Published online Feb 7, 2014. doi: 10.3748/wjg.v20.i5.1340
Revised: September 24, 2013
Accepted: September 29, 2013
Published online: February 7, 2014
Processing time: 189 Days and 18 Hours
AIM: To investigate the accuracy of Endoscopic ultrasound (EUS) in staging and sub-staging T1a and T1b esophageal squamous cell carcinoma (ESCC).
METHODS: A retrospective analysis involving 72 patients with pathologically confirmed T1a or T1b ESCC, was undertaken between January 2005 and December 2011 in Sun Yat-sen University Cancer Center. The accuracy and efficiency of EUS for detecting stages T1a and T1b ESCC were examined.
RESULTS: The overall accuracy of EUS for detecting stage T1a or T1b ESCC was 70.8% (51/72), and the sensitivity was 74.3%. 77.8% (7/9) of lesions originated in the upper thoracic region, 73.1% (38/52) in the mid-thoracic region and 72.7% (8/11) in the lower thoracic region. Multivariate analysis revealed that the diagnostic accuracy of EUS was closely related to lesion length (F = 4.984, P = 0.029).
CONCLUSION: EUS demonstrated median degree of accuracy for distinguishing between stages T1a and T1b ESCC. Therefore, it is necessary to improve EUS for staging early ESCC.
Core tip: Endoscopic ultrasound (EUS) is the best option for staging early esophageal squamous cell carcinoma (ESCC). However, the accuracy of EUS for staging ESCC is not good and diverse. There is no other report about sub-staging T1 disease as T1a or T1b by EUS for ESCC. This study indicated that accuracy demonstrated by EUS for sub-staging T1a and T1b ESCC was only about 70%. Therefore, the technique of EUS requires further refinement to enhance its diagnostic accuracy for staging early ESCC. The results in this study indicated that EUS can stage and sub-stage early ESC pre-operatively whereas this modality need to be improved.
- Citation: He LJ, Shan HB, Luo GY, Li Y, Zhang R, Gao XY, Wang GB, Lin SY, Xu GL, Li JJ. Endoscopic ultrasonography for staging of T1a and T1b esophageal squamous cell carcinoma. World J Gastroenterol 2014; 20(5): 1340-1347
- URL: https://www.wjgnet.com/1007-9327/full/v20/i5/1340.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i5.1340
In accordance with the American Joint Committee on Cancer (AJCC) TNM classification of carcinoma of the esophagus and the esophageal-gastric junction (7th edition, 2010), the T1 stage of esophageal squamous carcinoma (ESCC) is subdivided into T1a (the tumor has infiltrated into the mucosal lamina propria and muscularis mucosa) and T1b (the tumor has infiltrated into the submucosa)[1,2]. Lymph node metastases occur in approximately 3%-6% of T1a cases, and T1a cancers can be removed surgically or with endoscopic treatments such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection, both of which have advantages of less damage and lower cost than esophagectomy[3-5]. In contrast, lymph node metastases occur in 21%-24% of those with T1b stage of ESCC, and these patients are not suitable for endoscopic treatment and require surgical resection[4-8]. Therefore, identifying the lesion stage of ESCC prior to treatment is essential.
