Published online Aug 14, 2015. doi: 10.3748/wjg.v21.i30.9217
Peer-review started: February 27, 2015
First decision: April 13, 2015
Revised: April 26, 2015
Accepted: June 9, 2015
Article in press: June 10, 2015
Published online: August 14, 2015
Processing time: 171 Days and 4.1 Hours
We report a case of a 56-year-old woman with a history of allogenic bone marrow transplantation for two years, complaining with dysphagia and weight loss. Upper endoscopy revealed esophageal stenosis and extensive mucosa sloughing. Biopsies confirmed the diagnosis of graft-vs-host disease (GVHD). Balloon dilation, corticosteroids and cyclosporin resulted in marked clinical improvement. Gastrointestinal tract is involved in the majority of patients with chronic GVHD. Esophageal manifestations are rare and include vesiculobullous disease, ulceration, esophageal webs, casts or strictures. Sloughing esophagitis along with severe stenosis requiring endoscopic dilation has never been reported in this context.
Core tip: Esophageal manifestations of graft-vs-host disease (GVHD) are very rare. We report a case of sloughing esophagitis along with severe stenosis requiring endoscopic dilation, as a manifestation of chronic GVHD, after allogenic bone marrow transplantation. This manifestation has never been reported in this context. Endoscopy may play a significant role in early diagnosis and treatment of esophageal GVHD. Histological examination of gastrointestinal biopsies is needed to confirm the diagnosis.
-
Citation: Trabulo D, Ferreira S, Lage P, Rego RL, Teixeira G, Pereira AD. Esophageal stenosis with sloughing esophagitis: A curious manifestation of graft-
vs -host disease. World J Gastroenterol 2015; 21(30): 9217-9222 - URL: https://www.wjgnet.com/1007-9327/full/v21/i30/9217.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i30.9217
Graft-vs-host disease (GVHD) is a serious complication of allogenic hematopoietic stem cell transplantation (HSCT). It is a multisystem disorder that can involve the skin, gastrointestinal (GI) tract and liver[1]. Nausea, vomiting, anorexia and diarrhea are common manifestations of GI-GVHD, but they may also be attributable to chemoradiation toxicity, medication side effects or infections[1,2]. Thus, it is difficult to establish the diagnosis based only on clinical grounds.
Sometimes, GI-GVHD can cause life-threatening complications such as massive diarrhea, hemorrhage, paralytic ileus and perforation[3,4]. Therefore, recognition of GI-GVHD is essential for directing specific therapy. Although endoscopy with biopsy is accurate in the identification of GI-GVHD, several mucosal patterns can be observed, ranging from normal to mild edema or severe erythema, exudates, erosions and ulceration[2,5].
In particular, involvement of the esophagus in chronic-GVHD (initially defined as a disorder occuring 100 d after HSCT)[1] is not common, with only a few reports found in the literature[5-8]. It can be manifested as a vesiculobullous disease, ulceration, web, desquamative esophagitis, esophageal cast or stricture[1,2,5-9].
We report a rare case of chronic-GVHD with esophageal involvement, presenting with dysphagia and weight loss, due to severe esophageal stenosis and mucosal sloughing.
A 56-year-old woman with acute myeloid leukemia M5b (monocitic) underwent allogenic bone marrow transplantation (BMT). After 3 mo, she developed a full-body skin rash and abnormal liver function tests with increased bilirubin. She was diagnosed with acute GVHD and was treated with prednisolone (1 mg/kg per day) and cysclosporine. The patient improved clinically and after 10 mo of therapy, prednisolone was discontinued.
Two years after transplantation, the patient complained with dysphagia for solids with progressive worsening in the last 2 wk and was referred to Gastroenterology Department. She reported xerostomia, anorexia and weight loss of 18 kg in 2 mo (> 20% of total body weight). Physical exam revealed aphthous stomatitis and skin lesions of the lower limbs, with pruriginous and erythematous papules, desquamation and induration areas (Figure 1). Her blood pressure, pulse rate, and body temperature were normal. Neurological examination was normal. Laboratory studies revealed hemoglobin 11.5 g/dL, leucocytes 11000, albumin 2.7 g/dL, AST 82 IU/L, ALT 87 IU/L, alkaline phosphatase 514 IU/L, GGT 282 IU/L, total bilirubin 1.3 mg/dL, C-reactive protein 1.17 mg/dL, international normalized ratio (INR) 1.1, antinuclear antibody (ANA) 1:160. Hepatitis A, B and C, HIV, cytomegalovirus, herpes and Epstein-Barr virus infections were ruled out by serology. Based on these observations, we considered as more probable the diagnostic hypothesis of chronic GVHD with GI, cutaneous and liver involvement. We also considered systemic-cutaneous auto-immune diseases (pemphigus, pemphigoid), infectious esophagitis, central cause dysphagia or a paraneoplastic syndrome/LMA recurrence.
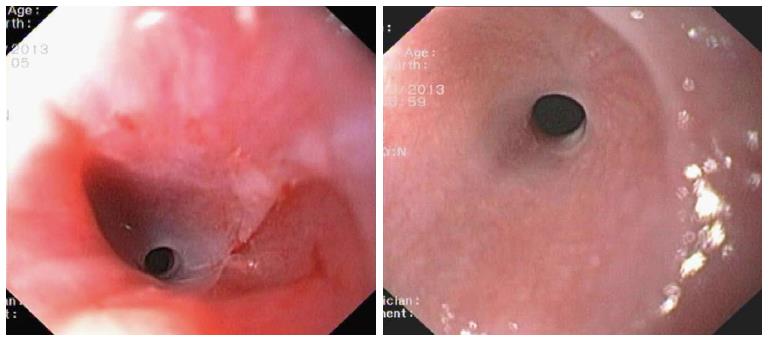
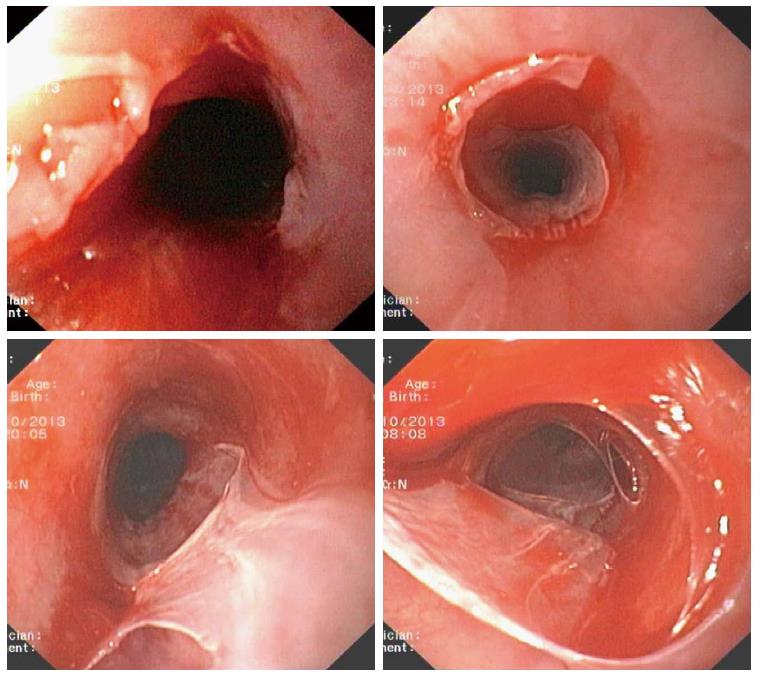
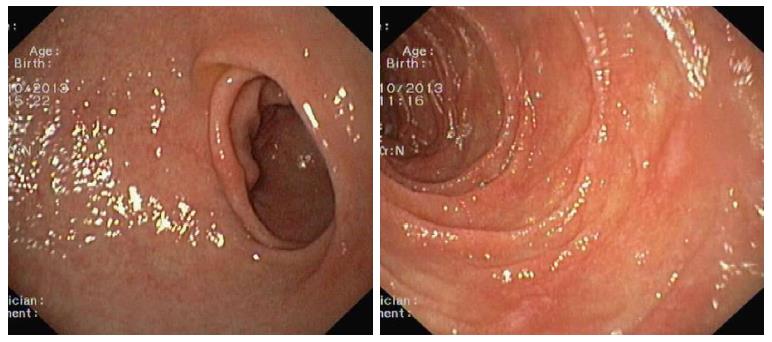
Upper GI endoscopy was performed and at 17 cm from the dental arch, we identified a regular ring, with 5 mm in diameter, causing unsurpassable obstructive stenosis (Figure 2). After barium instillation, we concluded that the stenosis was 1 cm length and proceeded to progressive dilation with Hercules® 3 stage wire guided balloon (Cook Medical) to 13.5 mm. After dilation, we were easily able to overcome the stenosis and observed friability and severe extensive detachment of the esophageal mucosa (Figure 3). In bulbar apex and second portion of duodenum, the mucosa was irregular with hyperemia and pearly areas (Figure 4). Esophageal, gastric and duodenal biopsies were obtained.
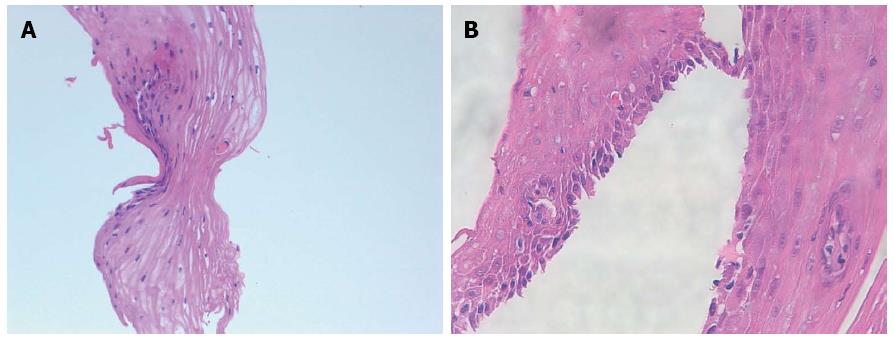
Esophageal biopsies showed increased intraepithelial lymphocytes, dyskeratotic squamous cells and apoptosis of individual squamous cells, with acanthosis and spongiosis. Congestion of the subepithelial vessels and increased submucosal fibrosis were also observed (Figure 5). These findings suggested the diagnosis of GVHD. Duodenal and gastric biopsies supported the diagnosis. Special stains for fungi and CMV were negative. Skin biopsies also confirmed the diagnosis of chronic GVHD.
The patient was treated with intravenous prednisolone 1 mg/kg per day, cyclosporine 1.5 mg/kg, 12 h/12 h and antifungal prophylaxis with posaconazole 300 mg/d. After 20 d of follow-up, she reported marked improvement of the dysphagia, with tolerance for solids and weight gain of 8 kg. Cutaneous lesions and laboratory studies also improved significantly. Prednisolone was maintained for 3 mo and then tapered for a total duration of 9 mo. Immunosuppressive therapy was maintained for 2 years.
Acute and chronic GVHD are multisystem disorders that are common complications of allogenic HSCT[1]. They occur when immune cells transplanted from a non-identical donor recognize the transplant recipient as foreign, thereby initiating an immune reaction that causes disease in the transplant recipient[9].
GVHD, the leading cause of morbidity and mortality after HSCT[2], has been classically divided into acute and chronic variants based upon the time of onset using a cutoff of 100 d[1]. However, this conventional division has been challenged by the recognition that signs of acute and chronic GVHD may occur outside these designated periods. This has led to the increased use of clinical findings, rather than a set time period, to differentiate between acute and chronic GVHD. The National Institute of Health consensus criteria for the diagnosis of GVHD include an overlap syndrome in which diagnostic or distinctive features of acute and chronic GVHD appear together[1].
Clinical manifestations of acute GVHD include a classic maculopapular rash (70%), nausea, vomiting (and) abdominal cramps with high-volume diarrhea (74%) and liver involvement (44%) with a rising serum bilirubin[10]. Patients with chronic GVHD commonly demonstrate skin involvement (67%) resembling lichen planus or cutaneous manifestations of scleroderma; dry oral mucosa with ulcerations (60%); dysphagia, weight loss, chronic diarrhea and malabsortion (30%); liver involvement (52%) suggested by elevations in serum alkaline phophatase and bilirubin concentrations; and pulmonar involvement (50%) resulting in bronchiolitis obliterans[1,11]. Chronic GVHD can also result in exocrine pancreatic insufficiency[1,11].
The GI tract is involved in the majority of patients with chronic GVHD[1,11]. Oral lesions are seen in 60% of patients and other areas of GI tract involvement are present in 30%[11]. The diagnosis is often difficult because of the nonspecific GI symptoms. In fact, they may also be attributable to chemoradiation toxicity, medication side effects or a variety of bacterial, fungal and viral infections[2].
Risk factors for the development of chronic GVHD include higher degree of HLA mismatching, older age of donor/receptor, donor and receptor gender disparity, source of stem cells (peripheral blood rather than bone marrow), cytomegalovirus seropositivity and prior acute GVHD[1,11]. In fact, our patient developed acute GVHD, 3 mo after BMT.
Endoscopy with biopsies remains the gold standard for the diagnosis of GI-GVHD[2]. The endoscopic appearance can range from normal to edema, eythema, erosion, ulceration and active bleeding. Histological criteria are the presence of epitelial single-cell apoptosis and crypt cell dropout[12]. There is a discrepancy between endoscopic and histologic assessment of the severity of GI-GVHD[2].
Esophageal involvement in GVHD occurs in less than 15% of BMT patients[13]. This can be manifested as vesiculobullous disease, esophageal cast, desquamative or sloughing esophagitis (esophageal dissecans superficialis), or severe ulceration which leads to web and stricture formation[1,2,5-9,13]. In patients with chronic GVHD, the production of autoantibodies may alter intercelular adhesions and cell matrix adhesion leading to desquamative esophagitis and stenosis[7-12].
We report a case of severe chronic GVHD two years after BMT. In fact, the patient presented involvement of the skin (erythematous papules, desquamation and induration areas in the lower limbs), liver (altered liver function tests) and esophagus (esophageal stricture and mucosal sloughing). Only a few cases of esophageal manifestations of GVHD were reported in literature[5-9]. Moreover, a wide area of sloughing mucosa along with severe stenosis requiring endoscopic dilation, as observed in the present case, has never been reported. Therefore, we point out that this is a rare complication of chronic GVHD, which is associated to the patient’s background disease and its treatment - bone marrow transplantation for acute myeloid leukemia two years ago.
In conclusion, esophageal stenosis and sloughing esophagitis are rare but typical manifestations of chronic-GVHD. This diagnosis should be considered when assessing patients with history of BMT.
A 56-year-old woman with a history of allogenic bone marrow transplantation for two years, presented with dysphagia, xerostomia, anorexia, and weight loss.
Physical exam revealed aphthous stomatitis and skin lesions of the lower limbs, with pruriginous and erythematous papules, desquamation and induration areas.
The authors considered the diagnosis of chronic graft-vs-host disease (GVHD) with gastrointestinal (GI) and cutaneous involvement; systemic-cutaneous auto-immune diseases (pemphigus, pemphigoid); infectious esophagitis; central cause dysphagia; paraneoplastic syndrome or LMA recurrence.
Laboratory studies revealed hemoglobin 11.5 g/dL, leucocytes 11000, albumin 2.7 g/dL, AST 82 IU/L, ALT 87 IU/L, alkaline phosphatase 514 IU/L, GGT 282 IU/L, total bilirubin 1.3 mg/dL.
Upper GI endoscopy identified a regular ring in cervical esophagus, causing unsurpassable obstructive stenosis, as well as friability and severe extensive detachment of the esophageal mucosa.
Esophageal biopsies showed increased intraepithelial lymphocytes, dyskeratotic squamous cells and apoptosis of individual squamous cells, with acanthosis and spongiosis, congestion of the subepithelial vessels and increased submucosal fibrosis.
Endoscopic dilation of the esophageal stenosis; prednisolone 1 mg/kg per day, cyclosporine 1.5 mg/kg, 12 h/12 h and posaconazole 300 mg/d.
Very few cases of esophageal manifestations of GVHD are reported in literature. Sloughing esophagitis along with severe stenosis requiring endoscopic dilation has never been reported in this context.
This case report presents the clinical and endoscopic characteristics of an extremely rare and curious manifestation of esophageal GVHD, which required endoscopic intervention. Therefore, endoscopy may play a significant role in the early diagnosis and treatment of GVHD.
The case report written by Trabulo et al describes a case of graft-vs-host disease complicating a rare esophageal lesion. The case report is a unique and interesting one, and well-described. This severe form of complication is related to the treatment (bone marrow transplantation) of acute leukemia and subsequent development of graft vs host disease.
P- Reviewer: Saligram S, Shimizu Y S- Editor: Yu J L- Editor: A E- Editor: Liu XM
| 1. | Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, Martin P, Chien J, Przepiorka D, Couriel D. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant. 2005;11:945-956. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2645] [Cited by in RCA: 2883] [Article Influence: 151.7] [Reference Citation Analysis (0)] |
| 2. | Xu CF, Zhu LX, Xu XM, Chen WC, Wu DP. Endoscopic diagnosis of gastrointestinal graft-versus-host disease. World J Gastroenterol. 2008;14:2262-2267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 3. | Okubo H, Nagata N, Uemura N. Fulminant gastrointestinal graft-versus-host disease concomitant with cytomegalovirus infection: case report and literature review. World J Gastroenterol. 2013;19:597-603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Irani JL, Cutler CS, Whang EE, Clancy TE, Russell S, Swanson RS, Ashley SW, Zinner MJ, Raut CP. Severe acute gastrointestinal graft-vs-host disease: an emerging surgical dilemma in contemporary cancer care. Arch Surg. 2008;143:1041-1045; discussion 1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | McDonald GB, Sullivan KM, Schuffler MD, Shulman HM, Thomas ED. Esophageal abnormalities in chronic graft-versus-host disease in humans. Gastroenterology. 1981;80:914-921. [PubMed] |
| 6. | Minocha A, Mandanas RA, Kida M, Jazzar A. Bullous esophagitis due to chronic graft-versus-host disease. Am J Gastroenterol. 1997;92:529-530. [PubMed] |
| 7. | Nakshabendi IM, Maldonado ME, Coppola D, Mamel JJ. Esophageal cast: a manifestation of graft-versus-host disease. Dig Dis. 2000;18:103-105. [PubMed] |
| 8. | Memoli D, Spitzer TR, Cottler-Fox M, Cahill R, Benjamin S, Deeg HJ. Acute esophageal stricture after bone marrow transplantation. Bone Marrow Transplant. 1988;3:513-516. [PubMed] |
| 9. | Ratanatharathorn V, Ayash L, Lazarus HM, Fu J, Uberti JP. Chronic graft-versus-host disease: clinical manifestation and therapy. Bone Marrow Transplant. 2001;28:121-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 169] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 10. | Chao NJ. Clinical manifestations, diagnosis and grading of acute graft-vs-host disease. Accessed in April 11, 2013. Available from: http://www.uptodate.com. |
| 11. | Chao NJ. Clinical manifestations, diagnosis and grading of chronic graft-vs-host disease. Accessed in August 11, 2013. Available from: http://www.uptodate.com. |
| 12. | Velasco-Guardado A, López-Corral L, Alvarez-Delgado A, Flores-Corral T, Geijo-Martínez F, Caballero-Barrigón D, Rodríguez-Pérez A. Endoscopic evaluation and histological findings in graft-versus-host disease. Rev Esp Enferm Dig. 2012;104:310-314. [PubMed] |
| 13. | McDonald GB, Sullivan KM, Plumley TF. Radiographic features of esophageal involvement in chronic graft-vs.-host disease. AJR Am J Roentgenol. 1984;142:501-506. [PubMed] |