Published online Mar 14, 2015. doi: 10.3748/wjg.v21.i10.2973
Peer-review started: August 23, 2014
First decision: November 14, 2014
Revised: December 8, 2014
Accepted: February 5, 2015
Article in press: February 5, 2015
Published online: March 14, 2015
Processing time: 207 Days and 8.6 Hours
AIM: To introduce a simple and safe anvil insertion technique to esophagus during laparoscopic total gastrectomy (LTG).
METHODS: Between July 2010 and December 2012, 58 consecutive patients with early gastric cancer underwent LTG were enrolled. We performed a simple and safe Roux-en-Y esophagojejunostomy using the double stapling technique to all patients. Then patients’ characteristics, perioperative outcome and histopathologic data were analyzed retrospectively.
RESULTS: The mean age and body mass index were 59.3 ± 9.7 years and 22.7 ± 2.6 kg/m2. The mean operation, reconstruction and anvil insertion times (from gastric incision to linear stapling) were 251.8 ± 57.0, 43.1 ± 2.8 and 4.2 ± 1.9 min, respectively. Intraoperative blood loss was 204.6 ± 156.3 mL and there was no open conversion. The postoperative complications were in 8 cases (delayed gastric emptying in 4 cases, pulmonary complication in 2 cases, pancreatitis in 1 case, anastomotic stricture in 1 case). Anastomotic stricture occurred after discharge and was recovered by endoscopic intervention. The patients were discharged at a mean of 9.6 ± 2.0 d after surgery. Neither leakage nor bleeding from the esophagojejunostomy occurred postoperatively. The mean proximal margin of specimen was 2.7 ± 2.8 cm
CONCLUSION: Roux-en Y esophagojejunostomy using the double stapling technique is simple and rapid, and it may offer a solid, alternative reconstruction method for LTG or proximal gastrectomy.
Core tip: Although laparoscopic total gastrectomy for upper gastric cancer has become popular in Korea, esophagojejunostomy remains a difficult procedure. Recently introduced intracorporeal esophagojejunostomy methods facilitate more convenient anastomosis. We describe the modified double stapling technique (which has been used in colorectal surgery) for esophagojejunostomy after laparoscopic total gastrectomy (LTG). Although it cannot be used for all patients undergoing LTG because of the lack of long-term survival data, this double stapling technique can provide easy and safe anastomosis after LTG. In particular, it may be a considerable option for inexperienced surgeons.
- Citation: Kim JH, Choi CI, Kim DI, Kim DH, Jeon TY, Kim DH, Park DY. Intracorporeal esophagojejunostomy using the double stapling technique after laparoscopic total gastrectomy: A retrospective case-series study. World J Gastroenterol 2015; 21(10): 2973-2981
- URL: https://www.wjgnet.com/1007-9327/full/v21/i10/2973.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i10.2973
In the last decade, laparoscopic gastrectomy after laparoscopic surgery for early gastric cancer has been increasingly used worldwide. Laparoscopic-assisted distal gastrectomy and even totally laparoscopic distal gastrectomy are now commonly performed to treat early gastric cancer in Korea.
D1+ lymph node dissection and Roux-en-Y esophagojejunostomy are generally accepted as standard laparoscopic total gastrectomy (LTG) procedures for treating early gastric cancer. LTG has become as common as laparoscopic distal gastrectomy; however, LTG is still technically challenging when dissecting short gastric arteries (lymph node 4sa), as well as when performing esophagojejunostomy[1,2]. With improved surgical skills and the development of laparoscopic instruments, LTG with lymph node dissection is less complicated, and stapling devices provide excellent anastomosis, with low failure or leakage rates. Nevertheless, purse-string sutures and anvil insertions are still problematic due to the narrow operation field or the need for more experienced manipulations[3,4].
Various techniques and instruments for intracorporeal esophagojejunostomy have been reported, and intracorporeal suture is no longer a specialized procedure. However, some techniques, such as OrVilTM or overlap methods, might still be little complicated and time consuming for inexperienced surgeons. Therefore, we have devised a simple, rapid anvil insertion technique (i.e., the double stapling technique for Roux-en-Y esophagojejunostomy) that can be used after performing LTG. Despite its simplicity, it has rarely been reported in large LTG cohorts. The details of this technique are described herein.