The T staging classification depends mainly on the depth of the infiltration and the extent of damage to histological layers. At present, the most effective method for diagnosing and defining ESCC is endoscopic ultrasonography (EUS)[9,10]. EUS delivers the ultrasound probe via endoscopy and directly observes echoes in different layers of the digestive tract wall, and therefore, the depth of lesion infiltration and the extent of damage in different layers can be relatively easily visualized using this approach. In contrast, methods such as computed tomography (CT), magnetic resonance imaging (MRI) and positron emission computed tomography (PET-CT) cannot provide an accurate assessment of the different layers of the esophageal wall. In addition, the accuracy of EUS for T1 staging in ESCC is greater than that of other methods[11-13]. A meta-analysis demonstrated that the sensitivities of EUS in stages T1, T2, T3 and T4 are 81.6%, 81.4%, 91.4% and 92.4%, with corresponding specificities of 99.4%, 96.3%, 94.4% and 97.4%, respectively. However, there are few reports that have distinguished between T1a and T1b stages of ESCC using EUS[14]. In addition, this meta-analysis enrolled most pathological types of esophageal carcinoma, including adenocarcinoma, adenosquamous carcinoma and sarcoma, but there was a paucity of data concerning ESCC[15-17]. Due to the importance of preoperative staging in patients with stage T1a or T1b ESCC, a statistical analysis of the accuracy of EUS for identifying specific stages is needed[18,19]. This study focused on the role of EUS in distinguishing between the T1a and T1b stages of ESCC, to facilitate accurate preoperative assessment and more reliable decision-making on the appropriateness of endoscopic treatment or surgical resection.
From January 2005 to December 2011, 72 ESCC patients who underwent endoscopic treatment or surgical resection and whose cancers were confirmed as T1N0M0 post-operatively were enrolled. Then, we retrospectively compared the preoperative EUS stages with the pathological results. The study protocol was approved by the institutional review board. All patients provided written informed consent before preoperative EUS examination.
In addition, to compare the accuracy of EUS for staging early and advanced ESCC, 90 randomly chosen patients with non-T1 ESCC (30 cases each of T2, T3 and T4, all confirmed post-operatively) were also enrolled.
An Olympus GF-UM2000 EndoEcho Ultrasonic Gastrovideoscope was used for the study, and the EUS transducer offered four frequency modes, 5.0, 7.5, 12.0 and 20 MHz, to suit the clear-view requirement. Esophageal lesions were observed using the balloon method and the sterile deaerated water immersion method. All enrolled cases were observed using EUS with 7.5 and 12 MHz probes. The EUS examinations were performed by two experts in endoscopy, both of whom had at least 10 years of experience in Sun Yat-sen University Cancer Center. Both the balloon method and the water immersion method were performed during EUS examination.
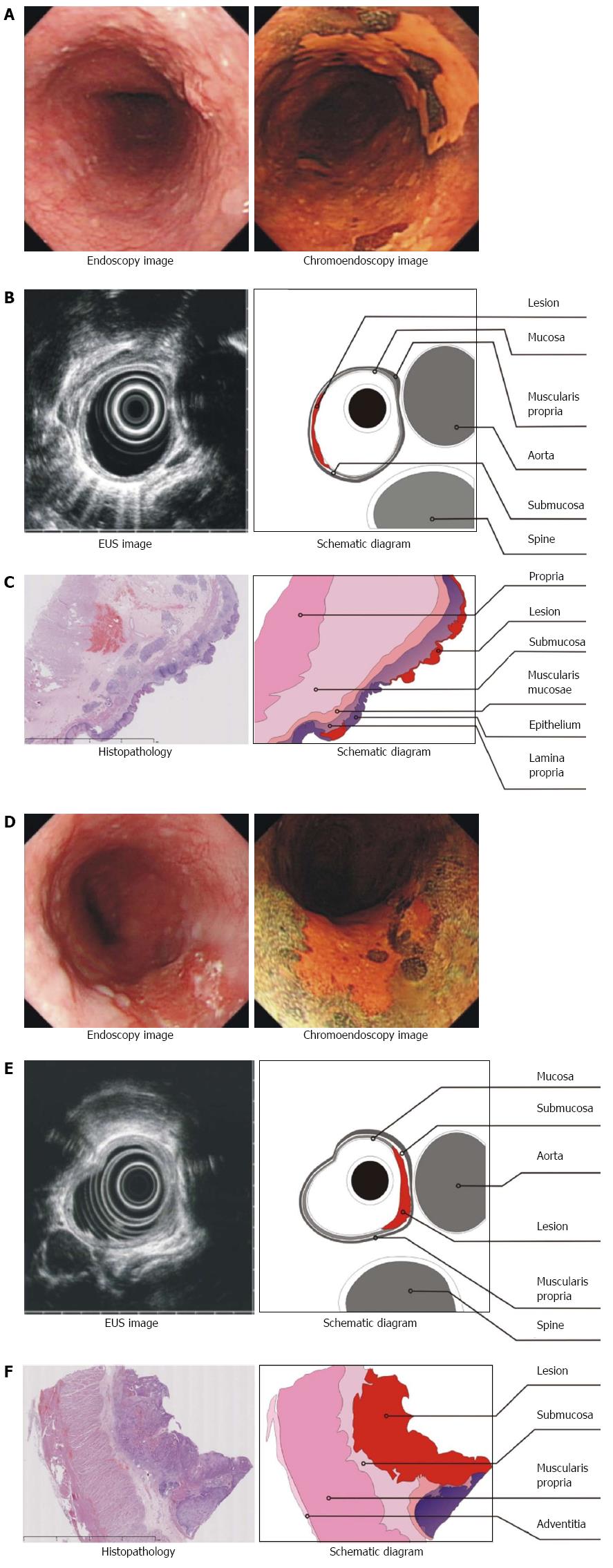
Lightdale et al[20] stated that the esophageal wall can be divided into five layers by ultrasound. The first layer is a high echogenic band, which represents the interface echo of the mucosa; the second layer is a low echogenic band, which represents the muscularis mucosae; the third layer is a high echogenic band, which represents the submucosa; the fourth layer is a low echogenic band, which represents the muscularis propria; and the fifth layer is a high echogenic band, which represents the serosal layer, or the adventitia and the interface. Therefore, with EUS, ultrasonic images of stage T1a ESCC can identify significant thickening of the first and/or second layers, as well as an intact third layer. In contrast, the imaging of stage T1b ESCC shows continuous infiltration from the first to the third layer; the third layer becomes narrower, and the fourth layer remains complete or intact. Two experts in endoscopy conducted staging for all patients independently, thus creating two sets of staging data. When the results of both sets were consistent, the data were used in the analysis. When the results were not consistent, the experts discussed and read the images together to obtain a third common set of results.
Data from the two independent assessors were statistically compared using SPSS version 13.0 software (SPSS Inc., Chicago, IL).
Numerical data are expressed as frequencies and percentages. A statistical descriptive method was used to analyze EUS evaluation indices for the clinical value of preoperative T and N staging of ESC, and this analysis included the diagnostic accuracy (AC), sensitivity (SE), false positive rate (FPR), false negative rate (FNR), specificity (SP), positive predictive value (PPV) and negative predictive value (NPV). The χ2 test was used to analyze interclass differences in numerical data between the EUS and pathological results.
There were 47 males (65.3%) and 25 females (34.7%) with T1 ESCC. Their ages varied from 37 to 78 years, with a median of 58 years. Pathological examination revealed that 35 patients had stage T1a (48.61%) disease and 37 patients had stage T1b (51.39%) disease. Pathologically, there were 26 cases of carcinoma in situ (36.11%), six cases of well-differentiated squamous cell carcinoma (8.33%), 30 cases of moderately differentiated (41.67%), and 10 cases of poorly differentiated (13.89%). Regarding lesion location, 9 patients had lesions in the upper esophagus (12.50%), 52 had lesions in the mid-esophagus (72.22%), and 11 had lesions in the lower esophagus (15.28%) (Table 1).
