Published online Aug 7, 2015. doi: 10.3748/wjg.v21.i29.8903
Peer-review started: December 16, 2014
First decision: January 22, 2015
Revised: March 13, 2015
Accepted: May 19, 2015
Article in press: May 19, 2015
Published online: August 7, 2015
Processing time: 237 Days and 22.7 Hours
AIM: To report the clinical outcomes and ergonomics analysis of three laparoscopic approaches in the management of Hirschsprung’s disease (HD).
METHODS: There were 90 pediatric patients (63 boys, 27 girls; mean age: 3.6 ± 2.7 mo; range: 1.0-90.2 mo) who underwent laparoscopic endorectal pull-through Soave procedures for short- and long-segment HD in our hospital. Three laparoscopic approaches were used: conventional laparoscopic pull-through (CLP) in 30 patients between 2009 and 2013, single-incision laparoscopic pull-through (SILP) in 28 patients between 2010 and 2013, and hybrid single-incision laparoscopic pull-through (H-SILP) in 32 patients between 2011 and 2013. We applied the hybrid version of the single-incision approach in 2011 to preserve the cosmetic advantage of SILP and the ergonomic advantage of CLP. We retrospectively analyzed the clinical data, cosmetic results, and ergonomics of these three approaches to have a better understanding of the selection of one approach over another.
RESULTS: The CLP, SILP, and H-SILP groups were similar in regard to age, sex, transition zone, blood loss, hospital stay, and intraoperative complications. Early and late postoperative results were not different, with equal daily defecation frequency and postoperative complications. No conversion to open technique was needed and none of the patients had recurrent constipation. With proper training, the ergonomics challenges were overcome and similar operative times were registered for the general operative time in the patients < 1 year of age and the short-segment HD patients. However, significantly shorter operative times were registered compared to SILP for patients > 1 year of age (CLP and H-SILP: 120 ± 15 min and 119 ± 12 min, respectively, vs 140 ± 7 min; P < 0.05) and for long-segment HD patients (152 ± 3.5 min and 154 ± 3.6 min, respectively, vs 176 ± 2.3 min; P < 0.05). The best cosmetic result was registered with the SILP (scarless), followed by the H-SILP (near scarless appearance) and the CLP (visible scars) procedures.
CONCLUSION: Based on the results, we believed that the laparoscopic approach should be selected according to the age, transition zone, and desired cosmetic result.
Core tip: This manuscript describes a comparison of the (1) hybrid single-incision laparoscopic endorectal pull-through, (2) conventional laparoscopic endorectal pull-through, and (3) single-incision laparoscopic endorectal pull-through in selected Hirschsprung’s disease patients. The cosmetic advantage was not the only concern, but also the age and transition zone-relating aspects of these three approaches. The clinical outcomes and ergonomics analysis are reported in order to better understand the choice of one approach over the other with regard to the patient’s age, transitional zone, and desired cosmetic result.
- Citation: Aubdoollah TH, Li K, Zhang X, Li S, Yang L, Lei HY, Dolo PR, Xiang XC, Cao GQ, Wang GB, Tang ST. Clinical outcomes and ergonomics analysis of three laparoscopic techniques for Hirschsprung's disease. World J Gastroenterol 2015; 21(29): 8903-8911
- URL: https://www.wjgnet.com/1007-9327/full/v21/i29/8903.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i29.8903
Hirschsprung’s disease (HD) is a well-known disease among pediatric surgeons; it is defined as a congenital abnormality of the enteric nervous system with the absence of ganglion cells in the distal parts of the colon resulting in a functional obstruction[1].
The laparoscopic technique has improved the surgical treatment of HD and has inspired surgeons to undertake more complex laparoscopic procedures to (1) promote early resumption of gastrointestinal function; (2) decrease complications; and (3) achieve better cosmetic results. Georgeson et al[2] described the conventional laparoscopic pull-through (CLP) procedure in 1995, and the single-incision laparoscopic pull-through (SILP) procedure was reported by Muensterer et al[3] in 2010. Since 1999, we have adopted the CLP procedure to treat various types of HD patients. In 2010, we started to perform SILP for cosmetic reasons, however, this procedure was challenging. In 2011, after accumulating a large amount of experience in CLP[4-6] and SILP[7], we applied the hybrid single-incision laparoscopic pull-through (H-SILP)[8], a combination of both procedures that preserves the cosmetic advantage of SILP and the ergonomic advantage of CLP.
This report describes the main three laparoscopic approaches that we have been using to treat HD with the same endorectal pull-through modified Boley-Soave procedure. The clinical outcomes and ergonomics analysis of the results are reported in order to better understand the choice of one approach over the other with regard to the patient’s age, transitional zone, and desired cosmetic result.
The clinical data of 90 cases (63 boys, 27 girls; mean age: 3.6 ± 2.7 mo, range: 1.0-90.2 mo) who underwent laparoscopic pull-through modified Soave procedures for short- and long-segment HD between 2009 and 2013 were retrospectively compared. Three laparoscopic approaches were used, including CLP in 30 patients between 2009 and 2013, SILP in 28 patients between 2010 and 2013, and H-SILP in 32 patients between 2011 and 2013.
The diagnosis was established in all the patients by rectal biopsy and anorectal manometry before the surgery[9,10]. Contrast barium enema[11] was performed to estimate the extent of the disease. The intraoperative frozen section biopsies and postoperative pathology reports confirmed the absence of ganglion cells and the transitional zone. Hematoxylin and eosin staining and calretinin and microtubule-associated protein-2 immunostaining were used to determine the presence or absence of the ganglion cells[12].
All these 90 patients underwent the same coloanal anastomosis. The transitional zone was located in the rectosigmoid (80 cases) and distal descending colon (10 cases). Patients who (1) required total or subtotal colectomy; (2) were treated by other procedures than the modified Boley-Soave procedure; and (3) were lost to follow-up or were previously operated in other hospitals were not included in this study. We also excluded three patients from the SILP group with long-segment HD (aged 22, 34, and 49 mo), because an additional working port was added to the right lower abdomen in order to retract the huge elongated colon for better exposure and to facilitate the dissection. Otherwise, it would have been very difficult to expose the vascular arcades of the descending colon and mobilize the splenic flexure. The operative time for the patients < 1 year (n = 63; infant) and > 1 year (n = 27; toddler, preschooler, and school-age) and the transitional zone of the three groups were compared to analyze the ergonomic impact or difficulties of the different laparoscopic approaches related to the age and transitional zone. None of the patients had a previous colostomy. Preoperatively, daily colon irrigations (mechanical bowel preparation) were performed for 2-7 d. Usually, intravenous antibiotics were started 1-2 d prior to operation and stopped 3 d after operation. Patients were reviewed on a monthly basis for 6 mo postoperatively, and then every 3-6 mo with mean follow-up 36 ± 10 mo (range: 17-53 mo).
All the procedures were performed under endotracheal general anesthesia. Cleaning and draping was performed for intraoperative change of position from the laparoscopic to transanal phase. Usually, the surgeon would position himself at the head or on the right of the table, facing the monitor, and the table was adjusted with the patient lying in a 30° head-down position.
In all the three groups of patients, the surgery was performed in two phases: (1) the laparoscopic phase; and (2) the transanal phase.
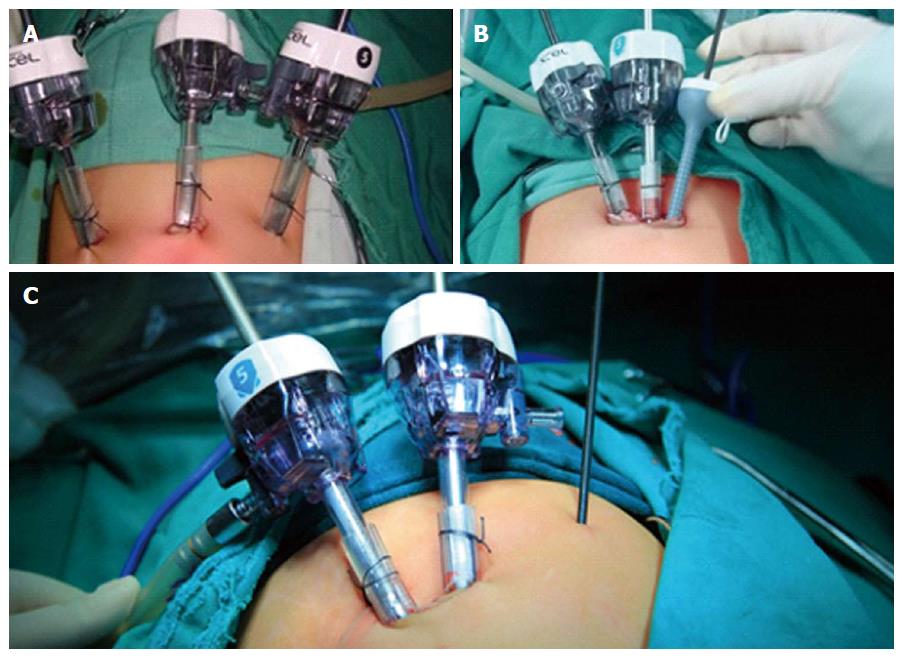
Laparoscopic phase: The CLP, SILP, and H-SILP procedures differ from each other with regard to the positioning of the trocars and instruments (Figure 1), but the objective remains the same. Usually, one assistant surgeon was needed for handling the 30° straight laparoscopic camera. No additional trocar was used.
In CLP, the first 5.0 mm trocar was introduced in the umbilicus via an umbilical skin incision as a laparoscope port. Under vision, after pneumoperitoneum was stabilized, two additional 5.0 mm trocars were introduced in the abdomen at the respective position: one on the left side and one on the right side (Figure 1A).
In SILP, the first 5.0 mm trocar was introduced in the umbilicus centrally via a single vertical umbilical skin incision as a laparoscope port, and pneumoperitoneum was stabilized. Lateral to the laparoscopic port, two additional trocars were introduced into the abdominal cavity as operator ports after the skin was stretched horizontally (one 5.0 mm trocar introduced on the right for an ultrasonic scalpel and one 3.0 mm trocar introduced on the left for a grasping forceps) (Figure 1B).
In H-SILP, two 5.0 mm trocars were introduced in the abdominal cavity via a vertical incision at the umbilicus. After pneumoperitoneum was stabilized, the left port was used as the laparoscope port and the right port was used as the working port for the ultrasonic scalpel or grasping forceps. A trocarless 3.0 mm grasping forceps was punctured in the abdomen via a stab incision, 10 cm to the left side of the umbilicus (Figure 1C).
After the insertion of the laparoscopic instruments, an overall view was obtained and the transition zone was located. One or two seromuscular biopsies were obtained for frozen section histology to identify the ganglionic bowel and to decide the dissecting level of the mesentery. Using the ultrasonic scalpel, a window was made in the sigmoid mesentery and the rectosigmoid colon was mobilized 5 cm above the transitional zone by dissecting the mesentery and relative vessels; however, the marginal arcade was preserved. The colonic pedicle was freed with sufficient length that it could be pulled through without tension or overstretching. The dissection was stopped at the rectal peritoneal reflection. After the laparoscopic dissection, the ports were left in situ, and we changed our position for the transanal phase. For long-segment HD patients, mobilization of the colon was performed to a higher level.
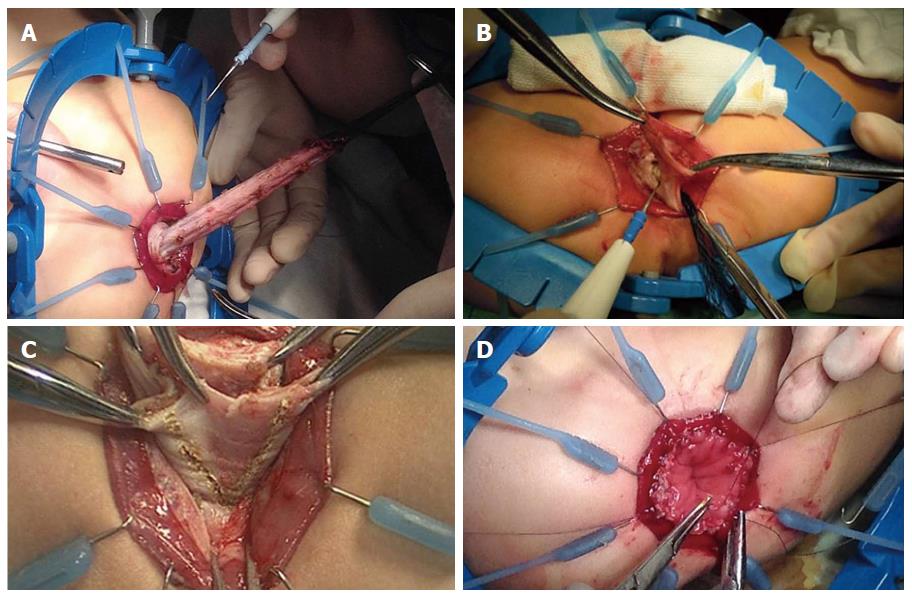
Transanal phase: All patients underwent the same modified Boley-Soave’s endorectal pull-through procedure[4-13]. This modified procedure consisted of: (1) lesser dissection in the pelvic cavity by the harmonic scalpel; (2) development of a long muscular rectal cuff for > 5 cm up to the peritoneal reflection by dissecting the submucosa layer of the rectum using electrocautery, which was then shortened to 2-3 cm; (3) partial resection of the rectal muscular cuff in a “V” shape at the posterior wall; and (4) resection of the necessary amount of the mobilized colon and coloanal anastomosis with the short cuff (Figure 2).
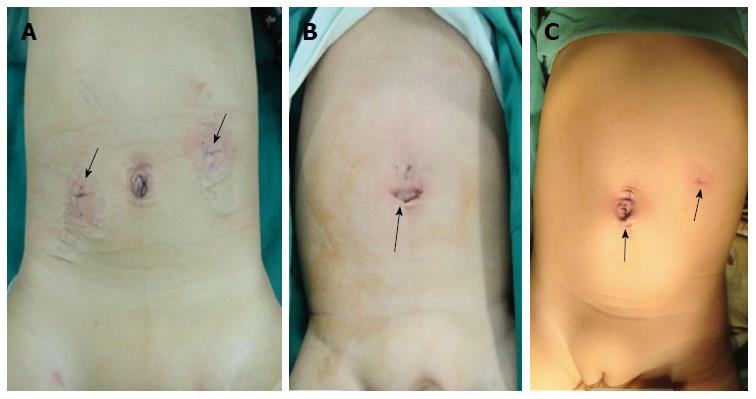
Once the anastomosis was completed, a rectal tube was inserted and laparoscopy was performed again to check for orientation of the pull-through bowel. Chitogel (15 mL of medical chitosan and physiologic-balanced solution) was injected at the dissection site via one of the ports to prevent peritoneal adhesion[14]. No abdominal drain was inserted. The port site at the umbilicus was stitched by 2-0 vicryl. The skin of the umbilicus and the other incisions were closed with skin glue. The postoperative appearance of the umbilicus and abdominal wound in the three groups were compared (Figure 3).
