Published online Aug 14, 2015. doi: 10.3748/wjg.v21.i30.9182
Peer-review started: January 19, 2015
First decision: February 10, 2015
Revised: February 25, 2015
Accepted: April 28, 2015
Article in press: April 30, 2015
Published online: August 14, 2015
Processing time: 210 Days and 21.9 Hours
AIM: To compare the clinical outcomes between 0.025-inch and 0.035-inch guide wires (GWs) when used in wire-guided cannulation (WGC).
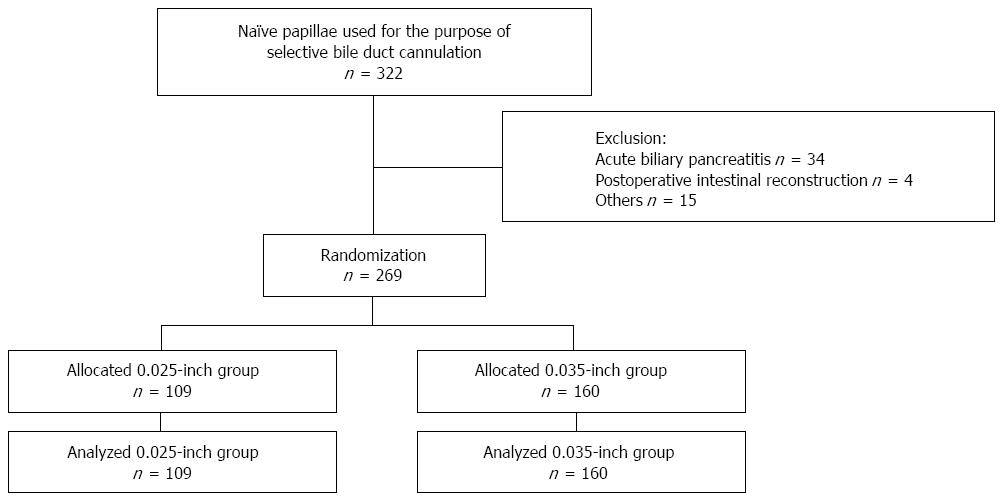
METHODS: A single center, randomized study was conducted between April 2011 and March 2013. This study was approved by the Medical Ethics Committee at our hospital. Informed, written consent was obtained from each patient prior to study enrollment. Three hundred and twenty-two patients with a naïve papilla of Vater who underwent endoscopic retrograde cholangiopancreatography (ERCP) for the purpose of selective bile duct cannulation with WGC were enrolled in this study. Fifty-three patients were excluded based on the exclusion criteria, and 269 patients were randomly allocated to two groups by a computer and analyzed: the 0.025-inch GW group (n = 109) and the 0.035-inch GW group (n = 160). The primary endpoint was the success rate of selective bile duct cannulation with WGC. Secondary endpoints were the success rates of the pancreatic GW technique and precutting, selective bile duct cannulation time, ERCP procedure time, the rate of pancreatic duct stent placement, the final success rate of selective bile duct cannulation, and the incidence of post-ERCP pancreatitis (PEP).
RESULTS: The primary success rates of selective bile duct cannulation with WGC were 80.7% (88/109) and 86.3% (138/160) for the 0.025-inch and the 0.035-inch groups, respectively (P = 0.226). There were no statistically significant differences in the success rates of selective bile duct cannulation using the pancreatic duct GW technique (46.7% vs 52.4% for the 0.025-inch and 0.035-inch groups, respectively; P = 0.884) or in the success rates of selective bile duct cannulation using precutting (66.7% vs 63.6% for the 0.025-inch and 0.035-inch groups, respectively; P = 0.893). The final success rates for selective bile duct cannulation using these procedures were 92.7% (101/109) and 97.5% (156/160) for the 0.025-inch and 0.035-inch groups, respectively (P = 0.113). There were no significant differences in selective bile duct cannulation time (median ± interquartile range: 3.7 ± 13.9 min vs 4.0 ± 11.2 min for the 0.025-inch and 0.035-inch groups, respectively; P = 0.851), ERCP procedure time (median ± interquartile range: 32 ± 29 min vs 30 ± 25 min for the 0.025-inch and 0.035-inch groups, respectively; P = 0.184) or in the rate of pancreatic duct stent placement (14.7% vs 15.6% for the 0.025-inch and 0.035-inch groups, respectively; P = 0.832). The incidence of PEP was 2.8% (3/109) and 2.5% (4/160) for the 0.025-inch and 0.035-inch groups, respectively (P = 0.793).
