Published online Jun 28, 2015. doi: 10.3748/wjg.v21.i24.7594
Peer-review started: December 8, 2014
First decision: December 26, 2014
Revised: January 8, 2015
Accepted: March 18, 2015
Article in press: March 19, 2015
Published online: June 28, 2015
Processing time: 204 Days and 3.9 Hours
We report a case of biliary drainage for malignant stricture using a metal stent with an ultrathin endoscope through the gastric stoma. A 78-year-old female was referred to our hospital for jaundice and fever. She had undergone percutaneous endoscopic gastrostomy (PEG) for esophageal obstruction after radiation therapy for cancer of the pharynx. Abdominal contrast-enhanced computed tomography showed a 3-cm enhanced mass in the middle bile duct and dilatation of the intra-hepatic bile duct. We initially performed endoscopic retrograde cholangiopancreatography (ERCP) with a trans-oral approach. However, neither the side-viewing endoscope nor the ultrathin endoscope passed through the esophageal orifice. Thus, we eventually performed ERCP via the PEG stoma using an ultrathin endoscope. We performed biliary drainage with a 6F introducer self-expanding metal stent. The cytology findings obtained by brush cytology showed malignancy. Her laboratory results were restored to normal levels after drainage and no complication occurred.
Core tip: The method of transgastrostomic endoscopy using an ultrathin endoscope has been reported in terms of its safety and various advantages. A 6F delivery system uncovered-type self-expanding metal stent (SEMS) has been developed, and this SEMS is able to pass through an endoscopic working channel at least 2.0 mm in diameter. To our knowledge, this is the first reported evaluation of the performance of biliary drainage for malignant stricture using a 6F introducer SEMS with an ultrathin endoscope through the percutaneous endoscopic gastrostomy stoma.
- Citation: Matsumoto K, Kato H, Tsutsumi K, Akimoto Y, Uchida D, Tomoda T, Yamamoto N, Noma Y, Horiguchi S, Okada H, Yamamoto K. Successful biliary drainage using a metal stent through the gastric stoma. World J Gastroenterol 2015; 21(24): 7594-7597
- URL: https://www.wjgnet.com/1007-9327/full/v21/i24/7594.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i24.7594
A trans-oral or trans-nasal approach is essential for the performance of endoscopic retrograde cholangiopancreatography (ERCP), although difficulties are often encountered in complicated cases when both approaches are problematic; for instance, in patients who have suffered a cerebrovascular accident or a head-and-neck cancer. In such patients percutaneous endoscopic gastrostomy (PEG) is frequently carried out. PEG is a procedure that Ponsky and Gauderer developed in order to provide direct access to the lumen of the stomach[1]. PEG has become the preferred method of providing long-term enteral nutrition and some patients have prolonged survival after PEG placement[2].
Endoscopy with an ultrathin endoscope was developed for various gastrointestinal conditions, and its benefits have been demonstrated in various situations[3,4]. Recently, several procedures for transgastrostomic endoscopy (TGE) using an ultrathin endoscope have been reported, demonstrating its tolerability and benefits[5-7]. Moreover, diagnostic and therapeutic ERCP through the gastrostomy tract using an ultrathin endoscope for patients with benign biliary disease has been reported[7].
Here, we present the first reported case of biliary drainage for malignant stricture using a metal stent with an ultrathin endoscope through the gastric stoma.
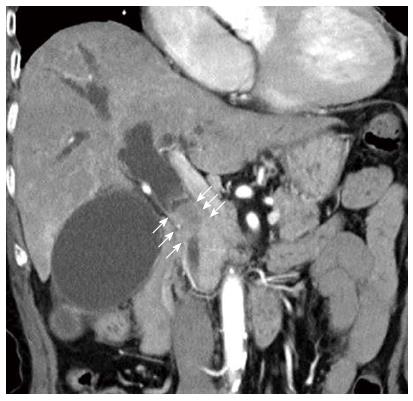
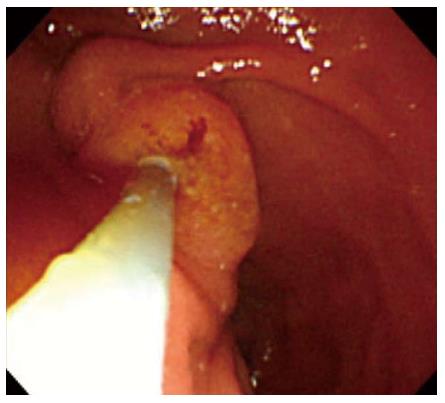
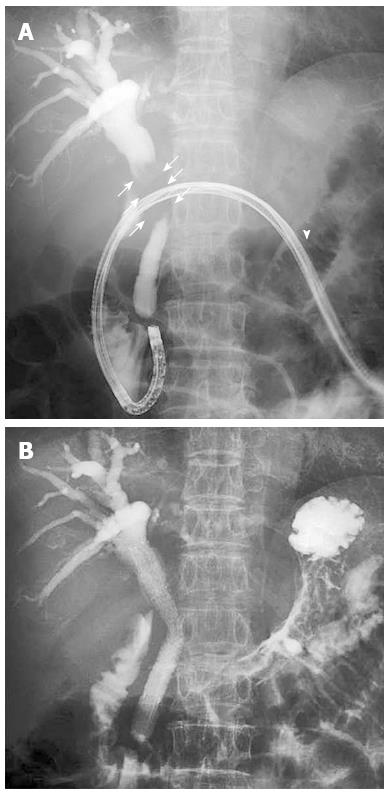
