Published online Mar 14, 2015. doi: 10.3748/wjg.v21.i10.3030
Peer-review started: April 29, 2014
First decision: May 29, 2014
Revised: August 6, 2014
Accepted: November 8, 2014
Article in press: November 11, 2014
Published online: March 14, 2015
Processing time: 322 Days and 21.6 Hours
AIM: To investigate the relationship between reflux and body mass index (BMI) in the asymptomatic obese population using the impedance-pH technique.
METHODS: Gastroesophageal reflux is frequent in the obese population. However, the relationship between acid reflux and BMI in asymptomatic obese people is unclear. Forty-six obese (BMI > 25 kg/m2) people were enrolled in this prospective study. We evaluated the demographic findings and 24-h impedance pH values of the whole group. Gas, acid (pH < 4), weak acid (pH = 4-7) and weak alkaline (pH ≥ 7) reflux parameters were analyzed.
RESULTS: The mean age of patients was 49.47 ± 12.24 years, and half of them were men. The mean BMI was 30.64 ± 3.95 kg/m2 (25.14-45.58 kg/m2). BMI of 23 was over 30 kg/m2. Seventeen patients had a comorbidity (hypertension, diabetes mellitus, or ischemic heart disease). Endoscopic examination revealed esophagitis in 13 of the 28 subjects (10 Grade A, 3 Grade B). The subjects were divided into two groups according to BMI (< 30 and > 30 kg/m2). Demographic and endoscopic findings, and impedance results were similar in these two groups. However, there was a positive correlation between BMI and total and supine pH < 4 episodes (P = 0.002, r = 0.414; P = 0.000, r = 0.542), pH < 4 reflux time (P = 0.015, r = 0.319; P = 0.003, r = 0.403), and DeMeester score (P = 0.012, r = 0.333).
CONCLUSION: Acid reflux is correlated with BMI in asymptomatic obese individuals.
Core tip: Obesity is an increasing problem worldwide. Few studies have reported on the association between gastroesophageal reflux symptoms and body mass index (BMI). We aimed to determine the effects of BMI on gastroesophageal reflux using esophageal pH-impedance technique in asymptomatic overweight and obese subjects. We found that BMI is positively correlated with acid reflux. Our study demonstrated that obesity is a risk factor for gastroesophageal reflux even in an asymptomatic healthy individuals. These findings are important for the obese population who are referred for bariatric surgery. Gastroesophageal reflux should be evaluated carefully before surgery, even in the absence of symptoms.
- Citation: Akyüz F, Uyanıkoglu A, Ermis F, Arıcı S, Akyüz &, Baran B, Pinarbasi B, Gul N. Gastroesophageal reflux in asymptomatic obese subjects: An esophageal impedance-pH study. World J Gastroenterol 2015; 21(10): 3030-3034
- URL: https://www.wjgnet.com/1007-9327/full/v21/i10/3030.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i10.3030
Obesity is an increasing problem worldwide. It is predicted that by the year 2020, 77.6% of men will be overweight and 40.2% obese; the corresponding predictions for women are 71.1% overweight and 43.3% obese[1]. Obesity is the main cause of many diseases such as cardiac, diabetes mellitus, nonalcoholic fatty liver disease. Gastroesophageal reflux disease (GERD) is also a common disorder in most countries. The etiopathogenesis of gastroesophageal reflux is multifactorial (impaired gastric emptying and esophageal clearance, etc.). A limited number of studies have reported on the association between gastroesophageal reflux symptoms and body mass index (BMI)[2,3]. A recently published meta-analysis showed that increased BMI was a risk factor for gastroesophageal reflux (OR = 1.89, 95%CI: 1.70-2.09)[4]. However, at present, the relationship between obesity and gastrointestinal symptoms remains poorly understood. We aimed to determine the effects of BMI on gastroesophageal reflux using the esophageal pH-impedance technique in overweight and obese subjects.
Forty-six overweight and obese subjects were consecutively included in this study between January 2007, and December 2009. Patients who were admitted to our hospital for a check-up or losing weight were recruited from internal medicine out-patient clinics. All patients were evaluated in terms of esophageal (heartburn, regurgitation) and extraesophageal (laryngitis, night coughs, dyspnea) symptoms before the study. Individuals who had any reflux symptoms in the last six months were excluded.
At the onset of the study, the participants underwent physical examinations. Medical histories, family histories, social habits (alcohol use and smoking) and BMI scores (kg/m2) were evaluated. BMI was classified according to the World Health Organisation classification: 18.5-24.9 kg/m2 (normal range), 25-30 kg/m2 (overweight), 30-40 kg/m2 (obese ), and > 40 kg/m2 morbid obese[5].
The participants were subsequently evaluated with the 24-h esophageal impedance pH-metry through a similar approach. Information regarding the study was provided to the patients and their written informed consents were taken in accordance with the Helsinki Declaration. The local ethics committee approved the study.
The patients were evaluated with the 24-h esophageal impedance pH-metry without disrupting their daily routine activities.
Ambulatory 24 h esophageal impedance pH-metry was performed with a mobile recording device (Ohmega Impedance ambulatory pH-metry; MMS, Enschede, Netherlands) and the catheter had an 8 impedance ring and 1 antimony pH measurement loop (Versa Flex Z-Impedance pH-metry disposable catheters; Alpine bio Med, Fountain Valley, CA, United States). Impedance pH-metry catheters were passed transnasally under topical anaesthesia and positioned to record pH 5 and impedance at 3, 5, 7, 9, 15 and 17 cm proximal to the lower esophageal sphincter (LES) in the esophageal body at 8:00 am. Postero-anterior chest X-rays were taken to confirm the correct positioning of the catheter. The catheter was not removed until the following day at 8:00 am. After a 24-h investigation, recordings were uploaded onto a personal computer. All data were interpreted under a related program manually by one expert (Akyüz F). Gastroesophageal reflux was defined as a sequential orally progressing drop in impedance to less than 50% of baseline values starting distally (3 cm above the LES) and propagating retrogradely to at least the next 2 more proximal impedance rings. Depending on the corresponding pH change, impedance detected reflux was classified as follows: (1) acid reflux: pH decrease < 4 for a period of at least 4 s during reflux or at least 1 unit decrease in pH for at least 4 s when pH is already below 4 (acid re-reflux) (superimposed reflux) were defined as acid reflux; (2) weakly acidic reflux: At least 1 unit of pH decrease for at least 4 s, while the maintenance of pH between 4-7 during the reflux were defined as weakly acidic reflux; and (3) weakly alkaline (non-acid) reflux: pH above 7 during reflux was defined as weakly alkaline reflux[6].
Each reflux episode was classified as liquid, gas, or mixed. Liquid, gas, mixed, acid, weak acid and weak alkaline reflux, the percentage of time period of pH < 4 relative to the total time, the number of episodes with pH < 4 were evaluated separately for 24 h recording periods in the supine and standing positions. The number and percentage of reflux episodes extending to the proximal esophagus (the number of reflux episodes extending 15 cm above the esophagus sphincter), bolus clearance time, the number of swallows and the DeMeester score were evaluated as a 24-h record. Results of Zerbib et al[7] were used as a normal values. Twenty-eight patients who had weakly or acid reflux in impedance gave consent to undergo gastroscopy.
Statistical analyses were carried out by SPSS 13.0. Independent groups were compared using the non-parametric Mann-Whitney U test. Dependent groups were evaluated with the Wilcoxon signed-rank test. Correlation analyses were performed using Spearman’s correlation tests. Multivariate regression analyses were performed to define the risk factor for acid reflux. Data are presented as mean values or as count and percentages, as appropriate. A P-value lower than 0.05 was considered to be statistically significant.
Forty-six obese (BMI > 25 kg/m2) patients were enrolled in this prospective study. The mean age of patients was 49.47 ± 12.24 years, and half of them were men. The mean BMI was 30.64 ± 3.95 kg/m2 (25.14-45.58 kg/m2). BMI of 23 patients was over 30 kg/m2. Seventeen patients had comorbidities (mild hypertension, diabetes mellitus, or ischemic heart disease). Endoscopic examination revealed esophagitis in 13/28 patients (10 Grade A, 3 Grade B). None of the patients had hiatal hernia. Pathologic weakly acid reflux was detected in half of all the patients and the pathologic acid reflux rate was 34.8% (n = 16). Only one patient whose BMI was < 30 kg/m2 had pH > 7 reflux (Table 1).
| Age, yr (mean/range) | 49 ± 12 (28-70) |
| Sex, n (female/male) | 23/23 |
| BMI, kg/m2 (mean age, range) | |
| < 30 | 27.7 ± 1.7 (25-29) |
| > 30 | 33.5 ± 3.3 (30.5-45.5) |
| Comorbidity | 37.0% |
| Smoking | 23.9% |
| Endoscopic esophagitis | 46.0% |
| Impedance results, n (%) | |
| Normal | 14 (30.4) |
| Pathologic acid reflux | 16 (34.8) |
| Weakly acid reflux | 15 (32.6) |
| Weakly alkaline reflux | 1 (2.2) |
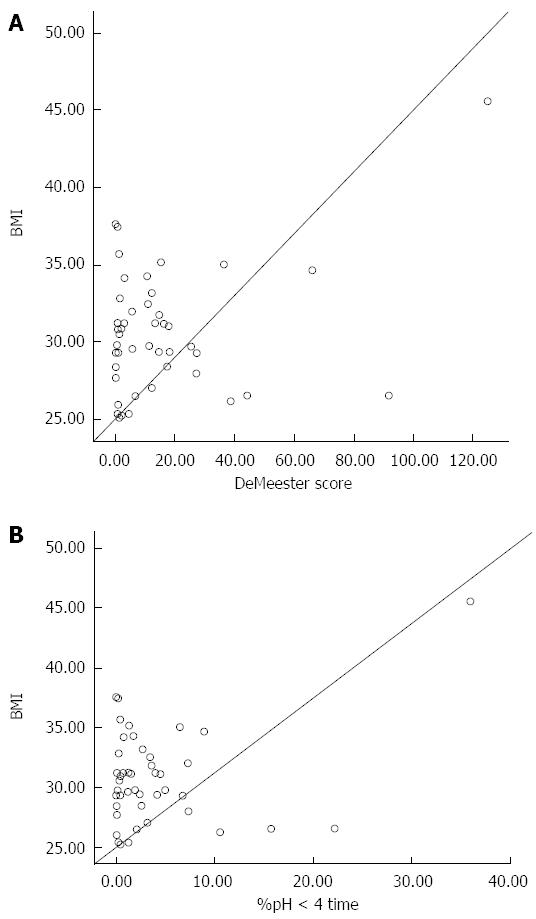
There was a positive correlation between BMI and total and supine pH < 4 episode number (P = 0.002, r = 0.414; P = 0.000, r = 0.542), < pH 4 reflux time (P = 0.015, r = 0.319; P = 0.003, r = 0.403) and DeMeester score (P = 0.012, r = 0.333) (Figure 1). In a multivariate regression analysis, only BMI was determined to be an independent risk factor for acid reflux (P = 0.024). Alcohol use, smoking, comorbidity, age and sex was not related to reflux in the multivariate regression analyses (P > 0.05).
The patients were divided into two groups according to BMI (< 30 kg/m2 and > 30 kg/m2). However, the demographics, endoscopic findings, and impedance results were similar in these two groups (Table 2).
| Impedance results, n | BMI > 30 kg/m2 (n = 23) | BMI < 30 kg/m2 (n = 23) | P value |
| Total gas reflux | 25.8 ± 34.7 (0-157) | 18.5 ± 13.3 (0-52) | 0.87 |
| Upright gas reflux | 20 ± 20 (0-88) | 16.9 ± 13 (0-52) | 0.82 |
| Acid reflux episodes | 26 ± 54 (0-268) | 26 ± 24 (1-77) | 0.87 |
| Weakly acid reflux episodes | 28 ± 31 (3-143) | 22 ± 20 (4-105) | 0.82 |
| Time of pH < 4 | 3.6% ± 7.4% (0%-35%) | 3.7% ± 5.5% (0%-22%) | 0.99 |
| Longest episodes of acid reflux | 6 ± 7.5 (0.14-25) | 11.7 ± 21 (0-90) | 0.88 |
| DeMeester score | 15.7 ± 27.9 (0.2-124) | 15.3 ± 21.09 (0.2-91) | 0.97 |
| Pathologic acid reflux, n (%) | 7 (30.4) | 9 (39.1) | 0.70 |
| Weakly acid reflux, n (%) | 9 (39.1) | 6 (26.1) | 0.70 |
| Weakly alkaline reflux, n (%) | - | 1 (4.3) | |
| Normal impedance findings, n (%) | 7 (30.4) | 7 (30.4) | 0.70 |
GERD prevalence has increased during the last decade. This is most probably related to obesity and changed diet. To date, most studies have been interested in symptomatic patients and have investigated the role of obesity in GERD. In a meta-analyses, a significant association between gastroesophageal reflux (OR = 1.89, 95%CI: 1.70-2.09) and increasing BMI was found[4].
Ayazi et al[8] retrospectively evaluated GERD patients’ 24-h pH-metry and manometry reports. They divided patients into four groups according to their BMI (under weight, normal weight, over weight, and obese) and showed that BMI was positively correlated with acid reflux. A significant difference was found between all groups. They also found that the rate of defective LES was higher in obese patients. However, the defective LES rate was similar in overweight and obese patients (50% vs 55%). There are few studies that are interested in an asymptomatic obese individuals for gastroesophageal reflux. In our study, we investigated the relationship between BMI and esophageal reflux using the impedance technique in asymptomatic overweight and obese people. We found that BMI was positively correlated with acid reflux. However, we found no difference between overweight and obese patients. This may be related with the limited number of patients or the presence of patients with high DeMeester scores in both groups. In another study, impedance was performed on proton pump inhibitor treatment in GERD patients. The positive symptom index and non-acid reflux rate was higher in obese patients (BMI > 30 kg/m2) than the others (BMI < 25 kg/m2 and BMI 25-30 kg/m2). The authors concluded that obesity increases reflux and increase the symptoms[9]. In our study, non-acid reflux was similar in the obese and overweight groups, and we found no correlation between non-acid reflux and BMI. We found no symptom correlation with higher BMI because our cases were asymptomatic.
Schneider et al[10] performed an impedance study in morbidly obese patients and a control group (BMI < 35 kg/m2). The median DeMeester score on pH-metry was significantly different between the various stages of obesity. However the severity of GERD was not directly related to the stage of obesity. We also found no correlation between the grade of esophagitis and BMI.
Ricci et al[11] investigated esophageal reflux by 24-h pH-metry + MII in 20 non-GERD and 15 GERD obese patients, 15 non-obese GERD and 10 healthy controls. Reflux symptoms and hiatal hernia were also observed in non-GERD patients. The percentage of time for acid exposure was significantly higher in obese non-GERD patients than controls (P = 0.007). Acid reflux episodes were higher in obese non- GERD (P = 0.005) and obese GERD (P = 0.034) patients than controls. Erosive esophagitis rates were similar in all groups. Our group was completely asymptomatic for reflux symptoms and we did not detect any hernias. Interestingly, in our group, the erosive esophagitis rate was high even though the patients were asymptomatic. However, we found no significant predictor for erosive esophagitis in the multivariate analyses. Smoking, alcohol consumption and cultural diet may be effective on erosive reflux.
Some patients do not easily perceive esophageal acid reflux[12]. This silent reflux can be detected incidentally[13]. Miwa et al[14] investigated the symptoms of esophagitis in 275 patients with endoscopically diagnosed reflux esophagitis by using a questionnaire and they found that 28.5% of these patients had silent GERD with no typical symptoms such as heartburn or regurgitation and fewer atypical symptoms compared with symptomatic patients. These findings showed that some patients have silent reflux. Our results also support these findings. This clinical situiation may be explained by hyposensitive esophagus.
We demonstrated that obesity is a risk factor for gastroesophageal reflux even in asymptomatic healthy individuals. Symptoms are subjective and sensitivity of the esophagus differs between individuals. All patients were questioned again after the impedance evaluation and they confirmed that they had no reflux symptoms. As previously reported[11], the proximal extent (at least 15 cm above the LES) of reflux is higher in obese non-GERD patients. We also found no correlation between BMI and proximal extent of reflux. The clinical impact of these findings is especially important for bariatric surgery in the obese population. Gastroesophageal reflux increases after sleeve gastrectomy[15,16]. Therefore, patients should be carefully evaluated before surgery even in the absence of symptoms.
In conclusion, obesity is a risk factor for gastroesophageal reflux. Acid reflux is correlated with BMI in obese individuals.
Obesity is an increasing problem worldwide. Different treatment modalities including bariatric surgery are becoming popular in last years. Gastroesophageal reflux disease is also a common disorder. A limited number of studies have reported on the association between gastroesophageal reflux symptoms and body mass index.
In this study authors investigated the relationship between reflux and body mass index in the asymptomatic obese population using the impedance-pH technique.
There are few studies that are interested in obese individuals asymptomatic for gastroesophageal reflux. Their group was completely asymptomatic for reflux symptoms and the authors did not detect any hernias. Interestingly, in the group, the erosive esophagitis rate was high even though the patients were asymptomatic. The clinical impact of these findings is especially important for bariatric surgery in the obese population. Patients should be carefully evaluated before surgery even in the absence of symptoms.
Further studies should be designed to evaluate the long term effects of silent reflux after bariatric surgery.
Some patients do not easily perceive esophageal acid reflux. This is called silent reflux in the literature.
Obesity is a risk factor for gastroesophageal reflux. Acid reflux is correlated with body mass index in obese individuals. Patients should be carefully evaluated before bariatric surgery even in the absence of symptoms.
P- Reviewer: Herbella FAM S- Editor: Gou SX L- Editor: O’Neill M E- Editor: Ma S
| 1. | Ruhm CJ. Current and future prevalence of obesity and severe obesity in the United States (June 2007). National Bureau of Economic Research (NBER) Working Paper No. W13181. Available from: http://ssrn.com/abstract = 994229. |
| 2. | Locke GR, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ. Risk factors associated with symptoms of gastroesophageal reflux. Am J Med. 1999;106:642-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 339] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 3. | Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Obesity and estrogen as risk factors for gastroesophageal reflux symptoms. JAMA. 2003;290:66-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 319] [Cited by in RCA: 331] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 4. | Eslick GD. Gastrointestinal symptoms and obesity: a meta-analysis. Obes Rev. 2012;13:469-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 110] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 5. | Gastrointestinal symptoms and obesity: a meta-analysis. Obesity: preventing and managing the global epidemic. Report on a WHO Consultation on Obesity, Geneva, 3-5 June, 1997 (WHO/NUT/NCD/98.1). Technical Report Series Number 894. Geneva: World Health Organization 2000; . |
| 6. | Sifrim D, Dupont L, Blondeau K, Zhang X, Tack J, Janssens J. Weakly acidic reflux in patients with chronic unexplained cough during 24 hour pressure, pH, and impedance monitoring. Gut. 2005;54:449-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 264] [Cited by in RCA: 265] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 7. | Zerbib F, Roman S, Bruley Des Varannes S, Gourcerol G, Coffin B, Ropert A, Lepicard P, Mion F. Normal values of pharyngeal and esophageal 24-hour pH impedance in individuals on and off therapy and interobserver reproducibility. Clin Gastroenterol Hepatol. 2013;11:366-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 131] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 8. | Ayazi S, Hagen JA, Chan LS, DeMeester SR, Lin MW, Ayazi A, Leers JM, Oezcelik A, Banki F, Lipham JC. Obesity and gastroesophageal reflux: quantifying the association between body mass index, esophageal acid exposure, and lower esophageal sphincter status in a large series of patients with reflux symptoms. J Gastrointest Surg. 2009;13:1440-1447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 115] [Cited by in RCA: 120] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 9. | Hajar N, Castell DO, Ghomrawi H, Rackett R, Hila A. Impedance pH confirms the relationship between GERD and BMI. Dig Dis Sci. 2012;57:1875-1879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Schneider JM, Brücher BL, Küper M, Saemann K, Königsrainer A, Schneider JH. Multichannel intraluminal impedance measurement of gastroesophageal reflux in patients with different stages of morbid obesity. Obes Surg. 2009;19:1522-1529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Ricci G, Amella C, Forti E, Rossi A, Bersani G, Dari S, Pasini V, Maimone A, Alvisi V. 24-h pH-metry and multichannel intraluminal impedance monitoring in obese patients with and without gastroesophageal reflux disease symptoms. Obes Surg. 2011;21:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Fass R, Sampliner RE, Mackel C, McGee D, Rappaport W. Age- and gender-related differences in 24-hour esophageal pH monitoring of normal subjects. Dig Dis Sci. 1993;38:1926-1928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Fass R, Dickman R. Clinical consequences of silent gastroesophageal reflux disease. Curr Gastroenterol Rep. 2006;8:195-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 47] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Miwa H, Kondo T, Oshima T, Fukui H, Tomita T, Watari J. Esophageal sensation and esophageal hypersensitivity - overview from bench to bedside. J Neurogastroenterol Motil. 2010;16:353-362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 15. | Carter PR, LeBlanc KA, Hausmann MG, Kleinpeter KP, deBarros SN, Jones SM. Association between gastroesophageal reflux disease and laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2011;7:569-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 109] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 16. | Himpens J, Dobbeleir J, Peeters G. Long-term results of laparoscopic sleeve gastrectomy for obesity. Ann Surg. 2010;252:319-324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 572] [Cited by in RCA: 569] [Article Influence: 37.9] [Reference Citation Analysis (0)] |