CONCLUSION: The thickness of the GW for WGC does not appear to affect either the success rate of selective bile duct cannulation or the incidence of PEP.
Core tip: The thickness of the guide wire for wire-guided cannulation does not appear to affect either the success rate of selective bile duct cannulation or the incidence of post-endoscopic retrograde cholangiopancreatography pancreatitis.
- Citation: Kitamura K, Yamamiya A, Ishii Y, Sato Y, Iwata T, Nomoto T, Ikegami A, Yoshida H. 0.025-inch vs 0.035-inch guide wires for wire-guided cannulation during endoscopic retrograde cholangiopancreatography: A randomized study. World J Gastroenterol 2015; 21(30): 9182-9188
- URL: https://www.wjgnet.com/1007-9327/full/v21/i30/9182.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i30.9182
Endoscopic retrograde cholangiopancreatography (ERCP) is important for diagnosing and performing procedures related to the biliary tract and pancreatic disease. Selective bile duct cannulation is a basic biliary tract procedure in ERCP. Cannulation using contrast medium has been performed as a conventional cannulation technique; however, it has been suggested that pancreatic contrast injection might be associated with the mechanism of post-ERCP pancreatitis (PEP)[1]. According to several reports, the incidence of PEP following this procedure is 1%-15%[2-5]. In a meta-analysis of randomized, controlled trials (RCTs), it was suggested that selective bile duct cannulation using wire-guided cannulation (WGC) might improve the primary bile duct cannulation rate and reduce the risk of PEP[6].
A sphincterotome or catheter and a guide wire (GW) are necessary for the WGC procedure. Various GWs are used, such as a straight or an angled type of tip with different outer diameters. One report suggested that there were no significant differences in the success rate of primary cannulation or in the risk of adverse events between 0.025-inch and 0.035-inch GWs[7]; however, no consensus exists regarding the type of GW that is most appropriate for the WGC procedure.
The aim of this study was to investigate whether clinical differences exist in the success rate of selective bile duct cannulation and the incidence of PEP during WGC using 0.025-inch or 0.035-inch GWs.
This study was conducted as an exploratory randomized study at Showa University Hospital. The study protocol was approved by the Medical Ethics Committee at our hospital and was registered at UMIN Clinical Trial Registry (UMIN000010082). Informed, written consent was obtained from each patient. Endoscopists performed ERCP either as an operator or as an assistant.
The success rate of selective bile duct cannulation with WGC using a sphincterotome is reportedly 69.1%-98.5%[8-13]. The sample size was calculated based on the assumption of a 90% success rate of selective bile duct cannulation using WGC. Non-inferiority was demonstrated within a margin of 10% at a one-sided significance level of 0.025 and a power of 80%, with a sample size of 142 patients in each group.
Between April 2011 and March 2013, 322 patients with a naïve papilla of Vater who underwent ERCP for the purpose of selective bile duct cannulation with WGC were enrolled in this study. Exclusion criteria were as follows: age under 15 years, postoperative intestinal reconstruction (Billroth II or Roux-en-Y), acute biliary pancreatitis, or inability to obtain informed consent. Fifty-three patients were excluded based on the exclusion criteria; the remaining 269 patients were randomly allocated to two groups using a computer and analyzed: the 0.025-inch GW group (n = 109) and the 0.035-inch GW group (n = 160) (Figure 1).
ERCP was performed using a duodenoscope (JF-260V; Olympus Medical Systems Corp, Tokyo, Japan). A 0.025-inch, 450-cm-long GW with an outer diameter of 0.65 mm or a 0.035-inch, 450-cm-long GW with an outer diameter of 0.91 mm with a straight tip (Jagwire; Boston Scientific, Natick, MA, United States) was used. Jagwire contains a nitinol core covered with polytetrafluoroethylene, and the tip is coated with a hydrophilic polymer. A sphincterotome with a tip length of 7 mm and a cutting wire length of 20 mm (Autotome RX39 or RX44; Boston Scientific) was used.
Physician-controlled WGC using a sphincterotome and a GW was performed for bile duct cannulation. When we could not perform bile duct cannulation within approximately ten minutes after seeing the papilla of Vater, bile duct cannulation using the pancreatic duct GW technique (double-wire technique) was attempted. If bile duct cannulation using the pancreatic duct GW technique was not successful within approximately five minutes, pancreatic sphincter precutting was performed. If cannulation with the GW to the pancreatic duct was difficult, precutting from the papilla of Vater without use of the pancreatic duct GW technique was performed. To prevent pancreatitis, all patients received intravenous infusions of protease inhibitor (gabexate mesilate, 600 mg) for approximately 12 h, beginning immediately after the ERCP procedures. A 5-Fr straight, 3-cm-long pancreatic duct stent, which was unflanged on the pancreatic ductal side and had 2 flanges on the duodenal side (GPDS-5-3, COOK Endoscopy Inc., Winston-Salem, NC, United States), was retained after performing the pancreatic GW technique and precutting. Stent dislodgments were confirmed using abdominal X-rays, which were recorded the day after ERCP.
The primary endpoint was the success rate of selective bile duct cannulation using WGC. The secondary endpoints were the success rates of the pancreatic GW technique and precutting, selective bile duct cannulation time, ERCP procedure time, the rate of pancreatic duct stent placement, the final success rate of selective bile duct cannulation, and the incidence of PEP.
PEP was defined as abdominal pain and serum amylase level more than three times the upper limit of normal within 24 h after the procedure[14]. The severity of PEP was graded according to widely accepted criteria: mild, requiring hospitalization for 2-3 d; moderate, requiring hospitalization for 4-10 d; and severe, requiring hospitalization for more than 10 d, requiring intervention (percutaneous drainage or surgery), the development of necrosis, or the development of a pseudocyst[14]. Other adverse events, such as bleeding, perforation, and cholangitis, were defined according to the same criteria[14].
Continuous variables are expressed as medians with interquartile ranges (IQRs). Statistical analyses were performed using StatMate III (ATMS Co. Ltd., Tokyo, Japan). Data were analyzed using the Mann-Whitney U-test and the χ2 test, and differences of P < 0.05 were considered significant.
Patient characteristics are shown in Table 1. There were no statistically significant differences in age and sex between the groups. There was significantly more cholangiocarcinoma in the 0.025-inch group than in the 0.035-inch group (P = 0.019), but other diseases were not significantly different between the groups. There were no significant differences in the biliary and pancreatic procedures between the groups.
| 0.025-inch group (n = 109) | 0.035-inch group (n = 160) | P value | |
| Age, median ± IQR, year (range) | 73 ± 12 (31-90) | 72 ± 16 (20-97) | 0.8691 |
| Sex male/female | 68/41 | 83/77 | 0.0882 |
| Benign disease | 69 (63.3) | 114 (71.3) | 0.1702 |
| Choledocholithiasis | 54 (49.5) | 78 (48.8) | 0.8992 |
| Gallbladder stones | 8 (7.3) | 15 (9.4) | 0.5582 |
| Benign biliary stricture | 5 (4.6) | 7 (4.4) | 0.8272 |
| Cholangitis | 1 (0.9) | 7 (4.4) | 0.2032 |
| Others | 1 (0.9) | 7 (4.4) | 0.2032 |
| Malignant disease | 40 (36.7) | 46 (28.8) | 0.1702 |
| Pancreatic cancer | 13 (11.9) | 26 (16.3) | 0.3232 |
| Cholangiocarcinoma | 12 (11.0) | 6 (3.8) | 0.0192 |
| Gallbladder cancer | 5 (4.6) | 3 (1.9) | 0.3582 |
| Ampullary cancer | 3 (2.8) | 3 (1.9) | 0.9542 |
| Cholangiocellular carcinoma | 1 (0.9) | 1 (0.6) | 0.6542 |
| Others | 6 (5.5) | 7 (4.4) | 0.8932 |
The primary success rates of bile duct cannulation using WGC were 80.7% and 86.3% for the 0.025-inch and in 0.035-inch groups, respectively (P = 0.226). Rates of use of the pancreatic duct GW technique were 13.8% and 13.1% for the 0.025-inch and 0.035-inch groups, respectively (P = 0.880), and the success rates of selective bile duct cannulation using the pancreatic duct GW technique were 46.7% and 52.4% for the 0.025-inch and 0.035-inch groups, respectively (P = 0.884). Precutting rates were 8.3% and 6.9% for the 0.025-inch and 0.035-inch groups, respectively (P = 0.672), and selective success rates of bile duct cannulation with precutting were 66.7% and 63.6% for the 0.025-inch and 0.035-inch groups, respectively (P = 0.893). The final success rates of selective bile duct cannulation using these procedures were 92.7% and 97.5% for the 0.025-inch and 0.035-inch groups, respectively (P = 0.113). There were no statistically significant differences regarding these procedures between the groups (Table 2).
| 0.025-inch group (n = 109) | 0.035-inch group (n = 160) | P value | |
| Success rate of selective bile duct cannulation with WGC | 88 (80.7) | 138 (86.3) | 0.2261 |
| Pancreatic duct GW | 15 (13.8) | 21 (13.1) | 0.8801 |
| Success rate of selective bile duct cannulation with pancreatic duct GW | 7 (46.7) | 11 (52.4) | 0.8841 |
| Precutting | 9 (8.3) | 11 (6.9) | 0.6721 |
| Success rate of selective bile duct cannulation with precutting | 6 (66.7) | 7 (63.6) | 0.8931 |
| Final success rate of selective bile duct cannulation | 101 (92.7) | 156 (97.5) | 0.1131 |
The pancreatic duct stent placement rate was 14.7% (16/109) in the 0.025-inch group and 15.6% (25/160) in the 0.035-inch group. There was no statistically significant difference in pancreatic duct stent placement between the groups (P = 0.832).
Median selective bile duct cannulation time was 3.7 min (IQR: 13.9) in the 0.025-inch group and 4.0 min (IQR: 11.2) in the 0.035-inch group. The median ERCP procedure times were 32 min (IQR: 29) and 30 min (IQR: 25) for the 0.025-inch and 0.035-inch groups, respectively. There were no statistically significant differences in selective bile duct cannulation time (P = 0.851) and ERCP procedure time (P = 0.184) between the groups.
PEP occurred in 2.8% of the 0.025-inch group and in 2.5% of the 0.035-inch group. There was no statistically significant difference in the incidence of PEP between the groups (P = 0.793). With respect to the severity of PEP, in the 0.025-inch group, 2 patients had moderate pancreatitis and 1 patient had severe pancreatitis, whereas in the 0.035-inch group, 1 patient had mild pancreatitis, 2 patients had moderate pancreatitis, and 1 patient had severe pancreatitis. Adverse events of bleeding, perforation, and cholangitis were not significantly different between the groups (Table 3).
Several reports noted that PEP occurred in 1%-15% of cases[2-5]. Risk factors for PEP in multivariate analyses were patient and procedure-related factors, such as young age, female sex, suspected sphincter of Oddi dysfunction, prior PEP, recurrent pancreatitis, chronic pancreatitis absent, pancreatic duct injection, pancreatic sphincterotomy, balloon dilation of intact biliary sphincter, difficult or failed cannulation, and pre-cut sphincterotomy[1].
Lella et al[8] reported that WGC using a sphincterotome reduced the incidence of PEP compared with the standard method with contrast injection. In a meta-analysis of RCTs without a cross-over design, it was reported that WGC increased the primary bile duct cannulation rate (OR = 2.05, 95%CI: 1.27-3.31) and decreased the incidence of PEP (OR = 0.23, 95%CI: 0.13-0.41) compared with the standard contrast injection method[6]. However, a meta-analysis of RCTs with a cross-over design by Shao et al[15] showed a non-significant reduction in the rate of PEP with the use of WGC. Based on these reports, the use of WGC for the prevention of PEP remains controversial.
The WGC technique includes physician-controlled (single-operator) or assistant-controlled cannulation. One report showed that the single-operator WGC technique was feasible, safe, and efficient without requiring an experienced assistant and precise coordination between the operator and assistant[16].
A sphincterotome or a catheter is used as the device for WGC. Kawakami et al[13] reported that WGC appears to significantly shorten cannulation and fluoroscopy times compared with the contrast injection method; however, there was no significant difference in either the success rate of bile duct cannulation or the PEP rate, regardless of the type of sphincterotome and catheter, based on a multicenter, prospective, randomized study.
A GW with a straight or angled tip is used for WGC. Several articles on WGC using GW with a straight or angled tip have been reported[11-13,17].
Normal and thin types of GW are used. It is not yet known which GW is more suitable for WGC. A prospective, randomized study reported that GW thickness did not appear to affect either the success rate of primary cannulation or the risk of adverse events[7]. In the present study of WGC using a 0.025-inch or a 0.035-inch GW of the straight type with a sphincterotome, the primary success rates of selective bile duct cannulation using WGC were 80.7% in the 0.025-inch group and 86.3% in the 0.035-inch group. No statistically significant difference was seen in the primary success rate of selective bile duct cannulation between the groups.
A case of difficult biliary cannulation was treated using the pancreatic duct GW technique, the double-wire technique, pancreatic duct stenting, needle knife precutting, and transpancreatic sphincterotomy as the next step[18-25].
In the present study, cannulation was performed using the pancreatic duct GW technique (double-wire technique) for a difficult bile duct cannulation using WGC; then, cannulation with precutting was performed for difficult bile duct cannulation using the pancreatic duct GW technique. The pancreatic duct GW procedure was performed in 36 patients (13.3%) for primary difficult bile duct cannulation using WGC; however, it was difficult to perform selective bile duct cannulation using the pancreatic duct GW technique in approximately half of the cases. No statistically significant differences were observed in the success rates of bile duct cannulation using the pancreatic duct GW technique between the groups (46.7% vs 52.4% for the 0.025-inch and 0.035-inch groups, respectively). Precutting was performed for difficult bile duct cannulation in 20 patients (12.5%). No statistically significant differences were observed in the success rates of bile duct cannulation with precutting between the groups (66.7% vs 63.6% for the 0.025-inch and 0.035-inch groups, respectively). The final success rates of selective bile duct cannulation using these techniques showed no statistically significant difference between the two groups (92.7% vs 97.5% for the 0.025-inch and 0.035-inch groups, respectively). Based on these results, it is suggested that successful bile duct cannulation appears equivalent for either GW during WGC.
The mechanism of PEP is suggested to involve a defect in pancreatic duct drainage that is caused by papillary edema, pancreatic duct injury, or spasm of the sphincter of Oddi after the ERCP procedure[1,14]. Several studies have reported the usefulness of endoscopic pancreatic duct drainage using a pancreatic duct stent for preventing PEP in patients at high risk[26-30]. In the present study, a pancreatic duct stent was used to treat 41 patients (15.2%) after using the pancreatic GW technique and precutting, which have been suggested as risk factors for PEP. There were no statistically significant differences in the rates of placement of pancreatic duct stents and the incidence of PEP between the two groups.
In this study, there were no statistically significant differences in the bile duct cannulation time and the ERCP procedure time between the groups. Halttunen et al[7] also reported that there were no significant differences in the bile duct cannulation time and the ERCP procedure time between the 0.025-inch and 0.035-inch GWs for WGC.
A difference in the incidence of PEP caused by the mechanical stimulation of the papilla of Vater and pancreatic duct cannulation due to the use of 0.025-inch or 0.035-inch GW with WGC was expected; however, no statistically significant difference was observed in the incidence of PEP between the groups (2.8% vs 2.5% for the 0.025-inch and 0.035-inch groups, respectively). Other adverse events of bleeding, perforation, and cholangitis were not significantly different between the groups. A previous study also reported that the thickness of the hydrophilic GW used in that study did not appear to affect the risk of adverse events[7].
A limitation of this study was the use of a small number of patients in a single center, with a consequent lack of power. Furthermore, a protease inhibitor was used to prevent PEP during the ERCP procedure in all cases.
In conclusion, the thickness of the GW during WGC does not appear to affect either the success rate of selective bile duct cannulation or the incidence of PEP. However, multi-center RCTs are needed to confirm these findings.
Selective bile duct cannulation using wire-guided cannulation (WGC) might improve the primary bile duct cannulation rate and reduce the risk of post-endoscopic retrograde cholangiopancreatography pancreatitis (PEP). However, no consensus exists regarding the type of guide wire (GW) that is most appropriate for the WGC procedure. The aim of this study was to investigate whether clinical differences exist in the success rate of selective bile duct cannulation and the incidence of PEP for WGC using 0.025-inch or 0.035-inch GWs.
A sphincterotome or catheter and GW are necessary for the WGC procedure. Various GWs are used, such as a straight or an angled type of tip with different outer diameters. However, there are few articles which compared clinical differences between 0.025-inch and 0.035-inch GWs with WGC.
The authors compared the clinical outcomes between 0.025-inch and 0.035-inch GWs for WGC, and showed that no clinical differences exist in the success rate of selective bile duct cannulation and the incidence of PEP with WGC using 0.025-inch or 0.035-inch GWs.
