Published online Apr 28, 2015. doi: 10.3748/wjg.v21.i16.5105
Peer-review started: September 26, 2014
First decision: October 14, 2014
Revised: November 20, 2014
Accepted: January 16, 2015
Article in press: January 16, 2015
Published online: April 28, 2015
Processing time: 217 Days and 24 Hours
Nonconvulsive status epilepticus has become an important issue in modern neurology and epileptology. This is based on difficulty in definitively elucidating the condition and its various clinical phenomena and on our inadequate insight into the intrinsic pathophysiological processes. Despite nonconvulsive status epilepticus being a situation that requires immediate treatment, this disorder may not be appreciated as the cause of mental status impairment. Although the pathophysiology of nonconvulsive status epilepticus remains unknown, this disorder is thought to lead to neuronal damage, so its identification and treatment are important. Nonconvulsive status epilepticus should be considered in the differential diagnosis of patients with liver cirrhosis presenting an altered mental status. We report a case of a 52-year-old male with liver cirrhosis presenting an altered mental status. He was initially diagnosed with hepatic encephalopathy but ultimately diagnosed with nonconvulsive status epilepticus by electroencephalogram.
Core tip: This case highlights the probability of nonconvulsive status epilepticus in patient with liver cirrhosis and the utility of electroencephalogram to evaluate for patient with liver cirrhosis who presents an altered mental status. It is important to consider the possibility of nonconvulsive status epilepticus, evaluating for patient with liver cirrhosis who presents with an altered mental status, especially who do not respond to empirical treatment.
- Citation: Jo YM, Lee SW, Han SY, Baek YH, Ahn JH, Choi WJ, Lee JY, Kim SH, Yoon BA. Nonconvulsive status epilepticus disguising as hepatic encephalopathy. World J Gastroenterol 2015; 21(16): 5105-5109
- URL: https://www.wjgnet.com/1007-9327/full/v21/i16/5105.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i16.5105
Hepatic encephalopathy is defined as a reversible disturbance in central nervous system function that is observed in patients with chronic or acute liver failure. This complex neuropsychiatric disorder is mainly caused by biochemical disturbance and is a commonly diagnosed and well-recognized disorder that has been studied for many years. However, this disorder still continues to be a primary clinical problem and should be considered in any patient with liver cirrhosis who has neuropsychiatric symptoms but no brain abnormalities. Treatment depends on immediate awareness of the precipitating factors and initiation of empirical treatment.
Status epilepticus is a life-threatening condition involving constant seizures. This disorder is a well-recognized medical emergency requiring immediate treatment to prevent morbidity and mortality. However, nonconvulsive status epilepticus may not be recognized as the cause of a mental status change without obvious convulsions, so treatment can be delayed. This underdiagnosis may lead to injurious results. Nonconvulsive status epilepticus, such as the easily recognized convulsive status epilepticus, is a fatal condition requiring immediate treatment. It is often difficult to make a diagnosis, as many other conditions can cause an altered mental status in patients with liver cirrhosis.
It is important to understand the possibility of nonconvulsive status epilepticus being disguised as hepatic encephalopathy, especially when evaluating a patient with liver cirrhosis who presents an altered mental status.
Herein, we report the case of a patient with a high clinical suspicion of hepatic encephalopathy who was ultimately diagnosed as having nonconvulsive status epilepticus. To the best of our knowledge, this is the first reported case of such a presentation in Korea.
A 52-year-old man with liver cirrhosis secondary to hepatitis B and a 2 cm-sized hepatocellular carcinoma in the S4 segment of the liver was brought into the emergency department by ambulance for a confused and lethargic mental status.
On arrival, the patient had a blood pressure of 130/80 mmHg, a pulse of 65 beats per minute, a temperature of 36.5 °C, a respiratory rate of 20 breaths per minute, and oxygen saturation of 97% in room air. The patient did not have a history of hepatic encephalopathy. Additionally, the patient did not have a history of seizures, brain trauma or other brain diseases.
Physical examination revealed hepatosplenomegaly with ascites. The patient’s Glasgow Coma Scale score was 11 (eyes, 3; verbal, 4; motor, 4). There were no signs of traumatic injury anywhere on his body. His pupils were equally round and reactive to light, and his neck was soft, without the Brudzinski sign. Cardiopulmonary and abdominal examinations were unremarkable. The patient could move all extremities equally but showed shaking in both hands. The Babinski sign was normal in both feet.
Chest radiography did not reveal any pathologic lesion. Laboratory tests revealed a white blood cell count of 4830/mm3, with 64% neutrophils, hemoglobin of 14.4 g/dL, hematocrit of 39.8%, and platelets at 77000/mm3. The electrolyte and liver function test results are as follows: sodium, 137 mmol/L; potassium, 3.9 mmol/L; chloride, 105 mmol/L; bicarbonate, 21 mEq/L; calcium, 8.3 mg/dL; blood urea nitrogen, 11 mg/dL; creatinine, 1.0 mg/dL; total bilirubin, 3.7 mg/dL; aspartate aminotransferase, 86 IU/L; alanine aminotransferase 22 IU/L; alkaline phosphatase, 374 IU/L; albumin, 3.5 g/dL; lipase, 56 IU/L; prothrombin time (INR), 1.33; and ammonia, 88 μmol/L (reference range, 10-47 μmol/L). The random blood glucose level was 92 mg/dL. The arterial blood gas was pH 7.45.
According to the history and the laboratory data, hepatic encephalopathy grade III was suspected. Rifaximin 400 mg was administered to the patient via a nasogastric tube every eight hours, and lactulose 30 mL was administered via a nasogastric tube every six hours to induce three to four bowel movements daily. Despite the patient immediately improving neurologically during the emergency department stay, with a Glasgow Coma Scale score of 15 (eyes, 4; verbal, 5; motor, 6), physical examination still showed shaking in both hands, even when the ammonia levels had decreased to 63 μmol/L.
The patient was admitted to the general ward. Administration of empirical antibiotics was initiated in the emergency department but was interrupted because an infectious etiology was not demonstrated and because the culture results were negative.
On the second day of his hospitalization, the patient suddenly entered a stupor, could not respond to simple commands and showed a decerebrate response to painful stimuli. At that time, his Glasgow Coma Scale score was 4 (eyes, 1; verbal, 1; motor, 2), and his ammonia levels had increased to 112 μmol/L.
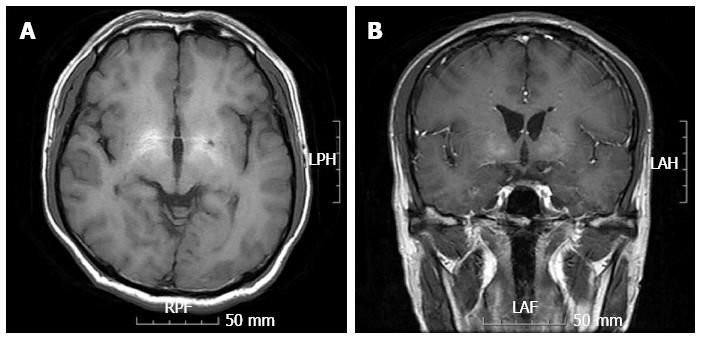
Despite continuation of empirical treatment for hepatic encephalopathy, the mental status of the patient remained comatose. A neurologist was consulted. The results of a magnetic resonance imaging brain scan exhibited symmetrical high-signal abnormalities in the basal ganglia on T1-weighted images (Figure 1).
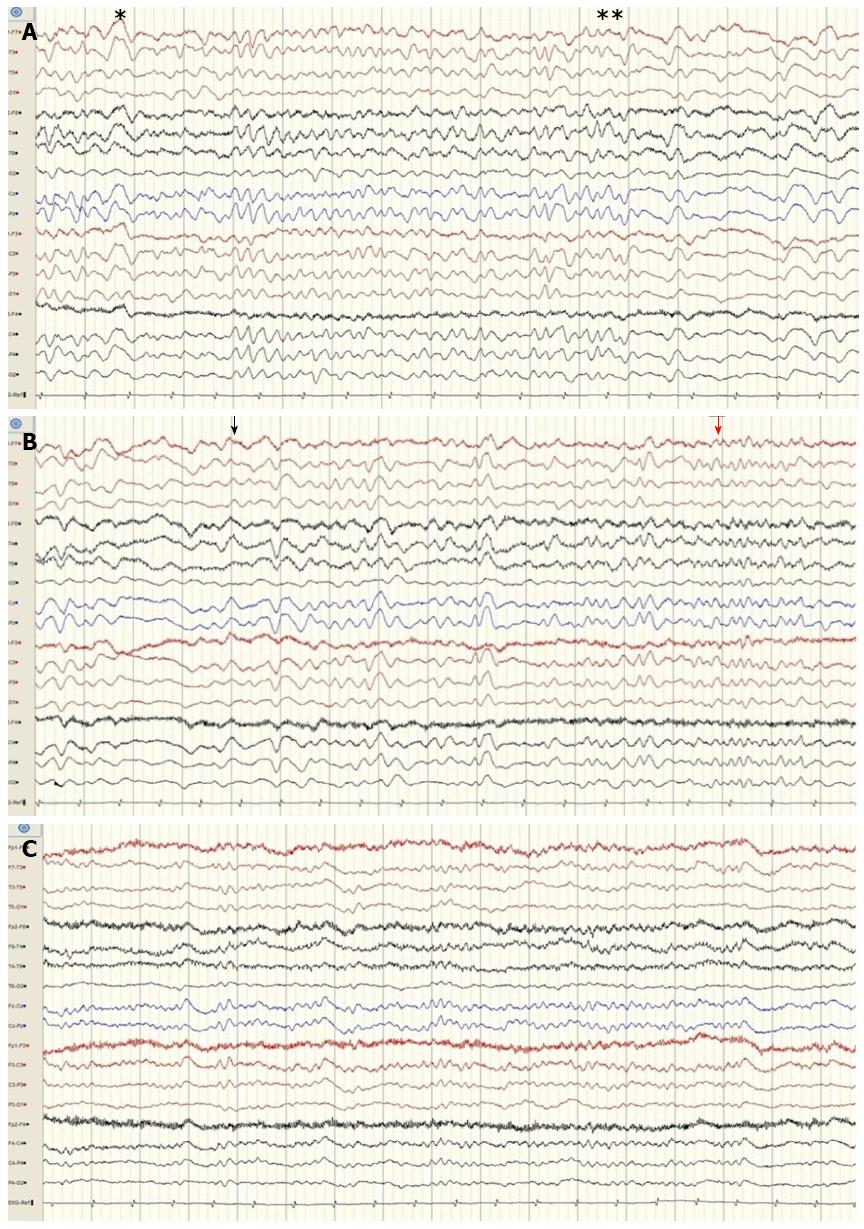
An electroencephalogram revealed generalized sequential rhythmic delta to theta activity, with decreasing termination and increasing onset (Figure 2A). After administration of intravenous lorazepam 4 mg, the electroencephalogram showed that the epileptiform discharge had resolved (Figure 2B and C). Because the patient had no obvious convulsions, he was diagnosed with nonconvulsive status epilepticus according to Young’s criteria for electrographic status epilepticus. Levetiracetam was administered, ultimately leading to resolution of status epilepticus, as revealed by an electroencephalogram. Despite the patient being treated with levetiracetam for 4 d, he did not improve neurologically. He was transferred to another facility for constant treatment at the family’s request. Unfortunately, the patient expired five days after the transfer because of multiple organ dysfunction, including hepatorenal syndrome.
Hepatic encephalopathy is often diagnosed when a patient with liver cirrhosis presents an altered mental status. The symptoms of hepatic encephalopathy generally include personality changes, poor concentration, poor judgment, disorientation and confusion[1]. Although not clearly defined, the common pathophysiological hallmark of the disorder is a synergic interaction between high ammonemia and an inflammatory response, causing astrocyte swelling and ultimately cerebral edema. Additionally, diverse metabolic components may be involved, including short-chain fatty acids, mercaptans, phenols, and false neurotransmitters[2]. An electroencephalogram can be a useful diagnostic tool for hepatic encephalopathy. Electroencephalographic findings in hepatic encephalopathy show high-amplitude, low-frequency waves and triphasic waves. Hyperammonemia has been well investigated as a contributing factor to triphasic waves on electroencephalogram in hepatic encephalopathy[3-5].
Nonconvulsive status epilepticus is a clinical disorder defined as prolonged seizure activity without major motor signs for at least 30 min. Nonconvulsive status epilepticus can be difficult to diagnose because of the absence of overt convulsive activity[6].
Despite the lack of convulsive activity, this disorder is thought to result in neuronal damage, so awareness about it and treatment are critical[7]. This disorder should be treated rapidly to prevent serious neuronal damage. In intensive care units, nonconvulsive status epilepticus may be provoked by diverse conditions, such as infections, sleep deprivation, severe electrolyte imbalance, toxic or metabolic disturbances, antiepileptic drug or alcohol withdrawal and acute or remote structural brain injury[5,8]. Because nonconvulsive status epilepticus cannot be easily distinguished from other, similar conditions, diagnosis and awareness of the precipitating factors is important[9].
The present case involved a patient with a high clinical suspicion of hepatic encephalopathy who was ultimately diagnosed with nonconvulsive status epilepticus. The patient was initially diagnosed with hepatic encephalopathy grade III. Empirical treatment of hepatic encephalopathy was initiated, but the condition did not ultimately improve. The clinical features, the results of a magnetic resonance imaging brain scan and an electroencephalogram were suggestive of nonconvulsive status epilepticus on the basis of Young’s criteria for electrographic status epilepticus.
Reports of nonconvulsive status epilepticus in patients with liver cirrhosis are very rare. Additionally, the pathophysiology of nonconvulsive status epilepticus in patients with liver cirrhosis remains unknown. Various metabolic factors may be suggested as the cause. Plasma ammonium levels are consistently elevated, and other factors, such as short-chain free fatty acids, phenols, mercaptans and false neurotransmitters, have also been implicated.
This case emphasizes the reality of nonconvulsive status epilepticus in patients with liver cirrhosis and the utility of an electroencephalogram to evaluate the patient with liver cirrhosis who presents an altered level of consciousness. It is important to consider the possibility of nonconvulsive status epilepticus, evaluating the patient with liver cirrhosis who presents with an altered mental status, and especially the patient who does not respond to empirical treatment. An emergent electroencephalogram can be useful in the evaluation of patients with hepatic encephalopathy who have alterations in their level of consciousness.
A 52-year-old man with liver cirrhosis secondary to hepatitis B and a 2 cm-sized hepatocellular carcinoma in the S4 segment of the liver was brought into the emergency department by ambulance for a confused and lethargic mental status.
He was diagnosed with nonconvulsive status epilepticus on the basis of Young’s criteria for electrographic status epilepticus.
Hepatic encepathopathy, Infectious meningoencephalitis, Central nervous system hemorrhage, Central venous system infarction.
Ammonia, 88 μmol/L.
The results of a magnetic resonance imaging brain scan exhibited symmetrical high-signal abnormalities in the basal ganglia on T1-weighted images, consistent with liver cirrhosis.
Despite the patient being treated with levetiracetam for 4 d, he did not improve neurologically.
To the best of the authors’ knowledge, this is the first reported case of such a presentation in Korea.
Nonconvulsive status epilepticus is an approximately clinical disorder defined as prolonged seizure activity without major motor signs for at least 30 min.
It is important to consider the possibility of nonconvulsive status epilepticus, evaluating the patient with liver cirrhosis who presents with an altered mental status, and especially the patient who does not respond to empirical treatment.
It is important to understand the possibility of nonconvulsive status epilepticus disguising as hepatic encephalopathy in evaluating for especially patient with liver cirrhosis who presents an altered mental status.
P- Reviewer: Chamuleau RAFM, Cao WK, Montagnese S S- Editor: Yu J L- Editor: A E- Editor: Ma S
| 1. | White H. Neurologic manifestations of acute and chronic liver disease. Continuum (Minneap Minn). 2014;20:670-680. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Rothstein JD, Herlong HF. Neurologic manifestations of hepatic disease. Neurol Clin. 1989;7:563-578. [PubMed] [Cited in This Article: ] |
| 3. | Ficker DM, Westmoreland BF, Sharbrough FW. Epileptiform abnormalities in hepatic encephalopathy. J Clin Neurophysiol. 1997;14:230-234. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 36] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Walker MC. Status epilepticus on the intensive care unit. J Neurol. 2003;250:401-406. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 34] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Kaplan PW. Assessing the outcomes in patients with nonconvulsive status epilepticus: nonconvulsive status epilepticus is underdiagnosed, potentially overtreated, and confounded by comorbidity. J Clin Neurophysiol. 1999;16:341-352; discussion 353. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 178] [Cited by in F6Publishing: 161] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 6. | Drislane FW. Presentation, evaluation, and treatment of nonconvulsive status epilepticus. Epilepsy Behav. 2000;1:301-314. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 113] [Cited by in F6Publishing: 109] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 7. | Blennow G, Brierley JB, Meldrum BS, Siesjö BK. Epileptic brain damage: the role of systemic factors that modify cerebral energy metabolism. Brain. 1978;101:687-700. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 336] [Cited by in F6Publishing: 346] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 8. | Fountain NB, Waldman WA. Effects of benzodiazepines on triphasic waves: implications for nonconvulsive status epilepticus. J Clin Neurophysiol. 2001;18:345-352. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 92] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Waterhouse EJ, DeLorenzo RJ. Status epilepticus in older patients: epidemiology and treatment options. Drugs Aging. 2001;18:133-142. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 59] [Article Influence: 2.6] [Reference Citation Analysis (0)] |