Postoperatively, patients were kept on intravenous total parenteral nutrition[15] and nasogastric decompression for 12-24 h. Intravenous antibiotics were given for 72 h and the urinary catheter was removed after 72 h. Patients were fed orally when bowel sounds returned. The parents were instructed on how to care for the wound and with regard to the toileting of the patients. The patients were discharged when they were clinically stable. Each patient was reviewed 2 wk after the operation, when a digital rectal examination was performed and anal dilatation[16,17] was taught to the parents, so that they could perform it at home with Hegar dilators once daily for 3-6 mo, until the dilatation process became easy and painless with the recommended dilator size.
The SPSS 13.0 software package (SPSS Inc., Chicago, IL, United States) was used for data analysis. The transition zone, age at surgery, operative time, estimated blood loss, intraoperative complications, conversion to open surgery, time of flatus passage, postoperative hospital stay, and defecation frequency were compared using analyses of variance. The sex and postoperative complications were compared using the χ2 test. The Student’s t test was used to compare the mean scar score between the CLP and the H-SILP groups. All the results are described as mean ± SD or as percentage. A P < 0.05 was considered as significant. The statistical methods of this study were reviewed by Prof. Ping Yin, PhD (Department of Epidemiology and Biostatistics School of Public Health Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430030, China.
The CLP, SILP, and H-SILP groups were similar in regard to age, sex, transition zone, blood loss, general operative time, hospital stay, and intraoperative complications (Table 1). Early and late postoperative results were not different, including equal daily defecation frequency and postoperative complications. There was no conversion to open technique. Postoperative enterocolitis occurred in two patients, one from the SILP (1/28; 3.6%) and the other from then H-SILP (1/32; 3.3%) group; both were treated by intravenous fluid, antibiotic, parenteral nutrition, and enemas during re-hospitalization. Anastomotic leak occurred in one case (1/30; 33.3%) from the CLP group and was treated conservatively with a rectal decompressing tube, intravenous antibiotics, and total parenteral nutrition to allow the leak to heal by itself. Perianal excoriation occurred in 26/90 (28.8%) patients (n = 7 SILP, n = 10 CLP, and n = 9 H-SILP), and was treated by keeping the perianal are clean and dry and with application of stomahesive. All the patients achieved normal defecation without incontinence or recurrent constipation with a mean of 3.0 mo to obtain normal defecation frequency (1-2 times/d).
| Characteristic | CLP (n = 30) | SILP (n = 28) | H-SILP (n = 32) | P value |
| Median age (mo) (range) | 3.8 ± 2.6 (1.0-90.2) | 3.4 ± 2.1 (1.0-78.8) | 3.6 ± 2.1 (1.0-78.6) | > 0.05 |
| Sex, male | 21 (70.0) | 18 (64.3) | 24 (75.0) | > 0.05 |
| General operative time (min) | 115 ± 22 (75-156) | 118 ± 22 (90-178) | 115 ± 24 (75-158) | > 0.05 |
| Conversion to open surgery | 0 | 0 | 0 | > 0.05 |
| Estimated blood loss (mL) | 5.0 ± 1.0 | 6.0 ± 1.5 | 4.5 ± 1.0 | > 0.05 |
| Hospital stays (d) | 7.0 ± 1.5 | 7.0 ± 1.0 | 7.0 ± 1.0 | > 0.05 |
| Intraoperative complications | 0 | 0 | 0 | > 0.05 |
| Time of passage of flatus (h) | 22.0 ± 5.0 | 21.5 ± 4.5 | 21.5 ± 4.0 | > 0.05 |
| Early postoperative complications | 11 (36.7) | 8 (33.3) | 8 (31.3) | > 0.05 |
| Perianal excoriation | 10 (33.3) | 7 (25.0) | 9 (28.1) | |
| Anastomotic leak | 1 (3.3) | 0 | 0 | |
| Enterocolitis | 0 | 1 (3.6) | 1 (3.1) | |
| Defecation frequency, times per day | ||||
| 1 wk postoperatively | 5 ± 4 | 6 ± 4 | 5 ± 4 | > 0.05 |
| 1 mo postoperatively | 4 ± 2 | 4 ± 3 | 4 ± 2 | > 0.05 |
| 3 mo postoperatively | 2 ± 1 | 2 ± 1 | 2 ± 1 | > 0.05 |
| Recurrent constipation | 0 | 0 | 0 | > 0.05 |
The operative times did not differ among the patients < 1 year of age, but were significantly shorter for CLP and H-SILP compared to SILP for patients > 1 year (P < 0.05) (Table 2). Similarly, the operative times among short-segment (rectosigmoid) HD patients did not differ, but were significantly shorter for CLP and H-SILP compared to SILP in long-segment (descending colon) HD patients (P < 0.05).
| Group | CLP(n = 30) | SILP(n = 28) | H-SILP(n = 32) |
| Patients < 1 yr of age, n | 21 | 20 | 22 |
| Operative time (min) | 113 ± 23 | 109 ± 8 | 113 ± 12 |
| Patients > 1 yr of age, n | 9 | 8 | 10 |
| Operative time | 120 ± 15a | 140 ± 7 | 119 ± 12a |
| Rectosigmoid colon, n | 27 | 26 | 27 |
| Operative time (min) | 111 ± 20 | 114 ± 17 | 109 ± 20 |
| Descending colon, n | 3 | 2 | 5 |
| Operative time (min) | 152 ± 4a | 176 ± 2 | 154 ± 4a |
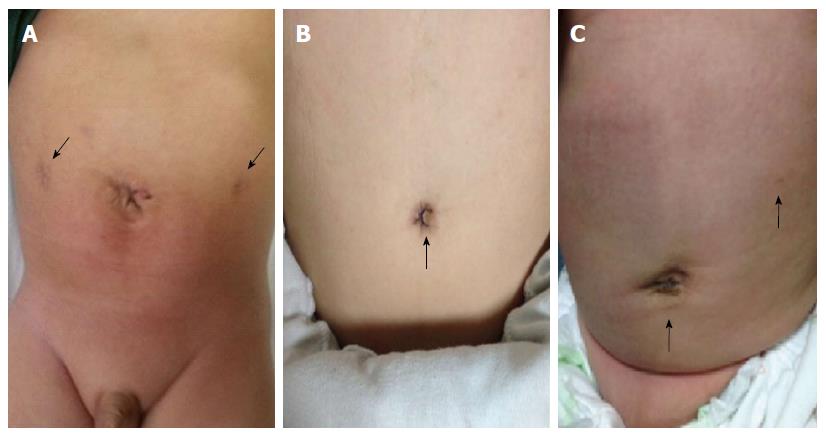
The wounds were healthy at hospital discharge and healed by 3 wk postoperatively. The cosmetic assessment was conducted 12 mo postoperatively (Table 3). The assessment of the abdomen revealed two visible scars in the CLP patients (Figure 4A), one barely remarkable/near scarless scar in an H-SILP (Figure 4C) patient and a scarless abdomen in the SILP patients (Figure 4B). The scar at the umbilicus was unremarkable, as it was embedded inside and the umbilicus appeared normal in all the patients. The Manchester Scar Scale[18,19] was used to assess the scar score only for the CLP and H-SILP patients, showing a significant difference between the two groups (P < 0.05) (Table 4). None of the patients suffered from wound infection or complications such as keloids or hypertrophied scars.
| Assessment | CLP(n = 30) | SILP(n = 28) | H-SILP(n = 32) | P value |
| Number of visible scars on the abdomen | 2 | 0 | 1 | - |
| Scar appearance on the abdomen | Visible | Scarless | Near scarless | - |
| MSS score of visible scar on the abdomen | 10.00 ± 0.72 (good) | - | 5.00 ± 0.72 (excellent) | < 0.05 |
| Appearance at the umbilicus | Normal | Normal | Normal | - |
| Category | Visual analog scale descriptor | Poor |
| Color | Perfect | 1 |
| Slight mismatch | 2 | |
| Obvious mismatch | 3 | |
| Gross mismatch | 4 | |
| Matte vs shiny | Matte | 1 |
| Shiny | 2 | |
| Contour | Flush with surrounding skin | 1 |
| Slightly proud/indented | 2 | |
| Hypertrophic | 3 | |
| Keloid | 4 | |
| Distortion | None | 1 |
| Mild | 2 | |
| Moderate | 3 | |
| Severe | 4 | |
| Texture | Normal | 1 |
| Just palpable | 2 | |
| Firm | 3 | |
| Hard | 4 |
The advancements in minimally invasive techniques have allowed HD to be treated quickly and safely with well-known benefits such as minimal surgical trauma, short operative time, and less postoperative pain[20], which lead to fast rehabilitation and avoidance of prolonged hospitalization. Many centers around the world have adopted the laparoscopic procedures as the standard procedure to treat HD, but the open approach is inevitable in case of laparoscopic failure[6].
More recently, in view of better cosmetic results and new laparoscopic procedures, De la Torre-Mondragón et al[21] described the transanal-endorectal pull-through technique, and Vahdad et al[22] described the totally transanal LESS pull-through colectomy. Both procedures are also relatively safe and feasible for short- and long-segment HD. However, besides the ergonomic disadvantages[23,24], the possibility of overstretching the anal sphincter and mesentery of rectosigmoid colon has been reported, which can increase the risk of fecal incontinence[3]. Similar to the single-incision laparoscopy[25-28], these minimally invasive procedures have excellent cosmetic results and are gaining in popularity.
As for any new technique, there was a learning curve for each of the procedures. In this study, there was no learning curve for the CLP, as a large amount of experience was accumulated by using the CLP[4-6] to treat HD patients. However, the training skill for the SILP procedure was acquired by training on a simulator[29,30] for at least 50 correct attempts before it was successfully applied in real practice. Initially, we had a prolonged operative time among the first five cases, but gradually decreased with the mean operating time to 118 ± 22 min (range: 90-178 min). After overcoming the difficulties encountered in the SILP, the learning curve was rather short for the H-SILP, where training on a simulator for at least ten correct attempts was sufficient because maneuverability was the same as the CLP. We believe that the general operative time did not differ among these procedures because of the proper training, which allowed us to overcome the challenges of the minimally invasive surgery.
With minimally invasive surgery, a man-machine environment is brought into the operating room, which creates mental and physical challenges for the operating team. The science of ergonomics analyzes these challenges and formulates guidelines for creating a work environment that is safe and comfortable for its operators while maintaining effectiveness and efficiency of the process[31]. The ergonomics analysis of the three procedures showed that the operating room, man power, and technical requirements were similar with an experienced operating team and the same coaxial alignments. The only difference in the three approaches was the positioning (Figure 1) of the working ports, which affected the ergonomics of the standard instruments[32]. In this study, curved instruments and a TriPort system were not considered as they are inappropriate for use younger children, especially newborns and infants[33,34].
As the SILP procedure was technically the most challenging, the following findings were observed besides the routine challenges of minimally invasive surgery. Optimum working angles are necessary for suturing and desired tissue manipulation. These working angles are directly influenced by the distance between the working ports. Ideally, good angles for working and suturing are acquired by placing the working ports 10 cm apart outside the body cavity, which provided a working distance of 4 cm inside the body cavity. In the SILP, the distance between the two working ports was approximately 4-5 cm outside the body cavity and the laparoscopic port was situated in the middle. In this context, the working angles were rather restricted and the manipulation was quite difficult.
Relative to the abdomen, each working port projects an internal and an external cone-shaped field, which limits our manipulations to a specific working field perimeter. In the SILP, the interception of these cone-shaped fields narrows the working area and eventually leads to internal and external clashing of the instruments and difficult manipulation. The operative field of vision is affected by the triangulation of the ports with the camera centrally placed. In the SILP, due to one site location of all the working ports, the field of the camera was narrowed, resulting in a restricted field of vision and often clashing of the camera with instruments manipulations (internally and externally). These problems were absent in the CLP and H-SILP, but SILP had the best cosmetic result.
The H-SILP is a “novel” modified version of the SILP. For ergonomic reasons, we shifted the left working port from the umbilical site to the left side the abdomen without trocar. Technically, the maneuverability of the instruments is much easier; similar to the CLP procedure, the working ports were 10 cm apart outside the body cavity, thus improving the triangulation, working angles, and working field. This provided better intra-abdominal exposure with greater in-line endoscope viewing, greater degrees of freedom, and minimal clashing of the instruments.
We used a trocarless instrument on the left side of the abdomen in the H-SILP to improve the cosmetic result and because there was no indication for interchange of instruments at that site. Although a 5.0 mm or 3.0 mm trocar is less traumatic to the surrounding skin tissue, it leaves a small, remarkable and shiny scar on the abdomen (Figure 4A) compared to a matte and nondistorted scar of a 3 mm trocarless instrument (Figure 4C). In this study, the SILP procedure had the best cosmetic result (scarless), followed by the H-SILP (near scarless appearance) and the CLP (two visible scars), and there was no significant change in the scar score during the entire follow-up period. The scar at the umbilicus was embedded inside, and the appearance was similar to a normal umbilicus, which favors the SILP[35]. The cosmetic result does play an important role in the life of a child, especially in terms of psychologic and psychosocial functioning[36,37].
Ergonomically, the CLP and the H-SILP have the same maneuverability and were less challenging than the SILP. However, with respect to the similar general operative times, we can say that the ergonomic challenges were overcome. Furthermore, to support this statement, the operative times for patients < 1 year of age and short-segment HD patients were not different. So, we can conclude that the SILP is as effective as the CLP and H-SILP. On the other hand, the operative times were significantly different for the patients > 1 year of age and for the patients with long-segment HD. So, we can conclude that the CLP and H-SILP are more convenient for patients > 1 year (toddler, preschool, and school-age patients) and for long-segment HD patients. The most possible reasons for the age and transitional zone ergonomic-related differences are: (1) children > 1 year have a thicker and larger abdominal wall than children < 1 year; (2) the mesenteries and organs are more developed (larger, thicker, and longer); (3) manipulations and dissections are performed at a deeper depth; and (4) for the long aganglionic segment, a longer length of the mesentery are dissected to mobilize the colon to a higher level.
In conclusion, all the procedures are feasible and safe with the same functional outcome. The laparoscopic approach should be selected according to the age, transition zone, and desired cosmetic result. The SILP is more suitable for short-segment HD in neonates and infants. The H-SILP is more convenient for patients > 1 year of age and long-segment HD patients. The CLP can be used in difficult cases where the SILP or the H-SILP might fail.
Hirschsprung’s disease (HD) is one of the diseases responsible for constipation in children. This article describes the main three laparoscopic approaches that the authors have been using to treat HD with the same endorectal, pull-through modified Soave procedure. The authors compared their outcomes and difficulties in order to better understand the choice of one approach over the other regarding patient age, transitional zone, and desired cosmetic result.
The laparoscopic technique has improved the surgical treatment of HD and has inspired surgeons to undertake more complex laparoscopic procedures to promote early resumption of gastrointestinal function, decrease complications, and to achieve better cosmetic results.