Based on EUS results, the first expert concluded that 36 cases were stage T1a and 36 cases were stage T1b (Figure 1). Pathological results confirmed an AC of 65.3% (47/72), SE of 65.7%, FPR of 35.1%, FNR of 34.3%, SP of 64.9%, PPV of 63.9% and NPV of 66.7%. The area under the curve (AUC) was 0.668 (P = 0.014). The second expert concluded that 39 cases were stage T1a and 33 were T1b, with an AC of 66.7% (48/72), SE of 64.1%, FPR of 35.9%, FNR of 30.3%, SP of 69.7%, PPV of 71.4%, NPV of 62.2% and an AUC of 0.668 (P = 0.014). However, the combined assessment concluded that 36 cases were stage T1a and 36 were stage T1b. Pathological results confirmed an AC of 70.8% (51/72), SE of 74.3%, FPR of 27.0%, FNR of 25.7%, SP of 73.0%, PPV of 72.2%, NPV of 75.0% and AUC of 0.736 (P = 0.001, Table 2). These results indicate that EUS is a valid method for diagnosing and identifying stages T1a and T1b disease.
| Pathology | Expert 1 | Expert 2 | Common results | ||
| T1a (n = 36) | T1b (n = 36) | T1a (n = 39) | T1b (n = 33) | T1a (n = 36) | |
| T1a (n = 35) | 23 | 13 | 25 | 10 | 26 |
| T1b (n = 37) | 13 | 24 | 14 | 23 | 10 |
| Group | |||||
| AC | 65.30% | 66.70% | 70.80% | ||
| SE | 65.70% | 64.10% | 74.30% | ||
| FPR | 35.10% | 35.90% | 27.00% | ||
| FNR | 34.30% | 30.30% | 25.70% | ||
| SP | 64.90% | 69.70% | 73.00% | ||
| PPV | 63.90% | 71.40% | 72.20% | ||
| NPV | 66.70% | 62.20% | 75.00% | ||
| AUC | 0.653 | 0.668 | 0.736 | ||
| P value | 0.026 | 0.014 | 0.001 | ||
We conducted statistical analyses of the impact of tumor site on EUS staging accuracy for T1 stage ESCC. The combined set of common results revealed that for ESC in the upper thoracic region, EUS had an AC of 77.8% (7/9), SE of 80.0%, SP of 75.0%, PPV of 80.0% and NPV of 77.8%. For ESCC in the middle thoracic region, EUS had an AC of 73.1% (38/52), SE of 68.0%, SP of 77.8%, PPV of 73.9% and NPV of 72.4%. Finally, for ESC in the lower thoracic region, EUS had an AC of 72.7% (8/11), SE of 83.3%, SP of 60.0%, PPV of 71.4% and NPV of 75.0%. Furthermore, when compared with the combined set of common results, data obtained by the experts individually were not significantly better (Table 3).
| Site of neoplasm | Expert 1 | Expert 2 | Common results | ||||
| T1a | T1b | T1a | T1b | T1a | T1b | ||
| Upper third | T1a | 4 | 2 | 4 | 2 | 4 | 1 |
| T1b | 1 | 2 | 1 | 2 | 1 | 3 | |
| Mid third | T1a | 14 | 10 | 16 | 11 | 17 | 8 |
| T1b | 9 | 19 | 7 | 18 | 6 | 21 | |
| Lower third | T1a | 5 | 1 | 5 | 1 | 5 | 1 |
| T1b | 2 | 3 | 2 | 3 | 2 | 3 | |
| Group | |||||||
| AC | Upper third | 66.7% | 66.7% | 77.8% | |||
| Mid third | 63.50% | 65.40% | 73.10% | ||||
| Lower third | 72.70% | 72.70% | 72.70% | ||||
| SE | Upper third | 66.70% | 66.70% | 80.00% | |||
| Mid third | 58.30% | 59.30% | 68.00% | ||||
| Lower third | 83.30% | 83.30% | 83.30% | ||||
| FPR | Upper third | 66.70% | 66.70% | 75.00% | |||
| Mid third | 67.90% | 72.00% | 77.80% | ||||
| Lower third | 60.00% | 60.00% | 60.00% | ||||
| FNR | Upper third | 80.00% | 80.00% | 80.00% | |||
| Mid third | 60.90% | 69.60% | 73.90% | ||||
| Lower third | 71.40% | 71.40% | 71.40% | ||||
| SP | Upper third | 50.00% | 50.00% | 75.30% | |||
| Mid third | 65.50% | 62.10% | 72.40% | ||||
| Lower third | 75.00% | 75.00% | 75.00% | ||||
A multivariate statistical analysis of the accuracy of the distinguishing set was conducted (Table 4). The accuracy was closely related to tumor length (F = 4.984, P = 0.029) but not to tumor width (all P values > 0.05).
| Characteristics | Hazards ratio | P value |
| Age ( ≤ 58 vs > 58 yr) | 1.240 | 0.269 |
| Sex (male vs female) | 0.923 | 0.340 |
| Tumor width, cm ( ≤ 2 vs > 2) | 1.407 | 0.240 |
| Tumor length, cm ( ≤ 2 vs > 2) | 4.984 | 0.0291 |
| Differentiation (well-moderate vs poor) | 2.815 | 0.098 |
Given that the images of those with stage T1 and those with non-stage T1 disease were randomly arranged, the experts evaluated the images together. The combined set of common results had an AC of 93.21% (151/162), PPV of 92.5% and NPV of 92.8%. Among the 11 cases that were misdiagnosed, 7 cases with stage T1 were misdiagnosed and were re-staged based on the pathological results: 2 cases were T1a and 5 cases were T1b disease. Four patients in the non-stage T1 group were misdiagnosed as stage T1, and the pathological results showed that all 4 cases were stage T2 disease. These results demonstrate that EUS has a high accuracy and reliability for distinguishing stage T1 ESCC from non-T1 ESCC.
Early diagnosis and treatment are keys to reducing the morbidity and mortality associated with ESCC. With recent developments in endoscopic techniques, endoscopic treatment has become a standard first-line management strategy for early ESCC and precancerous lesions. However, due to significant differences in the presence of lymph node metastases and the prognosis of patients with stage T1a ESCC compared to those with stage T1b ESCC, accurate staging is necessary to choose the most appropriate treatment. The 2011 NCCN Guidelines state that stage T1a esophageal cancer (EC) is an indication for endoscopic treatment. Because imaging methods such as CT, MRI, and PET-CT cannot distinguish the layers of the esophageal wall, they are unable to accurately distinguish between T1a and T1b. Preoperative EUS can provide accurate information on echoes, the depth of lesion infiltration, and even the interface between the esophageal wall layers. Therefore, EUS is widely used clinically so that the most appropriate treatment can be chosen[21].
Pech et al[22] demonstrated an EUS accuracy of 92% for diagnosing stage T1 EC, which was higher than the reported accuracy for stages T3 and T4. This is essentially consistent with our results (93.21%). This observation may be explained by the fact that in stage T1, the extent of tumor infiltration ranges from the first layer to the third layer, and these three layers, particularly the submucosa, are relatively thick and significantly different from the muscular layer in terms of echo grayscale. Therefore, EUS has a high accuracy for evaluating early tumor infiltration. Hence, we believe that EUS is reliable for staging T1 ESCC. However, few studies have focused on the accuracy of EUS for sub-staging T1 esophageal carcinoma. There has been only one relevant study[17], which reported an accuracy of 86% (19/22) for stage T1a and an accuracy of 60% (22/33) for stage T1b. However, of the 55 cases in that study, 33 were adenocarcinomas, of which, 27 had developed from Barrett’s esophagus, and most of the EUS images showed thickening of the muscularis mucosae rather than the mucosal layer. Our study, on the other hand, focused on ESCC, which is a tumor that has a high occurrence rate in South China, generally develops in the mucosal layer and gradually infiltrates into the submucosa. Therefore, reliable statistical data about the accuracy of EUS for diagnosing ESCC stages T1a and T1b are needed, and some possible clinical and pathological factors that may impact the diagnostic accuracy of EUS should be considered.
Because relatively few patients with ESCC have stage T1N0M0 disease, our retrospective study enrolled only 72 cases from 2005 to 2011. Both endoscopists had 10 years of experience in endoscopic diagnosis, and their individual assessments revealed similar figures in terms of accuracy of diagnosis (65.3% vs 66.7%). In addition, data on accuracy from the combined assessment did not reveal a significant increase (70.8%, P > 0.05). Low diagnostic accuracy might be explained by a few reasons[23]. First, the esophageal wall is thin, and it is difficult to distinguish the boundaries of various layers according to the gray scale in EUS images alone. Second, the boundaries in EUS images are actually the reflections of the interfaces between various layers, and there is little difference between the actual anatomical structure and the echoic gray scale of EUS. Third, the two experts made the diagnosis through static images, without consistent and dynamic ultrasonic images. Moreover, this study focused on early ESCC, yet previous reports included all pathological types, such as squamous carcinoma, adenocarcinoma, adenosquamous carcinoma and sarcoma. Additionally, in most early ESCC patients, inflammation was present around the lesions, especially in the lower esophagus (e.g., the impact of reflux esophagitis), resulting in changes in the layers of the esophageal wall (particularly when shown as thickening of the esophageal submucosa), which may have an impact on diagnosis.
In addition, we found that the accuracy of EUS for staging T1 was related to tumor site and length. The diagnostic accuracy of both experts was lower for lesions in the middle section than in the upper and lower sections. The common results revealed that the diagnostic accuracy of lesions in the middle section increased to 73.1%, which was slightly higher than the accuracy observed for the lower section (72.7%), but still lower than the accuracy of for the upper section (77.8%). We believe that this difference may be explained by several factors. First, a minority of ESCC cases originated in the upper and lower sections (9 and 11, respectively), which may have adversely affected the statistical accuracy. Second, the data also showed that T staging of ESCC in the middle section was more difficult, and both experts had lower accuracy rates in this area (63.5% and 65.4%), which necessitated negotiation or discussion (which generated the common results) that increased the accuracy rate (73.1%). Third, because the esophagus is relatively wide in its thoracic section, it is difficult to fill the lumen with water during EUS examination; therefore, it is hard for the ultrasonic probe to get close to the lesion. Finally, the middle section of the esophagus is near the left atrium of the heart and the thoracic aorta[24,25], both of which pulsate and make it difficult to image. Consequently, T1 staging of ESCC in the middle section is more difficult. Furthermore, our multivariate statistical analysis demonstrated that accuracy was related to tumor length (maximum vertical axis of parallel esophagus) (P = 0.029), but not to tumor width (maximum vertical axis of vertical esophagus) or the degree of differentiation (P = 0.098). This result may be explained by the fact that when the tumor is long, the ultrasonic probe has to be moved backwards and forwards to visualize the lesion. At present, circle-scan probes are used in most clinical situations, which can comprehensively scan tumor width, and thus, width does not necessarily affect diagnostic accuracy.
Our team had tried to employ submucosal saline injection (a novel technique) to improve EUS for staging and sub-staging early ESCC. The preliminary results revealed that the accuracy of SSI + EUS for staging or substaging early ESCC increased significantly[26,27].
In conclusion, EUS plays an important role in defining the T stage of ESCC. However, accurately staging early ESCC as T1a or T1b is difficult using EUS alone, especially when the lesion is located in the mid-thoracic section. Therefore, EUS as a technique needs to be improved to distinguish T1a and T1b disease in patients with early ESCC.
Correct staging and sub-staging of early esophageal squamous cell carcinoma (ESCC) is of great importance for guiding therapy. Endoscopic ultrasound (EUS) is the most common modality for staging early ESCC.
However, the accuracy of EUS for staging ESCC is not good and diverse. In addition, there is no other report about sub-staging T1 disease as T1a or T1b by EUS for ESCC.
This study investigated whether EUS can distinguish between T1a and T1b ESCC. The results indicated that accuracy demonstrated by EUS for sub-staging T1a and T1b ESCC was only about 70%. Therefore, the technique of EUS requires further refinement to enhance its diagnostic accuracy for staging early ESCC.
The results in this study revealed that EUS can stage and sub-stage early ESCC preoperatively whereas EUS should be improved to better stage early ESCC.
This is a retrospective study for diagnostic value of EUS for early esophageal cancer with squamous cell carcinoma. The authors concluded that EUS demonstrated median degree of accuracy for distinguishing between T1a and T1b ESCC, and so it is necessary to improve EUS for staging and sub-stage early ESCC.
P- Reviewers: Bassotti G, Farmer AD, Kim GH S- Editor: Qi Y L- Editor: Wang TQ E- Editor: Zhang DN
| 1. | Union for International Cancer Control (UICC). TNM Classification of Malignant Tumors. 7th ed. Oxford: Wiley-Blackwell 2009; 15-18. |
| 2. | National Comprehensive Cancer Network (NCCN). NCCN practice guidline for oncology (esophageal and esophagogastric junction cancer) version 2. 2011; Available from: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#site. |
| 3. | Higuchi K, Tanabe S, Koizumi W, Sasaki T, Nakatani K, Saigenji K, Kobayashi N, Mitomi H. Expansion of the indications for endoscopic mucosal resection in patients with superficial esophageal carcinoma. Endoscopy. 2007;39:36-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 59] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 4. | Nealis TB, Washington K, Keswani RN. Endoscopic therapy of esophageal premalignancy and early malignancy. J Natl Compr Canc Netw. 2011;9:890-899. [PubMed] |
| 5. | Lee JH, Hong SJ, Jang JY, Kim SE, Seol SY. Outcome after endoscopic submucosal dissection for early gastric cancer in Korea. World J Gastroenterol. 2011;17:3591-3595. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Saito Y, Takisawa H, Suzuki H, Takizawa K, Yokoi C, Nonaka S, Matsuda T, Nakanishi Y, Kato K. Endoscopic submucosal dissection of recurrent or residual superficial esophageal cancer after chemoradiotherapy. Gastrointest Endosc. 2008;67:355-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 7. | Othman MO, Wallace MB. Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) in 2011, a Western perspective. Clin Res Hepatol Gastroenterol. 2011;35:288-294. [PubMed] |
| 8. | Kwee RM, Kwee TC. Imaging in local staging of gastric cancer: a systematic review. J Clin Oncol. 2007;25:2107-2116. [PubMed] |
| 9. | Mortensen MB, Edwin B, Hünerbein M, Liedman B, Nielsen HO, Hovendal C. Impact of endoscopic ultrasonography (EUS) on surgical decision-making in upper gastrointestinal tract cancer: an international multicenter study. Surg Endosc. 2007;21:431-438. [PubMed] |
| 10. | Thosani N, Singh H, Kapadia A, Ochi N, Lee JH, Ajani J, Swisher SG, Hofstetter WL, Guha S, Bhutani MS. Diagnostic accuracy of EUS in differentiating mucosal versus submucosal invasion of superficial esophageal cancers: a systematic review and meta-analysis. Gastrointest Endosc. 2012;75:242-253. [PubMed] |
| 11. | Subasinghe D, Samarasekera DN. A study comparing endoscopic ultrasound (EUS) and computed tomography (CT) in staging oesophageal cancer and their role in clinical decision making. J Gastrointest Cancer. 2010;41:38-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Margetts BM, Barker DJ, Kavanagh JP, Blacklock NJ. Do stone formers have lower urinary fibrinolytic activity than controls? Br J Urol. 1990;66:581-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Quint LE, Bogot NR. Staging esophageal cancer. Cancer Imaging. 2008;8 Spec No A:S33-S42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Puli SR, Reddy JB, Bechtold ML, Antillon D, Ibdah JA, Antillon MR. Staging accuracy of esophageal cancer by endoscopic ultrasound: a meta-analysis and systematic review. World J Gastroenterol. 2008;14:1479-1490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 243] [Cited by in RCA: 246] [Article Influence: 14.5] [Reference Citation Analysis (2)] |
| 15. | Crabtree TD, Yacoub WN, Puri V, Azar R, Zoole JB, Patterson GA, Krupnick AS, Kreisel D, Meyers BF. Endoscopic ultrasound for early stage esophageal adenocarcinoma: implications for staging and survival. Ann Thorac Surg. 2011;91:1509-1515; discussion 1509-1515. [PubMed] |
| 16. | Young PE, Gentry AB, Acosta RD, Greenwald BD, Riddle M. Endoscopic ultrasound does not accurately stage early adenocarcinoma or high-grade dysplasia of the esophagus. Clin Gastroenterol Hepatol. 2010;8:1037-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 102] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Thomas T, Gilbert D, Kaye PV, Penman I, Aithal GP, Ragunath K. High-resolution endoscopy and endoscopic ultrasound for evaluation of early neoplasia in Barrett’s esophagus. Surg Endosc. 2010;24:1110-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Shimpi RA, George J, Jowell P, Gress FG. Staging of esophageal cancer by EUS: staging accuracy revisited. Gastrointest Endosc. 2007;66:475-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Moss A, Bourke MJ, Hourigan LF, Gupta S, Williams SJ, Tran K, Swan MP, Hopper AD, Kwan V, Bailey AA. Endoscopic resection for Barrett’s high-grade dysplasia and early esophageal adenocarcinoma: an essential staging procedure with long-term therapeutic benefit. Am J Gastroenterol. 2010;105:1276-1283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 144] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 20. | Lightdale CJ, Kulkarni KG. Role of endoscopic ultrasonography in the staging and follow-up of esophageal cancer. J Clin Oncol. 2005;23:4483-4489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 127] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 21. | Tokar JL, Haluszka O, Weinberg DS. Endoscopic therapy of dysplasia and early-stage cancers of the esophagus. Semin Radiat Oncol. 2007;17:10-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Pech O, Günter E, Dusemund F, Origer J, Lorenz D, Ell C. Accuracy of endoscopic ultrasound in preoperative staging of esophageal cancer: results from a referral center for early esophageal cancer. Endoscopy. 2010;42:456-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 96] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 23. | Kutup A, Link BC, Schurr PG, Strate T, Kaifi JT, Bubenheim M, Seewald S, Yekebas EF, Soehendra N, Izbicki JR. Quality control of endoscopic ultrasound in preoperative staging of esophageal cancer. Endoscopy. 2007;39:715-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 55] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 24. | Rampado S, Bocus P, Battaglia G, Ruol A, Portale G, Ancona E. Endoscopic ultrasound: accuracy in staging superficial carcinomas of the esophagus. Ann Thorac Surg. 2008;85:251-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 66] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 25. | Peng GY, Wu YW, Long QL, Chen L, Zhao JJ, Li XH. A new endoscopic classification system of early-stage esophageal carcinoma and its usefulness in assessing the infiltration depth of esophageal carcinoma. Cancer Invest. 2011;29:167-172. [PubMed] |
| 26. | Li JJ, Shan HB, Gu MF, He L, He LJ, Chen LM, Luo GY, Xu GL. Endoscopic ultrasound combined with submucosal saline injection for differentiation of T1a and T1b esophageal squamous cell carcinoma: a novel technique. Endoscopy. 2013;45:667-670. [PubMed] |
| 27. | Li JJ, Shan HB, Xu GL, He LJ, Xia JC. Submucosal saline solution injection combined with endosonography for distinguishing between stages T1a and T1b of early esophageal cancer. Gastrointest Endosc. 2013;77:159-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |