Published online Oct 14, 2015. doi: 10.3748/wjg.v21.i38.10926
Peer-review started: March 27, 2015
First decision: April 24, 2015
Revised: May 27, 2015
Accepted: August 31, 2015
Article in press: August 31, 2015
Published online: October 14, 2015
Processing time: 202 Days and 11.5 Hours
This report describes a rare case of hilar cholangiocarcinoma with intratumoral calcification that mimicked hepatolithiasis. A 73-year-old man presented to a local hospital with a calcified lesion in the hepatic hilum. At first, hepatolithiasis was diagnosed, and he underwent endoscopic stone extraction via the trans-papillary route. This treatment strategy failed due to biliary stricture. He was referred to our hospital, and further examination suggested the existence of cholangiocarcinoma. He underwent left hepatectomy with caudate lobectomy and extrahepatic bile duct resection. Pathological examination revealed hilar cholangiocarcinoma with intratumoral calcification, while no stones were found. To the best of our knowledge, only one case of calcified hilar cholangiocarcinoma has been previously reported in the literature. Here, we report a rare case of calcified hilar cholangiocarcinoma and reveal its clinicopathologic features.
Core tip: Our report describes an extremely rare case of hilar cholangiocarcinoma with intratumoral calcification. Imaging findings of this case were confusingly similar to those of hepatolithiasis, and it was extremely difficult to make an accurate diagnosis using available radiological findings. We performed pathological examination and observed hilar cholangiocarcinoma with intratumoral calcification. We herein report a rare case of calcified hilar cholangiocarcinoma and reveal its clinicopathologic features.
- Citation: Inoko K, Tsuchikawa T, Noji T, Kurashima Y, Ebihara Y, Tamoto E, Nakamura T, Murakami S, Okamura K, Shichinohe T, Hirano S. Hilar cholangiocarcinoma with intratumoral calcification: A case report. World J Gastroenterol 2015; 21(38): 10926-10930
- URL: https://www.wjgnet.com/1007-9327/full/v21/i38/10926.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i38.10926
Calcification in the hepatic hilum is commonly caused by hepatolithiasis, which is defined as the presence of bile stones in the bile ducts proximal to the confluence of the right and left hepatic ducts[1]. The incidence of hepatolithiasis is as high as 18%-45% of patients with gallstone disease in East Asia[1], and the disease has become more prevalent in Western countries due to an increase in migrants from endemic regions[2,3]. By contrast, hilar cholangiocarcinoma with intratumoral calcification is an extremely rare cause of calcification in the hepatic hilus, with only one previously reported case in the English literature[4].
Although imaging findings are quite similar, the differential diagnosis between hepatolithiasis and calcified Klatskin tumor is crucial because of their different prognoses. We present a rare case of calcified hilar cholangiocarcinoma mimicking hepatolithiasis.
A 73-year-old man was admitted to a local hospital for investigation of a calcified lesion in the hepatic hilum associated with a dilated left intrahepatic bile duct. He initially received a diagnosis of hepatolithiasis. Endoscopic stone extraction via the trans-papillary route was attempted but was unsuccessful due to stricture of the left hepatic duct. He was referred to our hospital for further examination.
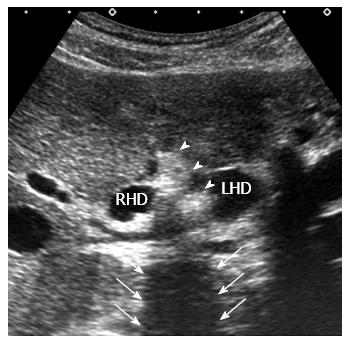
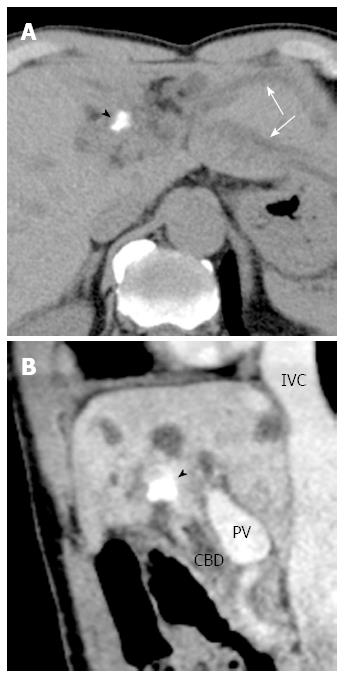
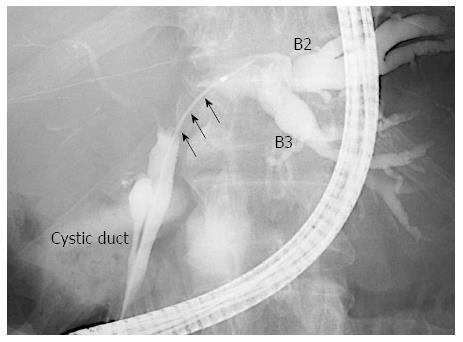
On admission, a blood test revealed mild elevation of carbohydrate antigen 19-9 (46.3 U/mL), though no elevation of carcinoembryonic antigen. All other laboratory findings, including serum concentrations of total bilirubin, aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase and γ-glutamyl transpeptidase, were within normal ranges. Hepatic ultrasonography showed a 33.5 mm × 26.5 mm intraductal mass at the confluence of the right and left hepatic duct. In addition, a highly echogenic mass with posterior acoustic shadowing was observed, suggesting a calcified lesion (Figure 1). Enhanced multi-detector-row computed tomography (CT) revealed marked dilatation of the left intrahepatic bile ducts upstream from the calcification and enhancement of the bile duct wall distal to the calcification (Figure 2). Endoscopic retrograde cholangiography (ERC) showed significant biliary stricture and disruption at the left hepatic duct, but no defect area (Figure 3). Furthermore, biopsy of the left hepatic duct was suggestive of adenocarcinoma.
Based on these findings, we diagnosed hilar cholangiocarcinoma complicated by the hepatolithiasis and decided to perform left hepatectomy with caudate lobectomy and extrahepatic bile duct resection. The patient underwent the scheduled operation. The operative time was 625 min, and the total blood loss was 1165 mL. No blood transfusion was required.
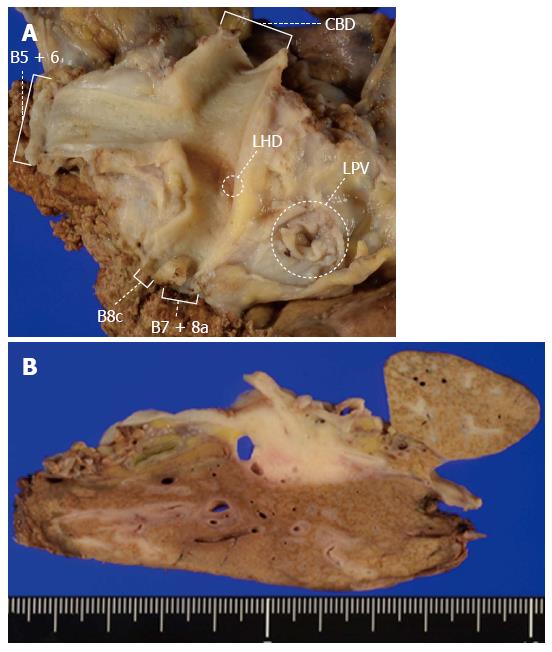
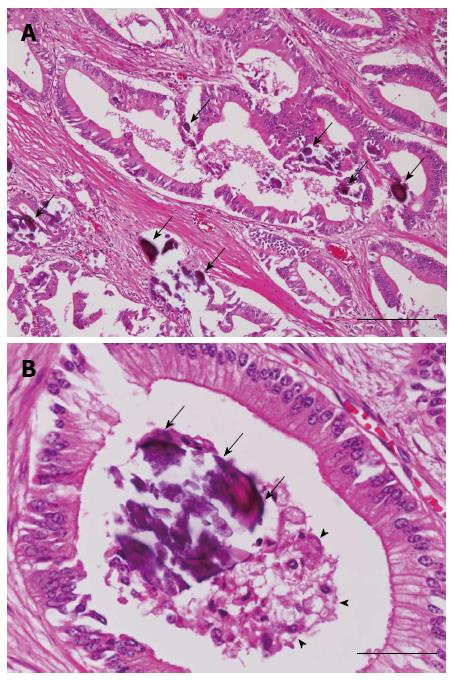
On histopathological examination, the tumor was found to have spread from the hepatic hilum to the left hepatic duct. The tumor was mucus-secreting and very hard, measuring 28 mm × 21 mm. It was a nodular-infiltrating type cholangiocarcinoma mainly existing in the perihilar bile duct with an abundance of fine calcification. No stones were found by the gross examination in the hilar lesion (Figure 4).
A regional lymph node in the hepatoduodenal ligament was invaded by tumor cells. Microscopically, this tumor was a gastric foveolar type adenocarcinoma and was rich in mucus. On the other hand, the majority of the calcified material was located within or replaced the tumor glands (Figure 5).
The postoperative course was uneventful, and the patient was discharged 21 d after surgery. At 7 mo after the surgery, the patient was well, without evidence of a recurrence of the disease.
This case report represents an unusual calcified hilar cholangiocarcinoma, which mimicked hepatolithiasis in clinical findings. To the best of our knowledge, there is only one article describing calcified Klatskin tumor in the literature[4].
The typical cause of calcified lesion in the porta hepatis is a calculus; in patients with primary calcium bilirubinate hepatolithiasis, stones are frequently located in the large bile ducts, such as the main hepatic ducts[5]. Histologically, in patients with hepatolithiasis, fibrotic changes in the bile duct walls and periductal hepatic parenchyma are often seen and lead to stricture formation[6,7]. Furthermore, hepatolithiasis is closely associated with concomitant cholangiocarcinoma with an incidence of approximately 5%[8], and this malignant lesion is also associated with biliary stricture[3]. Thus, among patients with hepatolithiasis, a calcified lesion is often associated with a biliary stenosis lesion caused by periductal fibrosis or cholangiocarcinoma[3].
In the present case, initial imaging findings showed a perihilar calcified lesion associated with the dilated proximal bile duct and the stricture lesion distal to the calcification. These findings were confusingly similar to those of hepatolithiasis associated with biliary stricture, and it was extremely difficult to make an accurate diagnosis using available radiological findings. In the previously reported case, the radiologic findings of the calcified Klatskin tumor were also very similar to those of hepatolithiasis, which resulted in biliary obstruction and proximal ductal dilation[4]. Because of these similarities in imaging findings, even more than the rarity of the disease, it can be difficult to make an accurate preoperative diagnosis of calcified hilar cholangiocarcinoma. ERC in this case, however, did not show a defective area, which is typically found in hepatolithiasis. In retrospect, this point might have suggested that the calcification in this case originated from diseases other than that of hepatolithiasis.
The pathogenesis of intratumoral calcification is mainly dystrophic calcification, which refers to the macroscopic deposition of calcium salts in injured tissues with normal serum levels of calcium[9]. In the dystrophic process, deranged cells form seed crystals that become encrusted with the mineral deposits, and the acquisition of outer layers gradually creates its lamellated configurations[10]. This type of calcification is most commonly observed in papillary thyroid carcinoma, meningioma, and papillary serous cyst adenocarcinoma of the ovary at the frequency of 40%-50%, 45%, and 33% of cases respectively[10]. Additionally, mucus-producing adenocarcinoma contributes to the deposition of calcium by via the actions of mucin glycoproteins as an ion-exchange resin[11]. Mucinous adenocarcinoma, which is a typical and frequently occurring histological type of colorectal cancer, can have fine or punctate calcification due to its mucinous component[12,13]. In intrahepatic cholangiocarcinoma, it is usually thought that, in addition to necrotic areas of the tumor, calcification occurs as a secondary reaction to mucin secretions[13,14]. In the present case, the intratumoral calcification was observed in the absence of a dysfunction in calcium metabolism, so it was thought that the calcification had formed in the dystrophic process. In addition, at the time of microscopic examination in this case, the tumor was noted to be a gastric foveolar type adenocarcinoma and was rich in mucus. Calcium deposition was seen in foveolar cells itself and the mucus in the glands. Therefore, the tumoral calcification in this case appears to reflect an accumulation of calcium secondary to dystrophy of tumor tissue and a mucus component produced by the tumor.
In conclusion, we presented an extremely rare case of hilar cholangiocarcinoma with intratumoral calcification. Radiological findings of this case were similar to those of hepatolithiasis. The pathogenic mechanism of this calcification was thought to be a dystrophic process that was associated with mucus.
A 73-year-old man presented with an asymptomatic calcified lesion in the hepatic hilum.
Upon physical examination, the patient had no clinical abnormality.
Hepatolithiasis.
A blood test revealed mild elevation of carbohydrate antigen (CA) 19-9 (46.3 U/mL), while metabolic panel and liver function test were within normal limits.
Ultrasonography/computed tomography revealed a highly echogenic mass or high-density area at the hepatic hilum with dilated left intrahepatic bile ducts.
Pathological examination revealed a nodular-infiltrating type cholangiocarcinoma mainly in the perihilar bile duct with abundance of fine calcification.
The patient underwent left hepatectomy with caudate lobectomy and extrahepatic bile duct resection.
Hilar cholangiocarcinoma with intratumoral calcification is an extremely rare cause of calcification in the hepatic hilum, with only one previous case report in the English literature.
Dystrophic calcification refers to the macroscopic deposition of calcium salts in injured tissues.
This case report describes a rare case of calcified hilar cholangiocarcinoma and reveals its clinicopathologic features. Imaging findings of this case were confusingly similar to those of hepatolithiasis, and it was extremely difficult to make an accurate diagnosis based on available radiological findings.
This article highlights the clinical characteristics of calcified hilar cholangiocarcinoma and discusses the pathogenic mechanism of this calcification.
P- Reviewer: Lee HC S- Editor: Yu J L- Editor: A E- Editor: Ma S
| 1. | Pausawasdi A, Watanapa P. Hepatolithiasis: epidemiology and classification. Hepatogastroenterology. 1997;44:314-316. [PubMed] |
| 2. | Al-Sukhni W, Gallinger S, Pratzer A, Wei A, Ho CS, Kortan P, Taylor BR, Grant DR, McGilvray I, Cattral MS. Recurrent pyogenic cholangitis with hepatolithiasis--the role of surgical therapy in North America. J Gastrointest Surg. 2008;12:496-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Park HS, Lee JM, Kim SH, Jeong JY, Kim YJ, Lee KH, Choi SH, Han JK, Choi BI. CT Differentiation of cholangiocarcinoma from periductal fibrosis in patients with hepatolithiasis. AJR Am J Roentgenol. 2006;187:445-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Park HS, Han JK, Lee HS, Lee KH, Kim SH, Kim KW, Kim YJ, Kim HC, Choi BI. Calcified Klatskin tumor mimicking intrahepatic stone: case report. Abdom Imaging. 2005;30:90-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 5. | Kondo S, Nimura Y, Hayakawa N, Kamiya J, Nagino M, Miyachi M, Kanai M. A clinicopathologic study of primary cholesterol hepatolithiasis. Hepatogastroenterology. 1995;42:478-486. [PubMed] |
| 6. | Nakanuma Y, Terada T, Tanaka Y, Ohta G. Are hepatolithiasis and cholangiocarcinoma aetiologically related A morphological study of 12 cases of hepatolithiasis associated with cholangiocarcinoma. Virchows Arch A Pathol Anat Histopathol. 1985;406:45-58. [PubMed] |
| 7. | Chan FL, Man SW, Leong LL, Fan ST. Evaluation of recurrent pyogenic cholangitis with CT: analysis of 50 patients. Radiology. 1989;170:165-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 45] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Chen MF, Jan YY, Wang CS, Hwang TL, Jeng LB, Chen SC, Chen TJ. A reappraisal of cholangiocarcinoma in patient with hepatolithiasis. Cancer. 1993;71:2461-2465. [PubMed] |
| 9. | Strayer DS, Rubin E. Cell adaptation, cell injury and cell death. Rubin’s pathology: clinicopathologic foundations of medicine. 6th ed. Philadelphia: Lippincott Williams & Wilkins 2011; 13. |
| 10. | Das DK. Psammoma body: a product of dystrophic calcification or of a biologically active process that aims at limiting the growth and spread of tumor. Diagn Cytopathol. 2009;37:534-541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 105] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 11. | Batlan LE. Calcification within the stomach wall in gastric malignancy; case report and review of literature. Am J Roentgenol Radium Ther Nucl Med. 1954;72:788-794. [PubMed] |
| 12. | Ko EY, Ha HK, Kim AY, Yoon KH, Yoo CS, Kim HC, Kim JC. CT differentiation of mucinous and nonmucinous colorectal carcinoma. AJR Am J Roentgenol. 2007;188:785-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Stoupis C, Taylor HM, Paley MR, Buetow PC, Marre S, Baer HU, Vock P, Ros PR. The Rocky liver: radiologic-pathologic correlation of calcified hepatic masses. Radiographics. 1998;18:675-685; quiz 726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 50] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 14. | Ros PR, Buck JL, Goodman ZD, Ros AM, Olmsted WW. Intrahepatic cholangiocarcinoma: radiologic-pathologic correlation. Radiology. 1988;167:689-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 102] [Article Influence: 2.8] [Reference Citation Analysis (0)] |