Published online Nov 28, 2014. doi: 10.3748/wjg.v20.i44.16698
Revised: June 13, 2014
Accepted: July 11, 2014
Published online: November 28, 2014
Processing time: 246 Days and 16.8 Hours
AIM: To assess the diagnostic accuracy of computed tomographic venography (CTV) for splanchnic vein thrombosis (SVT) detection in necrotizing acute pancreatitis (AP) patients.
METHODS: Forty-three patients with necrotizing AP who underwent both CTV and digital subtraction angiography (DSA) within 3 d were analyzed in this retrospective comparative study. All CTV procedures were performed with a dual-source CT scanner. The presence and location of SVT were determined via blinded imaging data analyses.
RESULTS: According to the DSA results, 17 (39.5%) of the total 43 patients had SVT. The sensitivity, specificity, positive and negative predictive values of CTV for SVT detection were 100% (95%CI: 77.1%-100%), 92.3% (95%CI: 73.4%-98.7%), 89.5% (95%CI: 65.5%-98.2%) and 100% (95%CI: 82.8%-100%), respectively.
CONCLUSION: CTV is an effective examination for SVT detection in patients with necrotizing AP with high positive and negative predictive values.
Core tip: Computed tomographic venography (CTV) is an effective examination for splanchnic vein thrombosis (SVT) detection in necrotizing acute pancreatitis (AP) with high positive and negative predictive values. As a non-invasive and quick procedure, CTV might effectively replace digital subtraction angiography and be the routine imaging method for screening and assessing SVT in necrotizing AP patients.
- Citation: Jiang W, Zhou J, Ke L, Li G, Tong ZH, Li WQ, Li JS. Splanchnic vein thrombosis in necrotizing acute pancreatitis: Detection by computed tomographic venography. World J Gastroenterol 2014; 20(44): 16698-16701
- URL: https://www.wjgnet.com/1007-9327/full/v20/i44/16698.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i44.16698
As a well-recognized acute pancreatitis (AP) complication, splanchnic vein thrombosis (SVT) may lead to severe clinical consequences such as hemorrhage due to local portal hypertension and the formation of gastric varices, small bowel ischemia due to superior mesenteric vein (SMV) occlusion, and hepatic failure due to portal vein (PV) occlusion[1-3]. In previous studies, the incidence of SVT varied from 1% to 24% depending on the severity of the study population and the detecting technique that was utilized[1]. SVT is more often associated with necrotizing acute pancreatitis and a recent study showed that SVT was associated with the presence, location, and extent of pancreatic necrosis[4].
With the development of computed tomography (CT) techniques as non-invasive and quick examinations, computed tomographic venography (CTV) has become a routine procedure for assessing the abdominal vascular system, such as collateral vessels[5,6]. Few studies, however, have evaluated the effectiveness of this technique for SVT detection in necrotizing AP patients. In our study, we aimed to assess the diagnostic accuracy of CTV for SVT detection in necrotizing AP as compared with digital subtraction angiography (DSA).
We reviewed data from patients diagnosed with necrotizing AP in our center from July 1, 2011 to June 30, 2013. Those who underwent both CTV and DSA within 3 d were included in this study. AP was diagnosed according to clinical presentation (typically abdominal pain), laboratory parameters (serum amylase or lipase levels that exceeded three times the normal upper limit) and abdominal imaging by contrast-enhanced CT (CECT). The severity and pancreatic or peripancreatic necrosis were defined according to the Determinant-Based Classification of Acute Pancreatitis Severity[7]. Patients with chronic pancreatitis, malignancy and cirrhosis were excluded. The study center was a tertiary referral pancreatic critical center at Jinling Hospital, Nanjing, and the local research ethics committee approved the study.
All CTV procedures were performed with a dual-source CT scanner (Somatom Definition, Siemens Medical Solutions). A non-contrast CT scan of the entire abdomen was initially performed. Then, 70 mL of iopromide (Ultravist; 300 mg I/mL, Bayer Schering Pharma, Berlin, Germany) was injected with a power injector at a rate of 3 mL/s via an 18 gauge catheter that was typically positioned in the antecubital vein. Arterial and portal venous phase images were acquired at a 25 s and 60 s delay from the start of the intravenous contrast injection, respectively. Axial images were reconstructed with a slice thickness of 1.25 mm at an interval of 0.625 mm and were stored for analysis.
Patients underwent DSA for a continuous regional arterial infusion, for hemorrhage spot detection or when there was a significant clinical SVT manifestation such as ascites. DSA was performed using Seldinger technique through the femoral artery with a biplane digital subtraction angiography unit (Axiom Artis dTA; Siemens Healthcare). After selective catheterization of the splenic, superior mesenteric and inferior mesenteric arteries, 25-40 mL of iopromide (Ultravist; 300 mg I/mL, Bayer Schering Pharma) was injected with a power injector at a rate of 5-10 mL/s via a 5 F catheter. The views were acquired during the hepatic arterial and portal venous phases for analysis.
All image resources were stored on a commercial workstation (Syngo VE32E, Siemens Medical Solutions). Two experienced gastrointestinal radiologists who were blinded to the clinical and DSA data, reviewed all of the CT data separately. An experienced interventional radiologist and an experienced endovascular gastrointestinal surgeon who were blinded to the clinical and CT data, reviewed all of the DSA data separately. The presence and location of the SVT were assessed, and any diagnostic differences between the two doctors were resolved by a discussion after which a consensus on the results was reached.
The data analyses were performed using SPSS 20.0 (IBM SPSS Statistics; IBM Corporation). In our study, with DSA as the comparison, the sensitivity, specificity, positive predictive value, and negative predictive values of CTV were determined, and 95% confidence intervals (CIs) were calculated according to the efficient-score model. A kappa value was used to quantify the inter-reader agreement for detecting the presence of SVT by CTV and DSA. A P value < 0.05 was regarded as statistically significant (two-tailed test).
Between July 1, 2011 and June 30, 2013, of all the 358 patients with clinical, laboratory, or radiographic AP evidence, 43 with pancreatic or peripancreatic necrosis underwent CTV and DSA within 3 d. Their mean age was 44.6 ± 13.3 years, and 30 (69.8%) of them were male. Twenty-seven (62.8%) patients had critical AP, 5 (11.6%) had severe AP, and 11 (25.6%) had moderate AP.
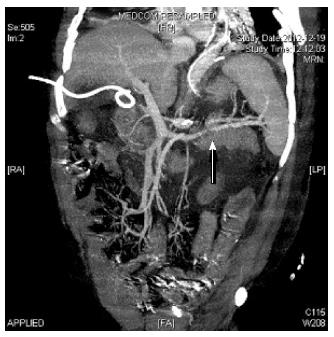
According to the DSA results, 17 (39.5%) of the 43 total patients had SVT (the SVT locations and numbers are presented in Table 1), while according to the CTV results, 19 (44.2%) patients had SVT. CTV identified all of the DSA-positive cases, but it also resulted in 2 false-positive diagnoses. Figure 1 shows a typical example of SVT identified by CTV. One was diagnosed as a multiple filling defect, and the other was not clearly displayed by CTV. Thus, the CTV positive predictive and negative predictive values for SVT detection were 89.5% (95%CI: 65.5%-98.2%), and 100% (95%CI: 82.8%-100%), respectively (Table 2). The κ value was 0.91, which indicated an excellent inter-reader agreement.
| Location of SVT | No. of patients |
| PV isolated | 1 |
| SplV isolated | 7 |
| SMV isolated | 5 |
| SMV + PV | 1 |
| PV + SplV | 0 |
| SplV + SMV | 2 |
| SMV + PV + SplV | 1 |
| Findings | Positive (DSA) | Negative (DSA) | Total |
| Positive (CTV) | 17 | 2 | 19 |
| Negative (CTV) | 0 | 24 | 24 |
| Total | 17 | 26 | 43 |
| Sensitivity | 100% (95%CI: 77.1%-100%) | ||
| Specificity | 92.3% (95%CI: 73.4%-98.7%) | ||
| Positive predictive value | 89.5% (95%CI: 65.5%-98.2%) | ||
| Negative predictive value | 100% (95%CI: 82.8%-100%) | ||
In our study, we observed that SVT has a high incidence in patients with necrotizing AP, and CTV has high positive and negative predictive values for detecting SVT. That finding suggests that CTV could serve as an alternative examination for screening and assessing SVT in this entity.
The incidence of SVT for all AP patients is relatively low, and the complications directly related to SVT are rare[4,8]. However, perivascular inflammation and compression by peripancreatic collections or pancreatic necrosis increase the frequency of SVT[1,2]. A retrospective study recently showed that 53% of patients with necrosis developed SVT[4]. Our study suggested that approximately 4 out of 10 patients with necrotizing AP have SVT.
It has been reported that SVT can lead to hemorrhage, bowel ischemia, and liver failure, but the signs and symptoms may overlap with those of pancreatitis[2,9]. Additionally, collaterals and varices caused by SVT increase the risk of hemorrhage during minimally invasive approaches[3]. Thus, it is important to establish a protocol for screening SVT in patients with necrotizing AP.
DSA is an invasive and time-consuming examination that usually is performed only when the thrombosis causes clinical conditions or is significantly suspected. In contrast, CTV is a non-invasive and quick procedure that can be easily added after performing CECT[10,11]. Additionally, CTV also reveals extravascular abnormalities, mesenteric edema, and the relationship between peripancreatic necrosis and blood vessels[1]. Thus, CTV serves as a more suitable screening tool for patients with necrotizing AP. In addition to the technical matters, CTV results are more likely influenced by extravascular abnormalities. In our study, CTV made 2 diagnoses that were different from the DSA diagnoses.
One limitation of our study is that during the interval between CTV and DSA, the splanchnic system status may have changed. Additionally, the sample size was not large enough and it was a single-center retrospective study.
Although more experience should be gained to determine the role of CTV for detecting SVT in necrotizing AP patients, our study findings suggest that CTV might effectively replace DSA and be the routine imaging method.
Splanchnic vein thrombosis (SVT) may cause severe clinical conditions like hemorrhage, small bowel ischemia and hepatic failure. Its incidence in acute pancreatitis (AP) patients varied widely in different studies. In necrotizing AP patients, the perivascular inflammation and compression by peripancreatic collections or pancreatic necrosis increase the frequency of SVT.
SVT is a well-recognized acute pancreatitis complication and more often occurs in severe patients, especially those with necrosis collections. Few studies have evaluated the effectiveness of computed tomographic venography (CTV) for SVT detection in necrotizing AP patients. In this study, the authors show that CTV could serve as an alternative examination for SVT screening with high accuracy.
Recent studies have suggested that it is important to establish a protocol for screening SVT in patients with necrotizing AP. This is the first article which shows that CTV is an effective examination for SVT detection in patients with necrotizing acute pancreatitis.
By showing that SVT has a high incidence in patients with necrotizing AP and CTV has high accuracy for detecting it, this study suggests that CTV might effectively replace DSA and be the routine imaging method.
This paper is well written and very interesting. It indicates that CTV is an effective examination for SVT detection in patients with necrotizing AP with high positive and negative predictive values. It has great clinical significance.
P- Reviewer: Rabitsch W S- Editor: Qi Y L- Editor: Wang TQ E- Editor: Wang CH
| 1. | Nadkarni NA, Khanna S, Vege SS. Splanchnic venous thrombosis and pancreatitis. Pancreas. 2013;42:924-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 67] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 2. | Gonzelez HJ, Sahay SJ, Samadi B, Davidson BR, Rahman SH. Splanchnic vein thrombosis in severe acute pancreatitis: a 2-year, single-institution experience. HPB (Oxford). 2011;13:860-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 82] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 3. | Besselink MG. Splanchnic vein thrombosis complicating severe acute pancreatitis. HPB (Oxford). 2011;13:831-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Easler J, Muddana V, Furlan A, Dasyam A, Vipperla K, Slivka A, Whitcomb DC, Papachristou GI, Yadav D. Portosplenomesenteric venous thrombosis in patients with acute pancreatitis is associated with pancreatic necrosis and usually has a benign course. Clin Gastroenterol Hepatol. 2014;12:854-862. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 90] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 5. | Willmann JK, Weishaupt D, Böhm T, Pfammatter T, Seifert B, Marincek B, Bauerfeind P. Detection of submucosal gastric fundal varices with multi-detector row CT angiography. Gut. 2003;52:886-892. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 50] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Zhao LQ, He W, Li JY, Chen JH, Wang KY, Tan L. Improving image quality in portal venography with spectral CT imaging. Eur J Radiol. 2012;81:1677-1681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 76] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 7. | Dellinger EP, Forsmark CE, Layer P, Lévy P, Maraví-Poma E, Petrov MS, Shimosegawa T, Siriwardena AK, Uomo G, Whitcomb DC. Determinant-based classification of acute pancreatitis severity: an international multidisciplinary consultation. Ann Surg. 2012;256:875-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 421] [Cited by in RCA: 342] [Article Influence: 26.3] [Reference Citation Analysis (1)] |
| 8. | Harris S, Nadkarni NA, Naina HV, Vege SS. Splanchnic vein thrombosis in acute pancreatitis: a single-center experience. Pancreas. 2013;42:1251-1254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 82] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 9. | Parikh S, Shah R, Kapoor P. Portal vein thrombosis. Am J Med. 2010;123:111-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 134] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 10. | Rubin GD, Dake MD, Napel SA, McDonnell CH, Jeffrey RB. Three-dimensional spiral CT angiography of the abdomen: initial clinical experience. Radiology. 1993;186:147-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 277] [Cited by in RCA: 214] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 11. | Brink JA. Spiral CT angiography of the abdomen and pelvis: interventional applications. Abdom Imaging. 1997;22:365-372. [PubMed] |