A 78-year-old female was referred to our hospital for jaundice and fever, and liver enzymes revealed an obstructive pattern with a serum level of total bilirubin 11.5 mg/dL (normal range: 0.33-1.28 mg/dL). She had been suffering from cancer of the pharynx for the past 6 years. She had undergone PEG for esophageal obstruction after radiation therapy for pharyngeal cancer. Abdominal contrast-enhanced computed tomography showed a 3-cm enhanced mass in the middle bile duct and dilatation of the intra-hepatic bile duct (Figure 1). We initially performed ERCP with a trans-oral approach using a side-viewing endoscope (JF-260V, 12.6 mm in diameter; Olympus, Tokyo, Japan). However, the scope could not pass through the esophageal orifice. Next, we used an ultrathin endoscope (EG-530NW 5.9 mm in diameter, Fujifilm, Tokyo, Japan) with the same approach; however, the scope could not pass. Thus, we eventually performed ERCP via the PEG stoma using an ultrathin endoscope. Cholangiography showed a 3-cm-long irregular stricture in the middle bile duct, and we suspected bile duct cancer (Figures 2 and 3A). We performed brush cytology (BC-24Q, Olympus, Tokyo, Japan) at the stricture and biliary drainage with a 6F introducer self-expanding metal stent (SEMS) (Zilver 635; 10 × 80 mm, Cook Medical Systems, Winston-Salem, NC)[8], which can pass through the 2.0-mm working channel of the ultrathin endoscope. We were able to place it successfully into the middle bile duct (Figure 3B). The cytology findings showed malignancy; however, she was ineligible for invasive surgery because of her advanced age. Her laboratory results were restored to normal levels after drainage and no complication occurred.
In a recent study, Choi et al reported the result of ERCP through a gastric stoma using a duodenal scope in patients with prior Roux-en-Y gastric bypass[8]. In their report of 44 patients undergoing 76 procedures, the technical therapeutic success rate was 97% (74/76) and ERCP-related complication rate was 1.3% (1/76). However, the gastrostomy-related complication rate was 13.2% (10/76). They concluded the procedure was hindered by the gastrostomy maturation delay and a higher morbidity.
Recently, the method of TGE using an ultrathin endoscope has been reported in terms of its safety and various advantages[5,6]. Mori et al[7] reported two cases of ERCP through a gastric stoma using an ultrathin endoscope (EG530N5; Fujifilm, Tokyo, Japan). In their report, one case was diagnostic ERCP, in which only cholangiography was performed, and the other case was therapeutic ERCP, in which biliary drainage with placement of a plastic stent in the common bile duct was performed. In both cases there was no difficulty identifying the papilla of Vater or in cannulation of the bile duct using the conventional ERCP tube through the biopsy channel (Figure 2). No significant complications were encountered. In our case, we could cannulate the bile duct using the conventional tube at the inversed scope position, and perform biliary drainage for malignant obstruction with SEMS using the ultrathin endoscope. In addition, no complications were encountered including cardiopulmonary damage or post-procedural hyperamylasemia.
The mortality of patients undergoing PEG appears to be high. Excluding patients with malignant disease, the survival rate has been about 53% at 6 months and 38% at 1 year, with pneumonia being the most common cause of death[2]. However, patients who have undergone PEG due to upper gastrointestinal obstruction caused by benign or curable cancer are able to have a long survival[9]. Although our patient had been suffering from cancer of the pharynx for the previous 6 years, it had become under remission due to radiation therapy. Our patient will survive for longer and has good performance status. Thus, we chose internal biliary drainage rather than external drainage.
A 6F delivery system uncovered-type SEMS has been developed for intended side-by-side bilateral deployment in hilar malignant obstruction[10]. This SEMS is able to pass through an endoscopic working channel at least 2.0 mm in diameter. To our knowledge, this is the first reported evaluation of the performance of biliary drainage for malignant stricture using a 6F introducer SEMS with an ultrathin endoscope through the PEG stoma. The patency of SEMS is longer than that with a plastic stent[11]. Thus, this case was suitable for drainage with SEMS. Currently, to the best of our knowledge, there is no covered metallic stent with 6F delivery system. We consider uncovered metallic stents such as Zilver635 are more suitable than covered metallic stents for an endoscope with a small working channel because of the thinner delivery of uncovered metallic stents. We conclude that this drainage method using a 6F introducer SEMS with an ultrathin endoscope is useful and safe for patients with a gastric stoma.
A 78-year-old female who had jaundice and fever, with a history of cancer of the pharynx.
The physical signs of this case were jaundice and fever. She had undergone percutaneous endoscopic gastrostomy (PEG) at the upper middle of abdomen for esophageal obstruction after radiation therapy for pharyngeal cancer.
Common bile duct stone, gallbladder stone (Mirizzi syndrome), acute hepatitis.
Liver enzymes revealed an obstructive pattern with a serum level of total bilirubin 11.5 mg/dL.
Abdominal contrast-enhanced computed tomography showed a 3-cm enhanced mass in the middle bile duct and dilatation of the intra-hepatic bile duct.
The cytology findings obtained by endoscopic retrograde cholangiopancreatography (ERCP) showed malignancy.
The patient underwent biliary drainage with a 6F introducer self-expanding metal stent (SEMS) using an ultrathin endoscope.
Several procedures for transgastrostomic endoscopy using an ultrathin endoscope have been reported. Moreover, diagnostic and therapeutic ERCP through the gastrostomy tract using an ultrathin endoscope for patients with benign biliary disease has been reported.
A 6F delivery system uncovered-type SEMS (Zilver 635; 10×80mm, Cook Medical Systems, Winston-Salem, NC, United States) has been developed for intended side-by-side bilateral deployment in hilar malignant obstruction. This SEMS is able to pass through an endoscopic working channel at least 2.0 mm in diameter.
This case report presents the performance of biliary drainage for malignant stricture using a 6F introducer SEMS with an ultrathin endoscope through the PEG stoma.
This is a report that a drainage method using a 6F introducer SEMS with an ultrathin endoscope is useful and safe for patients with a gastric stoma.
P- Reviewer: Erdogan A, Krishna SG S- Editor: Yu J L- Editor: Logan S E- Editor: Zhang DN
| 1. | Ponsky JL, Gauderer MW. Percutaneous endoscopic gastrostomy: a nonoperative technique for feeding gastrostomy. Gastrointest Endosc. 1981;27:9-11. [PubMed] |
| 2. | Tokunaga T, Kubo T, Ryan S, Tomizawa M, Yoshida S, Takagi K, Furui K, Gotoh T. Long-term outcome after placement of a percutaneous endoscopic gastrostomy tube. Geriatr Gerontol Int. 2008;8:19-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Itoi T, Kawai T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Takeuchi M. Initial experience of transnasal endoscopic biliary drainage without conscious sedation for the treatment of acute cholangitis (with video). Gastrointest Endosc. 2008;67:328-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Trevisani L, Cifalà V, Sartori S, Gilli G, Matarese G, Abbasciano V. Unsedated ultrathin upper endoscopy is better than conventional endoscopy in routine outpatient gastroenterology practice: a randomized trial. World J Gastroenterol. 2007;13:906-911. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 50] [Cited by in RCA: 52] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Imaeda H, Hosoe N, Nakamizo H, Kashiwagi K, Suzuki H, Saito Y, Suganuma K, Ida Y, Matsuzaki J, Iwasaki E. Clinical results of observation of the upper gastrointestinal tract by transgastrostomic endoscopy using an ultrathin endoscope. J Gastroenterol Hepatol. 2010;25:1850-1854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Adler DG, Gostout CJ, Baron TH. Percutaneous transgastric placement of jejunal feeding tubes with an ultrathin endoscope. Gastrointest Endosc. 2002;55:106-110. [PubMed] |
| 7. | Mori A, Ohashi N, Maruyama T, Tatebe H, Sakai K, Inoue H, Takegoshi S, Okuno M. Endoscopic retrograde cholangiopancreatography through a gastric stoma using an ultrathin endoscope: a novel approach. Endoscopy. 2007;39 Suppl 1:E323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Choi EK, Chiorean MV, Coté GA, El Hajj II, Ballard D, Fogel EL, Watkins JL, McHenry L, Sherman S, Lehman GA. ERCP via gastrostomy vs. double balloon enteroscopy in patients with prior bariatric Roux-en-Y gastric bypass surgery. Surg Endosc. 2013;27:2894-2899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 9. | Rimon E, Kagansky N, Levy S. Percutaneous endoscopic gastrostomy; evidence of different prognosis in various patient subgroups. Age Ageing. 2005;34:353-357. [PubMed] |
| 10. | Chennat J, Waxman I. Initial performance profile of a new 6F self-expanding metal stent for palliation of malignant hilar biliary obstruction. Gastrointest Endosc. 2010;72:632-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 11. | Elwir S, Sharzehi K, Veith J, Moyer MT, Dye C, McGarrity T, Mathew A. Biliary stenting in patients with malignant biliary obstruction: comparison of double layer, plastic and metal stents. Dig Dis Sci. 2013;58:2088-2092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |