due to the ineffective esophageal motility-the patient had a complete absence of peristaltic contractions in the thoracic region of the esophagus-resulting in slower bolus clearance (the time required for the esophagus to empty the contents which had entered it by means of primary and secondary peristalsis). The slower bolus clearance is accompanied by a longer delay in the esophageal reflux which creates a pressure high enough for the LES and as a result is clinically accompanied by heartburn.
The histology of esophageal symptoms were degenerative changes in the esophageal mucosa, which were expressed by focal proliferation of the basal cells, plethora of vessels and stasis of erythrocytes in the vessels of lamina propria papillae, and dystrophy of the epithelial cells.
Therefore striking confirmation of the fact that the esophageal symptoms with such a nature of occurrence, had a rapid clinical response to antithyroid drug therapy and there was a complete recovery of the esophageal peristalsis which was confirmed by the results of the esophageal manometry.
In conclusion, it should be noted that Graves’ disease can manifest not only with the thyrotoxic cardiomyopathy, encephalopathy, opthalmopathy, dermopathy and acropathy, but also with thyrotoxic esophagopathy. Odynophagia can be revealed on the thyrotoxic esophagopathy as well as previously described dysphagia and heartburn.
A 61-year-old-man with odynophagia arising on swallowing of both solid and liquid food, severe heartburn, tachycardia, dyspnea, general weakness, and weight loss of 15 kg over the past year.
Graves’ disease, 1st degree of average severity in the stage of decompensation.
Toxic multinodular goiter, Toxic adenoma, Hashimoto Thyroiditis.
The patient showed signs of thyrotoxicosis.
Peristaltic contractions were absent in thoracic esophageal, the intake of radioactive isotope of the thyroid gland were significantly higher than normal.
The focal proliferation of the basal cells, plethora of vessels and stasis of erythrocytes in the vessels of lamina propria papillae, and dystrophy of the epithelial cells.
The antithyroid drug Thiamazole 10 mg 3 times a day, β-blocker Bisoprolol 2.5 mg a day.
Graves’ disease can manifest with a variety of extrathyroidal clinical syndromes. Though quite rare, this disease can also manifest with gastrointestinal symptoms such as dysphagia, heartburn, nausea, vomiting and diarrhea.
Thyrotoxic esophagopathy is a rare extrathyroidal syndrome of Graves’ disease, that can manifests with dysphagia, odynophagia, and heartburn.
Graves’ disease can manifest not only with the thyrotoxic cardiomyopathy, encephalopathy, opthalmopathy, dermopathy and acropathy, but also with thyrotoxic esophagopathy. Odynophagia can be revealed on the thyrotoxic esophagopathy as well as previously described dysphagia and heartburn.
This is a case report about rare clinical manifestations of Graves’ disease. The whole manuscript is simple but interesting, including the consultation process, examination results, and treatment outcome.
P- Reviewer: Bozic MM, Zhang Q S- Editor: Yu J L- Editor: A E- Editor: Zhang DN
| 1. | Menconi F, Marcocci C, Marinò M. Diagnosis and classification of Graves’ disease. Autoimmun Rev. 2014;13:398-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 151] [Article Influence: 13.7] [Reference Citation Analysis (0)] |
| 2. | Carrell S, Trombatore K. Status quo won’t do: the health insurance crisis in Texas. Tex Med. 1991;87:36-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 88] [Article Influence: 5.9] [Reference Citation Analysis (1)] |
| 3. | Bartalena L. Graves’ orbitopathy: imperfect treatments for a rare disease. Eur Thyroid J. 2013;2:259-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Klein I, Danzi S. Thyroid disease and the heart. Circulation. 2007;116:1725-1735. [PubMed] |
| 5. | Utku U, Asil T, Celik Y, Tucer D. Reversible MR angiographic findings in a patient with autoimmune Graves disease. AJNR Am J Neuroradiol. 2004;25:1541-1543. [PubMed] |
| 6. | Parperis K, Dadu R, Hoq S, Argento V. Thyrotoxic Dysphagia in an 82-year-old male. Case Rep Med. 2011;2011:929523. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Kammer GM, Hamilton CR. Acute bulbar muscle dysfunction and hyperthyroidism. A study of four cases and review of the literature. Am J Med. 1974;56:464-470. [PubMed] |
| 8. | Voet D, Voet JG. Biochemistry. 4th ed. Minneapolis: John Wiley and Sons 2011; . |