The results of this study suggest that the thickness of the GW for WGC does not appear to affect either the success rate of selective bile duct cannulation or the incidence of PEP. However, multi-center, randomized, controlled trials are needed to confirm these findings.
Wire-guided cannulation is a method of selective bile duct cannulation using the guide wire without contrast medium.
This is a most interesting study on the use of guidewires in ERCP. Randomized studies in endoscopy are scarce and the subject of this study is particularly of interest for the reader of the journal. Fairly well written paper on cannulation using regular and thin guide wire in random fashion. The result is expected slightly, although not statistically, favouring the regular wire.
P- Reviewer: Albert JG, Halttunen J S- Editor: Yu J L- Editor: Webster JR E- Editor: Zhang DN
| 1. | Freeman ML, Guda NM. Prevention of post-ERCP pancreatitis: a comprehensive review. Gastrointest Endosc. 2004;59:845-864. [PubMed] |
| 2. | Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, Dorsher PJ, Moore JP, Fennerty MB, Ryan ME, Shaw MJ. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996;335:909-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1716] [Cited by in RCA: 1690] [Article Influence: 58.3] [Reference Citation Analysis (2)] |
| 3. | Masci E, Toti G, Mariani A, Curioni S, Lomazzi A, Dinelli M, Minoli G, Crosta C, Comin U, Fertitta A. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001;96:417-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 625] [Cited by in RCA: 613] [Article Influence: 25.5] [Reference Citation Analysis (0)] |
| 4. | Freeman ML, DiSario JA, Nelson DB, Fennerty MB, Lee JG, Bjorkman DJ, Overby CS, Aas J, Ryan ME, Bochna GS. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001;54:425-434. [PubMed] |
| 5. | Cheng CL, Sherman S, Watkins JL, Barnett J, Freeman M, Geenen J, Ryan M, Parker H, Frakes JT, Fogel EL. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006;101:139-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 434] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 6. | Cennamo V, Fuccio L, Zagari RM, Eusebi LH, Ceroni L, Laterza L, Fabbri C, Bazzoli F. Can a wire-guided cannulation technique increase bile duct cannulation rate and prevent post-ERCP pancreatitis? A meta-analysis of randomized controlled trials. Am J Gastroenterol. 2009;104:2343-2350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 109] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Halttunen J, Kylänpää L. A prospective randomized study of thin versus regular-sized guide wire in wire-guided cannulation. Surg Endosc. 2013;27:1662-1667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Lella F, Bagnolo F, Colombo E, Bonassi U. A simple way of avoiding post-ERCP pancreatitis. Gastrointest Endosc. 2004;59:830-834. [PubMed] |
| 9. | Artifon EL, Sakai P, Cunha JE, Halwan B, Ishioka S, Kumar A. Guidewire cannulation reduces risk of post-ERCP pancreatitis and facilitates bile duct cannulation. Am J Gastroenterol. 2007;102:2147-2153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 125] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 10. | Bailey AA, Bourke MJ, Williams SJ, Walsh PR, Murray MA, Lee EY, Kwan V, Lynch PM. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy. 2008;40:296-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 164] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 11. | Katsinelos P, Paroutoglou G, Kountouras J, Chatzimavroudis G, Zavos C, Pilpilidis I, Tzelas G, Tzovaras G. A comparative study of standard ERCP catheter and hydrophilic guide wire in the selective cannulation of the common bile duct. Endoscopy. 2008;40:302-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 12. | Nambu T, Ukita T, Shigoka H, Omuta S, Maetani I. Wire-guided selective cannulation of the bile duct with a sphincterotome: a prospective randomized comparative study with the standard method. Scand J Gastroenterol. 2011;46:109-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 13. | Kawakami H, Maguchi H, Mukai T, Hayashi T, Sasaki T, Isayama H, Nakai Y, Yasuda I, Irisawa A, Niido T. A multicenter, prospective, randomized study of selective bile duct cannulation performed by multiple endoscopists: the BIDMEN study. Gastrointest Endosc. 2012;75:362-72, 372.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 75] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 14. | Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383-393. [PubMed] |
| 15. | Shao LM, Chen QY, Chen MY, Cai JT. Can wire-guided cannulation reduce the risk of post-endoscopic retrograde cholangiopancreatography pancreatitis? A meta-analysis of randomized controlled trials. J Gastroenterol Hepatol. 2009;24:1710-1715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 26] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Li QY, Pan L, Ling Q, He JD, Zhang LX, Zheng SS. Single-operator wire-guided cannulation technique enables easier cannulation of endoscopic retrograde cholangiopancreatography. Dig Dis Sci. 2012;57:3293-3298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Omuta S, Maetani I, Shigoka H, Gon K, Saito M, Tokuhisa J, Naruki M. Newly designed J-shaped tip guidewire: a preliminary feasibility study in wire-guided cannulation. World J Gastroenterol. 2013;19:4531-4536. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 7] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Maeda S, Hayashi H, Hosokawa O, Dohden K, Hattori M, Morita M, Kidani E, Ibe N, Tatsumi S. Prospective randomized pilot trial of selective biliary cannulation using pancreatic guide-wire placement. Endoscopy. 2003;35:721-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 107] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 19. | Herreros de Tejada A, Calleja JL, Díaz G, Pertejo V, Espinel J, Cacho G, Jiménez J, Millán I, García F, Abreu L. Double-guidewire technique for difficult bile duct cannulation: a multicenter randomized, controlled trial. Gastrointest Endosc. 2009;70:700-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 99] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 20. | Goldberg E, Titus M, Haluszka O, Darwin P. Pancreatic-duct stent placement facilitates difficult common bile duct cannulation. Gastrointest Endosc. 2005;62:592-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 32] [Article Influence: 1.6] [Reference Citation Analysis (1)] |
| 21. | Abu-Hamda EM, Baron TH, Simmons DT, Petersen BT. A retrospective comparison of outcomes using three different precut needle knife techniques for biliary cannulation. J Clin Gastroenterol. 2005;39:717-721. [PubMed] |
| 22. | Goff JS. Long-term experience with the transpancreatic sphincter pre-cut approach to biliary sphincterotomy. Gastrointest Endosc. 1999;50:642-645. [PubMed] |
| 23. | Catalano MF, Linder JD, Geenen JE. Endoscopic transpancreatic papillary septotomy for inaccessible obstructed bile ducts: Comparison with standard pre-cut papillotomy. Gastrointest Endosc. 2004;60:557-561. [PubMed] |
| 24. | Kahaleh M, Tokar J, Mullick T, Bickston SJ, Yeaton P. Prospective evaluation of pancreatic sphincterotomy as a precut technique for biliary cannulation. Clin Gastroenterol Hepatol. 2004;2:971-977. [PubMed] |
| 25. | Weber A, Roesch T, Pointner S, Born P, Neu B, Meining A, Schmid RM, Prinz C. Transpancreatic precut sphincterotomy for cannulation of inaccessible common bile duct: a safe and successful technique. Pancreas. 2008;36:187-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 34] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 26. | Smithline A, Silverman W, Rogers D, Nisi R, Wiersema M, Jamidar P, Hawes R, Lehman G. Effect of prophylactic main pancreatic duct stenting on the incidence of biliary endoscopic sphincterotomy-induced pancreatitis in high-risk patients. Gastrointest Endosc. 1993;39:652-657. [PubMed] |
| 27. | Tarnasky PR, Palesch YY, Cunningham JT, Mauldin PD, Cotton PB, Hawes RH. Pancreatic stenting prevents pancreatitis after biliary sphincterotomy in patients with sphincter of Oddi dysfunction. Gastroenterology. 1998;115:1518-1524. [PubMed] |
| 28. | Fazel A, Quadri A, Catalano MF, Meyerson SM, Geenen JE. Does a pancreatic duct stent prevent post-ERCP pancreatitis? A prospective randomized study. Gastrointest Endosc. 2003;57:291-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 210] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 29. | Singh P, Das A, Isenberg G, Wong RC, Sivak MV, Agrawal D, Chak A. Does prophylactic pancreatic stent placement reduce the risk of post-ERCP acute pancreatitis? A meta-analysis of controlled trials. Gastrointest Endosc. 2004;60:544-550. [PubMed] |
| 30. | Sofuni A, Maguchi H, Itoi T, Katanuma A, Hisai H, Niido T, Toyota M, Fujii T, Harada Y, Takada T. Prophylaxis of post-endoscopic retrograde cholangiopancreatography pancreatitis by an endoscopic pancreatic spontaneous dislodgement stent. Clin Gastroenterol Hepatol. 2007;5:1339-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 112] [Article Influence: 6.2] [Reference Citation Analysis (0)] |