Since 1999, the authors have used a conventional laparoscopic procedure (CLP) to treat HD. In 2010, the authors applied the single-incision laparoscopic procedure (SILP). However, it was more challenging than CLP. In 2011, the authors applied the hybrid single-incision (H-SILP) to preserve the cosmetic advantage of the SILP and the ergonomic advantage of the CLP.
The authors found that the ergonomic challenges for the SILP procedure were overcome for a specific group of patients. So, with respect to age, transitional zone, and desired cosmetic results, the authors prefer to use: (1) SILP for short-segment HD in neonates and infants; (2) H-SILP for patients > 1 year and long-segment HD patients; and (3) CLP for difficult cases where the SILP or the H-SILP might fail.
The transitional zone is the boundary between the ganglionic and aganglionic segment of the colon. Surgically, it is very important to localize the specific affected segment of the colon for the proper amount of bowel resection and to reduce the risk of having to repeat the surgery for remnant aganglionic segments. Laparoscopic/endoscopic surgery is also known as minimally invasive surgery, where the surgeon uses a machine to operate on patients. Ergonomics is an applied scientific analysis of the interaction of man and machine in a specific environment.
This is a well-written paper with a well-performed analysis of three different approaches for the same disease, especially in different patients and those with different localization of the disease.
P- Reviewer: Agresta F, Dedemadi G, De Nardi P, Ryu DH S- Editor: Ma YJ L- Editor: AmEditor E- Editor: Wang CH
| 2. | Georgeson KE, Robertson DJ. Laparoscopic-assisted approaches for the definitive surgery for Hirschsprung’s disease. Semin Pediatr Surg. 2004;13:256-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 51] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Muensterer OJ, Chong A, Hansen EN, Georgeson KE. Single-incision laparoscopic endorectal pull-through (SILEP) for hirschsprung disease. J Gastrointest Surg. 2010;14:1950-1954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Tang ST, Wang GB, Cao GQ, Wang Y, Mao YZ, Li SW, Li S, Yang Y, Yang J, Yang L. 10 years of experience with laparoscopic-assisted endorectal Soave pull-through procedure for Hirschsprung’s disease in China. J Laparoendosc Adv Surg Tech A. 2012;22:280-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Tang ST, Cao ZQ, Ruan QL. A comparison between laparoscopic pull-through heart-shape coloproctectomy and open pull- through surgery in the treatment of Hirschsprung’s disease. Zhongguo Weichuang Waike Zazhi. 2005;5:699-701. |
| 6. | Tang ST, Wang GB, Ru QL. A comparison of laparoscopic-assisted pull-through with open approach for Hirschsprung‘s disease in infants and children. Zhongguo Weichuang Waike Zazhi. 2002;2:21-22. |
| 7. | Tang ST, Yang Y, Li SW, Cao GQ, Yang L, Huang X, Shuai L, Wang GB. Single-incision laparoscopic versus conventional laparoscopic endorectal pull-through for Hirschsprung’s disease: a comparison of short-term surgical results. J Pediatr Surg. 2013;48:1919-1923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Aubdoollah TH, Tang ST, Yang L, Li S, Lei HY, Zhang X. Hybrid Single-Incision Laparoscopic Approaches for Endorectal Pull-Through in Hirschsprung’s Disease. J Laparoendosc Adv Surg Tech A. 2015;25:595-598. [PubMed] |
| 9. | Kessmann J. Hirschsprung’s disease: diagnosis and management. Am Fam Physician. 2006;74:1319-1322. [PubMed] |
| 10. | de Lorijn F, Boeckxstaens GE, Benninga MA. Symptomatology, pathophysiology, diagnostic work-up, and treatment of Hirschsprung disease in infancy and childhood. Curr Gastroenterol Rep. 2007;9:245-253. [PubMed] |
| 11. | Yang WI, Oh JT. Calretinin and microtubule-associated protein-2 (MAP-2) immunohistochemistry in the diagnosis of Hirschsprung’s disease. J Pediatr Surg. 2013;48:2112-2117. [PubMed] |
| 12. | Pensabene L, Youssef NN, Griffiths JM, Di Lorenzo C. Colonic manometry in children with defecatory disorders. role in diagnosis and management. Am J Gastroenterol. 2003;98:1052-1057. [PubMed] |
| 13. | Yang L, Tang ST, Cao GQ, Yang Y, Li S, Li SW, Wang Y, Mao YZ, Ruan QL, Wang GB. Transanal endorectal pull-through for Hirschsprung’s disease using long cuff dissection and short V-shaped partially resected cuff anastomosis: early and late outcomes. Pediatr Surg Int. 2012;28:515-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Arung W, Meurisse M, Detry O. Pathophysiology and prevention of postoperative peritoneal adhesions. World J Gastroenterol. 2011;17:4545-4553. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 281] [Cited by in RCA: 308] [Article Influence: 22.0] [Reference Citation Analysis (4)] |
| 15. | Deleenheer B, Declercq P, Van Veer H, Nafteux P, Spriet I. Evaluation of parenteral nutrition use in patients undergoing major upper gastro-intestinal surgery. Int J Clin Pharm. 2015;37:579-582. [PubMed] |
| 16. | Aworanti O, Hung J, McDowell D, Martin I, Quinn F. Are routine dilatations necessary post pull-through surgery for Hirschsprung disease? Eur J Pediatr Surg. 2013;23:383-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Temple SJ, Shawyer A, Langer JC. Is daily dilatation by parents necessary after surgery for Hirschsprung disease and anorectal malformations? J Pediatr Surg. 2012;47:209-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Fearmonti R, Bond J, Erdmann D, Levinson H. A review of scar scales and scar measuring devices. Eplasty. 2010;10:e43. [PubMed] |
| 19. | Vercelli S, Ferriero G, Sartorio F, Stissi V, Franchignoni F. How to assess postsurgical scars: a review of outcome measures. Disabil Rehabil. 2009;31:2055-2063. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 20. | Nguyen NT, Lee SL, Goldman C, Fleming N, Arango A, McFall R, Wolfe BM. Comparison of pulmonary function and postoperative pain after laparoscopic versus open gastric bypass: a randomized trial. J Am Coll Surg. 2001;192:469-476; discussion 476-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 127] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 21. | De la Torre-Mondragón L, Ortega-Salgado JA. Transanal endorectal pull-through for Hirschsprung’s disease. J Pediatr Surg. 1998;33:1283-1286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 233] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 22. | Vahdad MR, Foroutan A, Najafi SM, Cernaianu G, Tröbs RB, Banani SA, Foroutan HR. Totally transanal LESS pull-through colectomy: a novel approach for avoiding abdominal wall incision in children with long-segment intestinal aganglionosis. J Laparoendosc Adv Surg Tech A. 2013;23:276-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 23. | Gobran TA, Ezzat A, Hassan ME, O’Neill J. Redo transanal endorectal pull-through: a preliminary study. Pediatr Surg Int. 2007;23:189-193. [PubMed] |
| 24. | Hansen EN, Muensterer OJ, Georgeson KE, Harmon CM. Single-incision pediatric endosurgery: lessons learned from our first 224 laparoendoscopic single-site procedures in children. Pediatr Surg Int. 2011;27:643-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 59] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 25. | Rothenberg SS, Shipman K, Yoder S. Experience with modified single-port laparoscopic procedures in children. J Laparoendosc Adv Surg Tech A. 2009;19:695-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 87] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 26. | Muensterer OJ, Adibe OO, Harmon CM, Chong A, Hansen EN, Bartle D, Georgeson KE. Single-incision laparoscopic pyloromyotomy: initial experience. Surg Endosc. 2010;24:1589-1593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Tam YH, Lee KH, Sihoe JD, Chan KW, Cheung ST, Pang KK. Initial experience in children using conventional laparoscopic instruments in single-incision laparoscopic surgery. J Pediatr Surg. 2010;45:2381-2385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 62] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 28. | Tugcu V, Ilbey YO, Polat H, Tasci AI. Early experience with laparoendoscopic single-site pyeloplasty in children. J Pediatr Urol. 2011;7:187-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 29. | Gallagher AG, Ritter EM, Champion H, Higgins G, Fried MP, Moses G, Smith CD, Satava RM. Virtual reality simulation for the operating room: proficiency-based training as a paradigm shift in surgical skills training. Ann Surg. 2005;241:364-372. [PubMed] |
| 30. | Frigenza M, Tran A, Breaud J, Fournier JP, Bongain A, Delotte J. Evaluation of single incision laparoscopic surgery “low-fidelity” simulation training. J Visc Surg. 2014;151:335-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | van Det MJ, Meijerink WJ, Hoff C, Totté ER, Pierie JP. Optimal ergonomics for laparoscopic surgery in minimally invasive surgery suites: a review and guidelines. Surg Endosc. 2009;23:1279-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 143] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 32. | Saxena AK, Hollwarth ME, editors . Essentials of Pediatric Endoscopic Surgery. Berlin and Heidelberg: Springer-Verlag, GmbH & Co. K 2008; 47-50. |
| 33. | Garey CL, Laituri CA, Ostlie DJ, St Peter SD. A review of single site minimally invasive surgery in infants and children. Pediatr Surg Int. 2010;26:451-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 34. | Chambers WM, Bicsak M, Lamparelli M, Dixon AR. Single-incision laparoscopic surgery (SILS) in complex colorectal surgery: a technique offering potential and not just cosmesis. Colorectal Dis. 2011;13:393-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 115] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 35. | Ostlie DJ, Sharp NE, Thomas P, Sharp SW, Holcomb GW, St Peter SD. Patient scar assessment after single-incision versus four-port laparoscopic cholecystectomy: long-term follow-up from a prospective randomized trial. J Laparoendosc Adv Surg Tech A. 2013;23:553-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 36. | Maskell J, Newcombe P, Martin G, Kimble R. Psychological and psychosocial functioning of children with burn scarring using cosmetic camouflage: a multi-centre prospective randomised controlled trial. Burns. 2014;40:135-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Sowislo JF, Orth U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychol Bull. 2013;139:213-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 957] [Cited by in RCA: 1060] [Article Influence: 81.5] [Reference Citation Analysis (0)] |