Between July 2010 and December 2012, 58 consecutive patients (42 men and 16 women) with early gastric cancer underwent LTG using this double stapling esophagogastrostomy technique at Pusan National University Hospital. Patients with early gastric cancer invading the upper third part of the stomach without lymph node metastasis were included in the study. Patients with tumors located within 2 cm of the esophagogastric junction were excluded from this study because of the possibility of tumor spillage during anastomosis. Patient selection was based on preoperative examinations, including endoscopic ultrasonography, esophagogastroduodenoscopy and abdominal computed tomography. We also retrospectively analyzed the patients’ characteristics, as well as their intraoperative and postoperative outcomes.
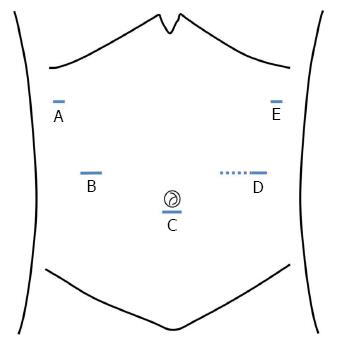
Each patient was placed in the lithotomy position. The operator stood on the right side of the patient. The first assistant stood on the left side, and the scopist stood between the patient’s legs. Then, a CO2 pneumoperitoneum was established through a 10 mm umbilical port, with pressure maintained at < 15 mmHg. Five ports were inserted in the abdomen, same to conventional laparoscopic gastrectomy (Figure 1). After completing the resection procedure, including D1+ lymph node dissection (except for the esophageal transection), Roux-en-Y reconstruction was performed using modified double-stapling esophagojejunostomy, as follows.
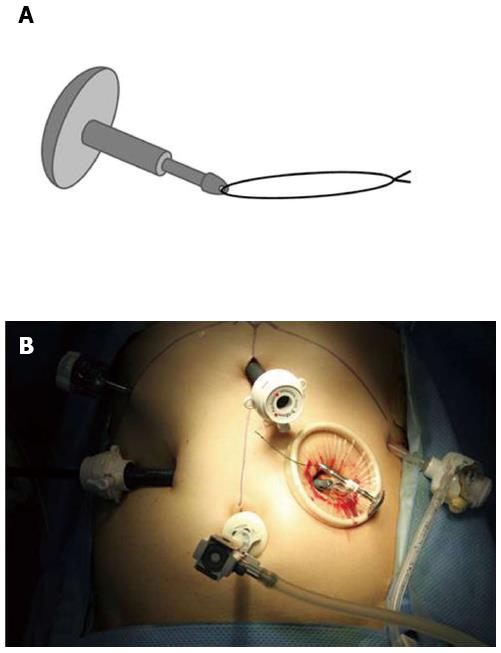
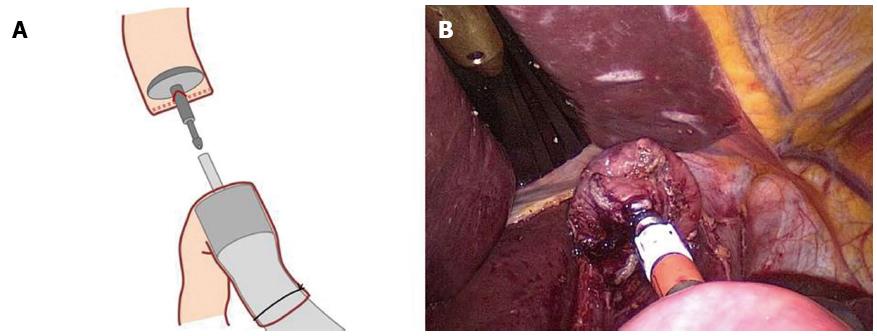
Firstly, anvil preparation: A 5-cm length of stay-suture was applied to the tip of the anvil (Premium Plus CEEA 25, US Surgical, Norwalk, CT, United States), and a 3- to 4-cm mini-laparotomy was performed at the site of the left lower port (Figure 2A). The mini-laparotomy wound was retracted and protected with a laparotomy wound retractor (Alexis Wound Retractor; Applied Medical, CA, United States). The anvil was inserted into the abdominal cavity through the mini-laparotomy, and the pneumoperitoneum was re-established by sealing off the laparotomy wound retractor with a surgical glove (Figure 2B).
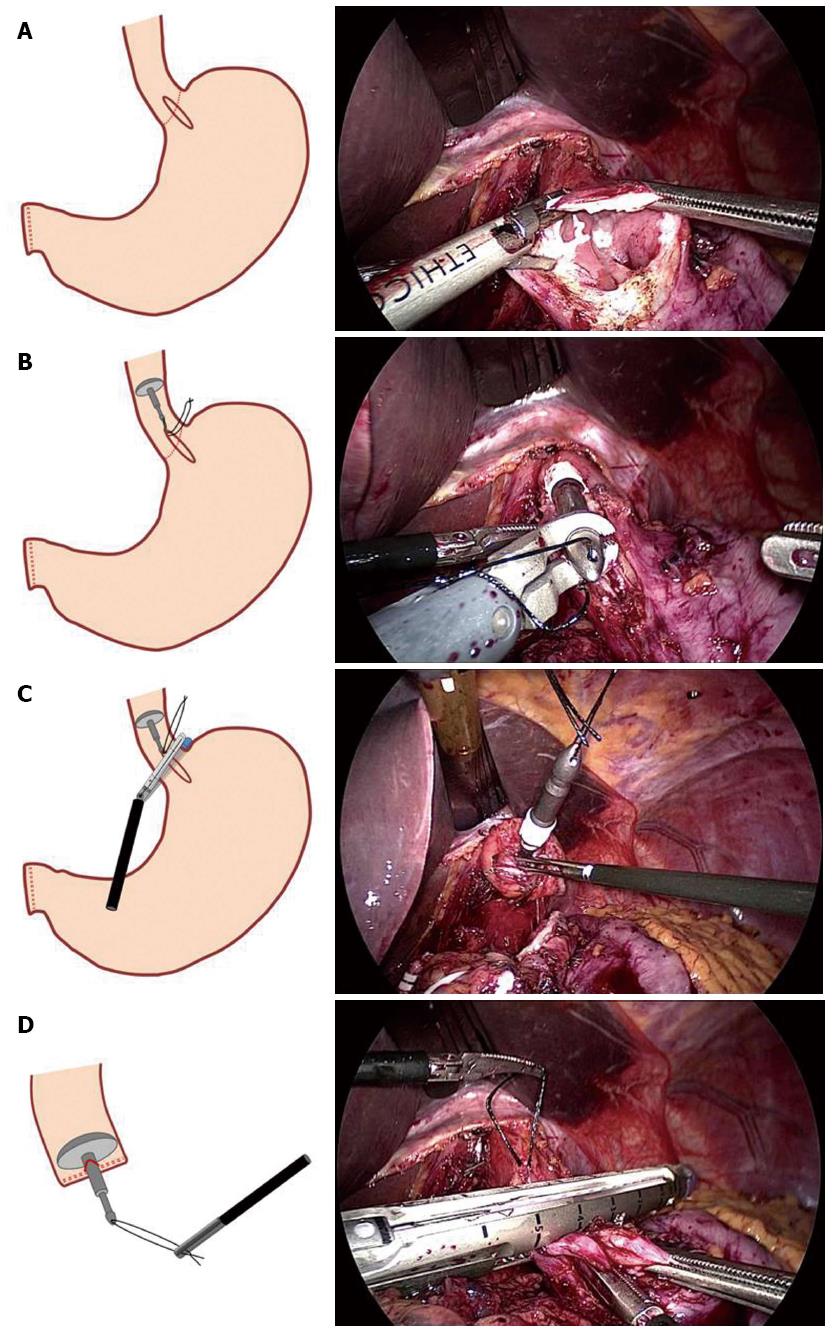
Secondly, anvil insertion: Gastrotomy was performed approximately 1 to 2 cm below the esophagogastric junction (away from the tumor mass), and it could be extended approximately 3 cm across the esophagogastric junction using a harmonic scalpel (Ethicon Endo-Surgery, Cincinnati, OH, United States) (Figure 3A). The prepared anvil was inserted into the esophagus through the gastrotomy and then placed in the thoracic esophagus (Figure 3B). Subsequently, the distal esophagus was transected with an Endo GIA linear stapler (Endo GIA 60, US Surgical, Norwalk, CT, United States). Then, to avoid disrupting the stay-suture during the linear stapling, the stay-suture was cranially lifted while dividing the distal esophagus (Figure 3C). The stay-suture was pulled through the remaining hole until the anvil reached the esophageal stump (Figure 3D). The gastrotomy site was grasped with forceps, or a laparoscopic bulldog clamp was used to prevent spillage of the gastric contents. The resected specimen was delivered through the mini-laparotomy.
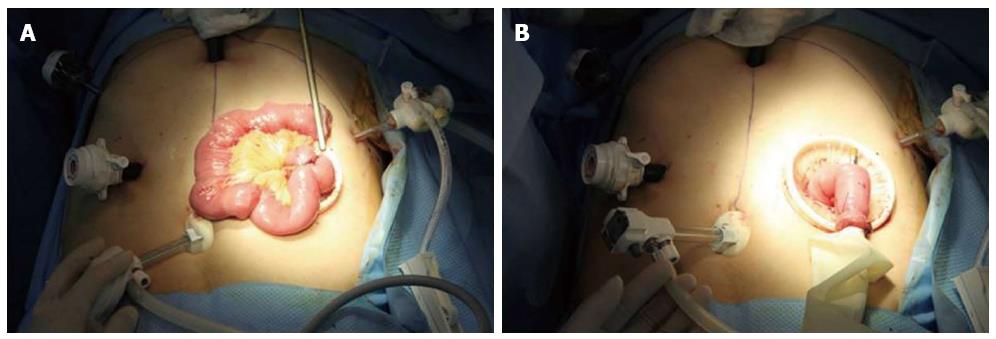
Thirdly, jejunojejunostomy: The jejunum was brought out through the mini-laparotomy and divided 15 to 20 cm distal to the ligament of Treitz. An extracorporeal end-to-side jejunojejunostomy was manually performed 45 cm below the site at which the esophagojejunostomy would be performed (Figure 4A).
Lastly, esophagojejunostomy: For intracorporeal use, a surgical glove was attached to the circular stapler. The circular stapler was inserted into the Roux limb, which was tied to the body of the circular stapler to prevent separation from the jejunum (Figure 4B). Then, the body of the circular stapler was introduced into the abdominal cavity, and the pneumoperitoneum was re-established using the attached surgical glove. Esophagojejunostomy was performed under laparoscopic view (Figure 5). Finally, the jejunal stump of the Roux limb was closed with an Endo GIA linear stapler.
Statistical analyses were performed using SPSS software (version 18; SPSS Inc., Chicago, IL, United States). For continuous variables, the one sample t-test was used to identify the mean value and for categorical data, frequency analysis was used. Quantitative data was expressed as mean ± SD.
The statistical methods of this study were reviewed by Professor Jin Mi Kim, who is biomedical statistician from Pusan National University Hospital.
A total of 58 consecutive patients underwent LTG with Roux-en-Y esophagojejunostomy using this double-stapling technique at our institute. Preoperative patient data are shown in Table 1.
| Variables | |
| Sex | |
| Male | 42 (72.4) |
| Female | 16 (27.6) |
| Age (yr) | 59.3 ± 9.7 (39-78) |
| BMI (kg/m2) | 22.7 ± 2.6 (16.6-28.1) |
| ASA score | |
| 1 | 25 (43.1) |
| 2 | 31 (53.4) |
| 3 | 2 (3.4) |
The mean operation time was 251.8 ± 57.0 min. The mean reconstruction time was 43.1 ± 2.8 min, and the mean anvil insertion time was 4.2 ± 1.9 min. There were no cases of intraoperative complications or open conversion. An upper gastrointestinal study using water-soluble contrast medium was routinely performed on the 4th postoperative day to evaluate for anastomotic leaks and strictures. In all patients, the contrast medium passed into the jejunum easily and without resistance; however, anastomotic stricture was observed in 1 patient after discharge. There was no sign of leakage at the esophagojejunostomy in any patient. Oral feeding was started at a mean of 4.9 ± 0.6 d after surgery. The mean hospital stay after surgery was 9.6 ± 2.0 d. The mean follow-up period was 26.8 ± 10.8 mo, and there were no local recurrences or cancer-related deaths (Table 2).
| Variables | |
| Operation time (min) | 251.8 ± 57.0 |
| Reconstruction time (min) | 43.1 ± 2.8 |
| Anvil insertion time (min) | 4.2 ± 1.9 |
| Intraoperative blood loss (mL) | 204.6 ± 156.3 |
| Open conversion | 0 |
| Postoperative complications | 8 (13.8) |
| Dumping syndrome | 4 (6.9) |
| Pulmonary complication | 2 (3.4) |
| Anastomotic stricture | 1 (1.7) |
| Pancreatitis | 1 (1.7) |
| Oral intake (d) | 4.9 ± 0.6 |
| Hospital stay (d) | 9.6 ± 2.0 |
| Mean follow-up period (mo) | 26.8 ± 10.8 |
Advanced gastric cancer (i.e., invading beyond the submucosal layer of the gastric wall) was confirmed in 8 cases. The mean total resected lymph node number was 55.1 ± 22.0, and the mean length of the proximal margin was 2.8 ± 2.1 cm (Table 3).
| Variables | n (%) |
| Tumor invasion depth | |
| Mucosa (T1a) | 19 (32.8) |
| Submucosa (T1b) | 31 (53.4) |
| Muscle propria (T2) | 4 (6.9) |
| Subserosa (T3) | 1 (1.7) |
| Serosa exposed (T4) | 3 (5.2) |
| Nodal metastasis | |
| 0 (N0) | 52 (89.7) |
| 1-2 (N1) | 3 (5.2) |
| 3-7 (N2) | 2 (3.4) |
| > 8 (N3) | 1 (1.7) |
| TNM1 stage | |
| IA | 46 (79.3) |
| IB | 4 (6.9) |
| IIA | 3 (5.2) |
| IIB | 5 (8.6) |
| Total number of resected lymph nodes | 55.1 ± 22.0 |
| Proximal margin (cm) | 2.7 ± 2.8 |
A nationwide survey in Korea by Yang et al and the Information Committee of the Korean Gastric Cancer Association reported that in 2004, laparoscopic assisted total gastrectomy was performed in only 20 patients compared with laparoscopic assisted distal gastrectomy (344 patients)[1]. In addition, the major obstacles to performing laparoscopic gastrectomy were medical insurance problems and technical difficulties. In recent years, laparoscopic gastrectomy has become a more popular and standard treatment option for early gastric cancer in most medical institutions in Korea. According to a 2009 Korea nationwide survey of gastric cancer reported by Jeong et al[5], 3783 patients (25.8% of total patients) underwent laparoscopic gastric resection. In addition, the popularity of laparoscopic gastric surgery is increasing annually due to improvements in instruments and surgical skill. Until now, however, many surgeons have been hesitant to perform LTG due to its technical difficulties, particularly the difficulties with anastomosis compared to lymph node dissection[6-8].
Since a circular stapler was first utilized in esophagojejunostomy, most esophagojejunostomies have been performed using a circular stapler in open total gastrectomy. Esophagojejunostomy during open total gastrectomy is easy and safe because open laparotomy allows for a sufficient operative field for performing the anastomosis. However, extracorporeal end-to-side esophagojejunostomy, which is generally used after LTG (in the same manner as esophagojejunostomy after open gastrectomy), cannot provide an adequate operative field for anastomosis[9,10]. Therefore, a larger incision, similar to that for open total gastrectomy, is necessary for both esophagojejunostomy and jejunojejunostomy, particularly in obese patients with a thick abdominal wall; such an incision could diminish the merits of laparoscopic surgery[11]. Various intracorporeal anastomosis techniques have been developed for this reason, thereby simplifying esophagojejunostomy. However, there is still some debate about the optimal reconstruction procedure.
Intracorporeal reconstruction can be divided into side-to-side anastomosis using a linear stapler and end-to-side anastomosis using a circular stapler. After side-to-side anastomosis was first introduced by Walther et al[12], simpler and safer (modified) methods of side-to-side anastomosis for esophagojejunostomy have been reported[13-16]. Side-to-side anastomosis has two advantages: no injury to the esophagus and no need for purse-string sutures. However, in cases of patients with a short abdominal esophagus, side-to-side anastomosis using a linear stapler would still be a difficult and complex procedure, although some length for anastomosis could be obtained through crural dissection. These methods require an expert surgeon and an assistant skilled in laparoscopic surgery.
Various end-to-side anastomosis techniques have also been consistently reported[17-19]. The key to this anastomosis is performing the purse-string suture and inserting the anvil into a fragile/contracted esophagus. Experienced surgeons can perform manual intracorporeal purse-string suturing, which facilitates simpler and safer purse-string suturing. In addition, the development of laparoscopic instruments such as Endostich® (Autosuture, Tyco Healthcare, Mansfield, MA, United States) or Endo-PSI (II) (Hope Electronics, Chiba, Japan) has reduced the difficulty of this procedure. However, there is still the inconvenience of manipulating the instruments in a narrow surgical space[20,21]. To overcome these problems, a method using an orally inserted anvil was first reported by Parker et al[22], followed by the double stapling technique using OrVilTM, which is designed for safer insertion through the esophagus[23]. In addition, Kunisaki et al[24] reported the feasibility of the OrvilTM method in their study of 30 patients. However, the method for using OrVilTM requires the cooperation of the anesthesiologist, and the esophagus can be damaged during anvil insertion. Although each technique has some disadvantages, the aforementioned techniques are useful when performing esophagojejunostomy after total gastrectomy if the operators are experienced.
Our double stapling technique allows for easy and safe anvil insertion because the anvil is introduced through the wide gastrotomy site, and the stomach becomes an inverted funnel-shape when the anvil is inserted into the esophagus. Furthermore, this technique reduces the operation time because anvil placement is completed with transection of the esophagus by the linear stapler, without performing a purse-string suture. In addition, a surgeon always needs to exercise caution to ensure that the linear stapler does not cut the stay-suture of the anvil. “Dog ear” formation can occur on the edge of the remaining esophagus after placing the anvil; however, it was not problematic for anastomosis in our experience.
Similar to our method, Omori et al[25] reported another novel double stapling technique in distal gastrectomy. The authors made an anterior incision in the residual stomach, and after inserting the anvil into the stomach, they extracted the anvil tip via the greater curvature of the stomach, with a suture at the anvil tip. Furthermore, as in our study, their technique does not require purse-string sutures for tightening the anvil. Their anvil insertion time in their study was approximately 5 min, which is not significantly different from our result (4.2 ± 1.9 min).
This technique has a weakness, the oncological safety. Because there is some risk of cancer cell spillage to the peritoneal cavity through the small gastrotomy made for this technique, careful patient selection is essential. To provide a sufficiently safe margin, we excluded patients with tumors located within 2 cm of the esophagogastric junction. In this study, the mean proximal margin of the specimen was 2.8 ± 2.1 cm, which is an acceptable result. Additionally, there was no local recurrence during the 26.8-mo follow-up period, although the long-term survival rate is unknown.
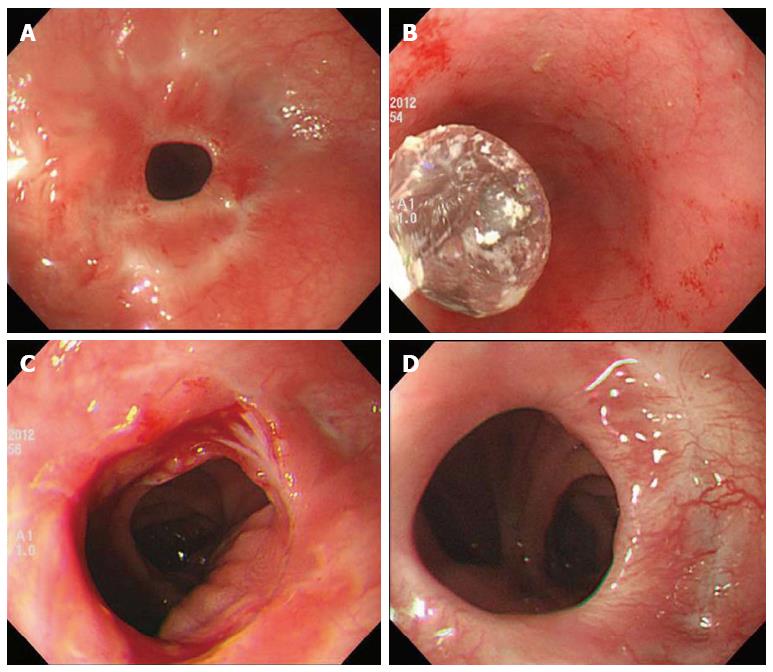
This double stapling technique was first introduced in colorectal surgery (particularly rectal cancer) for use in a narrow operative field, and its safety in colorectal surgery has already been reported and demonstrated in many studies[26-29]. Thus, the double stapling technique can be useful and time-saving for esophagojejunostomy after LTG, and recent studies have reported on its safety[23,30,31]. There was only one anastomotic stricture after discharge (a late complication), and there were no major complications, such as anastomotic leak, in the present study. The anastomotic stricture was easily managed with interventional endoscopic ballooning (Figure 6).
There may have been some selection bias because of the retrospective nature of the study; however, we tried to obtain reliable results by collecting consecutive data. Because of oncological safety, our methods cannot be applied to all patients for whom LTG is planned; however, this double stapling technique can provide easy and safe anastomosis after LTG. In particular, it can be considerable options for inexperienced surgeons, we think.
Laparoscopic gastrectomy for early gastric cancer has been accepted as the standard treatment. Although laparoscopic instrument and skill has improved in the last decade, esophagojejunostomy is still technically challenging during laparoscopic total gastrectomy.
Totally laparoscopic gastrectomy technique has been reported and these have a lot of advantages. In using circular stapler, anvil insertion is important point for safe anastomosis. But, the surgeon who has not wide experiences in laparoscopic surgery has some difficulties to perform anvil insertion to esophagus through the methods such as Orvil technique or manual purse-string suture.
The double stapling technique allows for easy and safe anvil insertion because the anvil is introduced through the wide gastrotomy site. Furthermore, this technique reduces the operation time because anvil placement is completed with transection of the esophagus by the linear stapler, without performing a purse-string suture. It can make the operative process simpler and provide more convenience to surgeon.
As mentioned above, the double stapling technique by Kim et al can provide easy and safe anastomosis during laparoscopic total gastrectomy. Consequently, it can lower the barrier to entry of laparoscopic total gastrectomy because the technique is not difficult even inexperience surgeon.
Full term of several abbreviations was described in the manuscript. Intracorporeal anastomosis is performing the anastomosis in the abdominal cavity and extracorporeal anastomosis is outside abdominal cavity.
This is an interesting, relatively simple and cost-effective approach. And the authors compliment the authors for the clear explanation of their technique and for the honest comments about the potentials and limits of this technique of esophagojejunostomy. As authors state though, it cannot be applied in tumors located very close to esophagogastric junction. The number of cases is considerable.
P- Reviewer: Forgione A, Giannopoulos GA, Song KY S- Editor: Yu J L- Editor: A E- Editor: Ma S
| 1. | Choi SM, Kim MC, Jung GJ, Kim HH, Kwon HC, Choi SR, Jang JS, Jeong JS. Laparoscopic wedge resection for gastric GIST: long-term follow-up results. Eur J Surg Oncol. 2007;33:444-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 87] [Article Influence: 4.6] [Reference Citation Analysis (1)] |
| 2. | Choi CI, Kim DH, Lee SH, Hwang SH, Jeon TY, Kim HY, Kim DH, Kim GH, Park DY. The Comparison between Laparoscopic Wedge Resection and Open Wedge Resection for Gastric Gastrointestinal Stromal Tumors. J Korean Soc Endosc Laparosc Surg. 2010;13:6-10. |
| 3. | Walther BS, Oscarson JE, Graffner HO, Vallgren S, Evander A. Esophagojejunostomy with the EEA stapler. Surgery. 1986;99:598-603. [PubMed] |
| 4. | Fujimoto S, Takahashi M, Endoh F, Takai M, Kobayashi K, Kiuchi S, Konno C, Obata G, Okui K. Stapled or manual suturing in esophagojejunostomy after total gastrectomy: a comparison of outcome in 379 patients. Am J Surg. 1991;162:256-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 5. | Jeong O, Park YK. Clinicopathological features and surgical treatment of gastric cancer in South Korea: the results of 2009 nationwide survey on surgically treated gastric cancer patients. J Gastric Cancer. 2011;11:69-77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 185] [Cited by in RCA: 190] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
| 6. | Jung YJ, Kim DJ, Lee JH, Kim W. Safety of intracorporeal circular stapling esophagojejunostomy using trans-orally inserted anvil (OrVil) following laparoscopic total or proximal gastrectomy - comparison with extracorporeal anastomosis. World J Surg Oncol. 2013;11:209. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Okabe H, Tsunoda S, Tanaka E, Hisamori S, Kawada H, Sakai Y. Is laparoscopic total gastrectomy a safe operation? A review of various anastomotic techniques and their outcomes. Surg Today. 2014;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 50] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 8. | Kim HS, Kim BS, Lee IS, Lee S, Yook JH, Kim BS. Intracorporeal laparoscopic Roux-en-Y gastrojejunostomy after 95% gastrectomy for early gastric cancer in the upper third of the stomach: a report on 21 cases. J Laparoendosc Adv Surg Tech A. 2013;23:250-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Usui S, Yoshida T, Ito K, Hiranuma S, Kudo SE, Iwai T. Laparoscopy-assisted total gastrectomy for early gastric cancer: comparison with conventional open total gastrectomy. Surg Laparosc Endosc Percutan Tech. 2005;15:309-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 77] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | Mochiki E, Toyomasu Y, Ogata K, Andoh H, Ohno T, Aihara R, Asao T, Kuwano H. Laparoscopically assisted total gastrectomy with lymph node dissection for upper and middle gastric cancer. Surg Endosc. 2008;22:1997-2002. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 99] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 11. | Bracale U, Marzano E, Nastro P, Barone M, Cuccurullo D, Cutini G, Corcione F, Pignata G. Side-to-side esophagojejunostomy during totally laparoscopic total gastrectomy for malignant disease: a multicenter study. Surg Endosc. 2010;24:2475-2479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 67] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 12. | Walther BS, Zilling T, Johnsson F, Staël von Holstein C, Joelsson B. Total gastrectomy and oesophagojejunostomy with linear stapling devices. Br J Surg. 1989;76:909-912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Matsui H, Uyama I, Sugioka A, Fujita J, Komori Y, Ochiai M, Hasumi A. Linear stapling forms improved anastomoses during esophagojejunostomy after a total gastrectomy. Am J Surg. 2002;184:58-60. [PubMed] |
| 14. | Okabe H, Obama K, Tanaka E, Nomura A, Kawamura J, Nagayama S, Itami A, Watanabe G, Kanaya S, Sakai Y. Intracorporeal esophagojejunal anastomosis after laparoscopic total gastrectomy for patients with gastric cancer. Surg Endosc. 2009;23:2167-2171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 77] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 15. | Inaba K, Satoh S, Ishida Y, Taniguchi K, Isogaki J, Kanaya S, Uyama I. Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg. 2010;211:e25-e29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 167] [Cited by in RCA: 196] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 16. | Nagai E, Ohuchida K, Nakata K, Miyasaka Y, Maeyama R, Toma H, Shimizu S, Tanaka M. Feasibility and safety of intracorporeal esophagojejunostomy after laparoscopic total gastrectomy: inverted T-shaped anastomosis using linear staplers. Surgery. 2013;153:732-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 17. | Kinoshita T, Oshiro T, Ito K, Shibasaki H, Okazumi S, Katoh R. Intracorporeal circular-stapled esophagojejunostomy using hand-sewn purse-string suture after laparoscopic total gastrectomy. Surg Endosc. 2010;24:2908-2912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 71] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 18. | Kim HI, Cho I, Jang DS, Hyung WJ. Intracorporeal esophagojejunostomy using a circular stapler with a new purse-string suture technique during laparoscopic total gastrectomy. J Am Coll Surg. 2013;216:e11-e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Sakuramoto S, Kikuchi S, Futawatari N, Moriya H, Katada N, Yamashita K, Watanabe M. Technique of esophagojejunostomy using transoral placement of the pretilted anvil head after laparoscopic gastrectomy for gastric cancer. Surgery. 2010;147:742-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 20. | Takiguchi S, Sekimoto M, Fujiwara Y, Miyata H, Yasuda T, Doki Y, Yano M, Monden M. A simple technique for performing laparoscopic purse-string suturing during circular stapling anastomosis. Surg Today. 2005;35:896-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 21. | Usui S, Nagai K, Hiranuma S, Takiguchi N, Matsumoto A, Sanada K. Laparoscopy-assisted esophagoenteral anastomosis using endoscopic purse-string suture instrument “Endo-PSI (II)” and circular stapler. Gastric Cancer. 2008;11:233-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Parker J, Sell H, Stahlfeld K. A new technique for esophagojejunostomy after total gastrectomy for gastric cancer. Am J Surg. 2001;182:174-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Jeong O, Park YK. Intracorporeal circular stapling esophagojejunostomy using the transorally inserted anvil (OrVil) after laparoscopic total gastrectomy. Surg Endosc. 2009;23:2624-2630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 149] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 24. | Kunisaki C, Makino H, Oshima T, Fujii S, Kimura J, Takagawa R, Kosaka T, Akiyama H, Morita S, Endo I. Application of the transorally inserted anvil (OrVil) after laparoscopy-assisted total gastrectomy. Surg Endosc. 2011;25:1300-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 25. | Omori T, Oyama T, Akamatsu H, Tori M, Ueshima S, Nakahara M, Toshirou N. A simple and safe method for gastrojejunostomy in laparoscopic distal gastrectomy using the hemidouble-stapling technique: efficient purse-string stapling technique. Dig Surg. 2009;26:441-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Knight CD, Griffen FD. An improved technique for low anterior resection of the rectum using the EEA stapler. Surgery. 1980;88:710-714. [PubMed] |
| 27. | Redmond HP, Austin OM, Clery AP, Deasy JM. Safety of double-stapled anastomosis in low anterior resection. Br J Surg. 1993;80:924-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 28. | Memon AA, Marks CG. Stapled anastomoses in colorectal surgery: a prospective study. Eur J Surg. 1996;162:805-810. [PubMed] |
| 29. | Fu CG, Muto T, Masaki T. Results of the double stapling procedure in colorectal surgery. Surg Today. 1997;27:706-709. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 30. | Tejero Cebrián E, Ratia Giménez T, Fernández Fernández L, Tieso Herreros A, Jorge Sanchez E. Double-stapling technique for mechanical circular oesophagojejunal anastomosis after total gastrectomy. Br J Surg. 1994;81:408-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 31. | Ohdaira H, Noro T, Terada H, Kameyama J, Ohara T, Yoshino K, Kitajima M, Suzuki Y. New double-stapling technique for esophagojejunostomy and esophagogastrostomy in gastric cancer surgery, using a peroral intraluminal approach with a digital stapling system. Gastric Cancer. 2009;12:101-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |