Published online Nov 14, 2014. doi: 10.3748/wjg.v20.i42.15815
Revised: May 19, 2014
Accepted: June 20, 2014
Published online: November 14, 2014
Processing time: 323 Days and 16.9 Hours
AIM: To compare the effectiveness of needle-free incision suture closure with butterfly tape and traditional secondary suturing techniques in treating incision infection.
METHODS: Two hundred and twenty-three patients with incision infection following hepatobiliary surgery at a tertiary hospital were randomly divided into three groups: 90 patients were closed by needle-free incision suture closure, which gradually closed the incision wound when drainage from incision infection was visibly decreased and healthy granulation tissues had grown; 79 patients were closed by butterfly bandage; another 54 patients were closed by traditional secondary suturing technique. Healing time of incision infection was calculated from the beginning of dressing change to the healing of the incision.
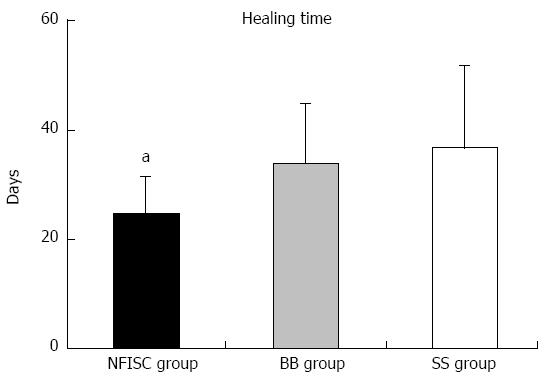
RESULTS: Healing time in the needle-free incision suture closure group (24.2 ± 7.2 d) was significantly shorter than that in the butterfly bandage group (33.3 ± 11.2 d) and the traditional secondary suturing group (36.2 ± 15.3 d) (P < 0.05). Healing time in the butterfly bandage group appeared to be slightly shorter than that in the secondary suture group, but the difference was not statistically significant (P > 0.05).
CONCLUSION: Needle-free incision suture closure could gradually close the infection wound at the same time of drainage and dressing change, thereby shortening the healing time.
Core tip: Both the secondary suturing closure and butterfly bandage methods have been widely used in clinical practice to treat incision infections for many years but have many drawbacks. In comparison to traditional methods the needle-free method of incision infection closure had following advantages: significant decrease in wound closure time; ability to adjust the suture tension at different times and gradually close the wound, thus allowing drainage and dressing at the same time; elimination of complicated and painful secondary suture; elimination of risk of secondary infection; and extreme ease of use.
- Citation: Ma WJ, Zhou Y, Mao H, Xu RH, Shrestha A, Li FY, Lorance A, Yang Q, Zhang YQ, Jiang T, Feng H, Zhang W, Cheng NS. Healing time of incision infection after hepatobiliary surgery treated by needle-free incision suture closure. World J Gastroenterol 2014; 20(42): 15815-15819
- URL: https://www.wjgnet.com/1007-9327/full/v20/i42/15815.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i42.15815
In surgical practice, an incision is the basic step that gains access to the operative field. However, the incision itself is a trauma, disrupting the integrity of local skin tissue, damaging the local protective barrier, promoting microbial invasion and growth, and causing further complications, of which the most common is wound infection[1-8]. As surgical techniques have advanced and hospital infection control has progressed, the rate of incision healing has significantly improved, yet incision infection still occurs for many reasons. The current rate of surgical wound infection is as high as 8.4%, and the treatment of infected incision remains an issue for surgeons[3,4]. In the past, postoperative wound infections were handled by secondary suturing or the butterfly bandage method, often after several weeks of open drainage and dressing. These traditional methods have many drawbacks; use of the butterfly bandage prevents continuous observation of the wound condition, the tape itself cannot be guaranteed to be sterile, and the adhesion strength of tape is often gradually reduced during wound closure. More importantly, the butterfly bandage exerts uneven forces and cannot gradually diminish the tension on an incision wound. For these reasons, this method often results in excessive extrusion of the wound, thereby hindering the growth of granulation tissue. The secondary suture method also has several shortcomings such as post-procedure pain and the need for local anesthesia, and because the appropriate time for closure is very hard to determine, the closure period is often prolonged. Furthermore, the success rate of the secondary suture method is low; sometimes if there is reinfection, the wound has to be reopened, thereby inconveniencing both patients and medical staff. Despite the flaws of these two traditional methods, which have been used clinically for many years for the control of incision infection, still no major changes have been made[8-10].
From January 2010 to June 2013, 90 incision infections after hepatobiliary surgery in our hospital were treated by needle-free incision suture closure (NFISC) (Li Chen Co., Chengdu, China). We found that this method of infected wound closure had the following advantages: unobstructed drainage of wound discharge, early wound closure, shorter wound healing time and higher success rate of incision closure. Our preliminary experience is introduced as follows.
From January 2010 to June 2013, 223 incision infections after hepatobiliary surgery at West China Hospital, Sichuan University School of Medicine, were selected for this study. These cases included 109 male patients and 114 female patients, ranging in age from 21 to 77 years (mean 43 years); 135 cases had wound infection after biliary surgery and 88 cases had wound infection after hepatic surgery. The Hospital Infection Diagnostic Criteria were used[2-4]. The inclusion criterion for this study was postoperative infection on the incision site, and the exclusion criterion was a history of any underlying disease that would affect wound healing. Occurrences of wound fat liquefaction were excluded. Appropriate consent was obtained from each patient. These 223 patients were randomly divided into three groups and treated accordingly: the NFISC group had 90 cases treated by needle-free incision suture closure (Li Chen Co., Chengdu, China), the BB group had 79 cases treated by the butterfly bandage method, and the SS group had 54 cases treated by the secondary suture method. The study protocol was approved by the ethics committee review board of Sichuan University.
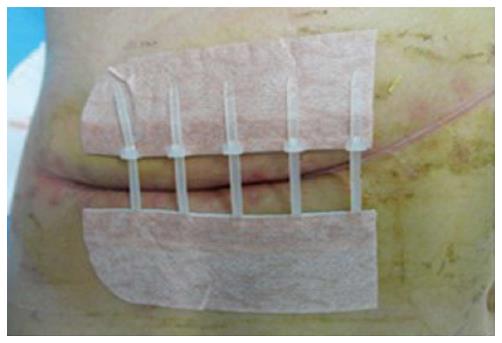
In the NFISC group (n = 90), patients who were diagnosed with surgical wound infection were treated by immediate removal of stitches and other foreign bodies, and drainage of pus. Needle-free suture treatments were used in these patients soon after the drainage decreased significantly and healthy granulation tissue appeared. At the early stage of closure, this method imposed only a small closure force so that the wound remained open; thus the infected fluids drained freely, and dressing of the wound could still be performed. At the later stage of closure, the skin edges of both sides were gradually brought together after much growth of healthy granulation tissue, resulting in complete wound closure (Figures 1 and 2). In the butterfly bandage method group (n = 79) and traditional secondary needle suture group (n = 54), infected wounds were closed by the butterfly bandage or secondary suture methods, respectively, when abnormal secretions disappeared and much healthy granulation tissue had grown after regular change of wound dressings. Wound healing time was calculated from the discovery of incision infection to the healing of the incision.
Data were analyzed using the SPSS v11.0 software package (SPSS, Chicago, IL, United States). Quantitative data are expressed as mean and standard deviation. Statistical comparisons between groups were performed using one-way analysis of variance. The least significant difference test was performed to compare two groups. A P-value < 0.05 was considered statistically significant.
All patients had a Class II right upper quadrant incision under the costal margin. Patients enrolled in this study had no underlying diseases that influenced the healing of the incision wound. Using analysis of variance no statistically significant differences were found at baseline (P > 0.05).
Wound healing time in the NFISC group was 24.2 ± 7.2 d; in the BB group, 33.3 ± 11.2 d; in the SS group, 36.2 ± 15.3 d. The latter included seven cases with failure of wound closure in which the patient had to undergo debridement, drainage dressing and re-suturing, which took longer to heal. The wound healing time in the NFISC group was significantly shorter than that in the BB and SS groups (P < 0.05 for both) (Figure 3). Healing time in the BB group appeared to be slightly shorter than that in the SS group, but the difference was not statistically significant (P > 0.05) (Figure 3).
Incision infection, one of the most common complications of surgery, results in longer hospital stays, increased medical expenses and many other problems for patients and caregivers. The incidence of wound infection directly affects outcomes of surgical procedure, patient satisfaction and the reputation of medical institution[5,11,12]. Wound infection prevention and control have been officially included in hospital management programs and have become an important criterion in evaluation of the quality of medical care[9,10,13]. Research has shown that infection of the incision site is 50% attributable to patient-related factors and 35% to staff-related factors. Risk factors for postoperative wound infection include old age, underlying diseases that influence the wound healing process, other infections, long operative time, poor suturing techniques, blood clots, foreign bodies, faults in the cutting edges and poor health status of patients[6]. Incision infection after abdominal surgery can be healed by traditional techniques, but this often delays healing time, requires a longer hospital stay, and leaves patients with large scars after healing. The secondary suture technique can significantly shorten the course of healing compared with butterfly bandaging but still is not satisfactory because improper techniques and improper suture time sometimes make it impossible to avoid reinfection, which exacerbates the patient’s suffering and economic burden.
The treatment of incision infection depends completely on open drainage. In normal healing, healthy granulation tissue grows slowly from the base of the wound, gradually filling and connecting the wound gap; however, if necrotic debris formed in the infected wound is not drained quickly, it will interfere with the formation of granulation tissue, interrupting new capillary network formation. Accumulation of toxins and enzymes by pyogenic bacteria leads to wound tissue necrosis of collagen fibers, collagen dissolution and increased tissue damage, thereby delaying the wound closure time and leading to the formation of thick scars.
In the past, incision infections were usually treated by secondary suture or butterfly bandage techniques, both of which had many limitations. Secondary suturing requires the patient to undergo local anesthesia prior to closure and often results in post-procedure pain, delayed healing, a coarser scar and sometimes a need to reopen and drain the wound because of reinfection. The butterfly bandage technique imposes uneven force on the wound edges and prevents direct observation of the wound healing; other drawbacks include preventing the drainage of infected fluids, secondary contamination by the tape itself, high wound pressure affecting the growth of granulation tissue, and inconvenience in wound cleaning and dressing. More importantly, when using butterfly bandages, the incision wound tension cannot be adjusted at different times. Thus the closure of the incision often has to rely on granulation tissue, which results in formation of thick scars. These scars may affect various functions and range of motion especially when they occur at joints or other parts. Thus, practical effects of these traditional secondary closure techniques for the infected incision wound are not wholly satisfactory.
Needle-free incision suture closure avoids the need to puncture the skin. By avoiding introduction of a foreign body, this source of a possible reaction is eliminated, and incision inflammation and scarring are consequently reduced[14]. Because the incision is open, necrotic material from the infected incision wound can be drained easily, thereby keeping the wound clean and promoting the healthy growth of granulation tissue, which will have a good effect on infected wound healing and patient satisfaction[15]. Moreover, needle-free incision suture closure method allows us to adjust the suture tension over time and gradually close the infected incision.
According to the results obtained from this study, management of infected incision wound using needle-free incision suture method gradually closes the infection wound and at the same time allows drainage and dressing change, thus shortening the wound healing time. Our preliminary clinical studies have shown that, compared to conventional sewing (secondary suture technique or butterfly bandage), the needle-free incision suture closure method is indeed a preferred method of incision closure, on the basis of significantly reduced healing time. Compared to conventional needle stitching or butterfly bandage to deal with infected wounds, needle-free incision suture closure method imposes equal wound closure force distribution, gradual reduction in the wound tension, and thereby can gradually close the incision with no secondary contamination; most importantly, it is convenient to observe and change dressing during the gradual closure of wound, and such advantages are not possessed by traditional methods[16].
This preliminary study of the clinical efficacy of the needle-free incision suture closure method is limited in scope, presenting only one key measure of clinical efficacy. Prior to wide clinical use, this method requires further study including other measures of efficacy and safety and longer-term follow-up.
In surgical practice, an incision is the basic step that gains access to the operative field. However, the incision itself could cause further complications, of which the most common is wound infection. Despite many drawbacks of traditional methods for the control of incision infection that have been applied clinically for many years, still no major changes have been made to tackle the problem of incision wound infection.
Incision infection is one of the most common complications of surgery. In the past, incision infections were usually treated by secondary suture or butterfly bandage methods, both of which had many limitations. In this study, the authors demonstrate that the needle-free incision suture closure method could be a potential treatment for incision infections.
In comparison to traditional methods the needle-free method of incision infection closure had following advantages: significant decrease in wound closure time; ability to adjust the suture tension over time and gradually close the wound, thus allowing drainage and dressing at the same time; elimination of complicated and painful secondary suture; elimination of risk of secondary infection; and extreme ease of use.
By showing the effectiveness of needle-free incision suture closure method to treat incision infections, this study may represent a future strategy for treatment of patients with incision infections.
Needle-free incision suture closure is a potential method to treat incision infections by imposing a small closure force so that the wound remains open at the early stage of closure; thus the infected fluids were drained freely, at the same time, the dressing of the wound could still be performed. At the later stage of closure, the skin edges of both sides are gradually brought together after much growth of healthy granulation tissue, thus resulting in complete wound closure.
A well done and interesting to read paper about a “problem” that everyone might face during the daily practice.
P- Reviewer: Agresta F, Yoshida H S- Editor: Qi Y L- Editor: Wang TQ E- Editor: Zhang DN
| 1. | Percival NJ. Classification of Wounds and their Management. Surgery (Oxford). 2002;20:114-117. [RCA] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Nichols RL. Postoperative wound infection. N Engl J Med. 1982;307:1701-1702. [PubMed] |
| 3. | Culver DH, Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG, Banerjee SN, Edwards JR, Tolson JS, Henderson TS. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med. 1991;91:152S-157S. [PubMed] |
| 4. | de Lissovoy G, Fraeman K, Hutchins V, Murphy D, Song D, Vaughn BB. Surgical site infection: incidence and impact on hospital utilization and treatment costs. Am J Infect Control. 2009;37:387-397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 761] [Cited by in RCA: 828] [Article Influence: 51.8] [Reference Citation Analysis (0)] |
| 5. | Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999;20:725-730. [PubMed] |
| 6. | Haridas M, Malangoni MA. Predictive factors for surgical site infection in general surgery. Surgery. 2008;144:496-501; discussion 501-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 139] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 7. | Gottrup F. Prevention of surgical-wound infections. N Engl J Med. 2000;342:202-204. [PubMed] |
| 8. | Burke JP. Infection control - a problem for patient safety. N Engl J Med. 2003;348:651-656. [PubMed] |
| 9. | Takahashi Y, Takesue Y, Nakajima K, Ichiki K, Wada Y, Tsuchida T, Ishihara M, Ikeuchi H, Uchino M. Implementation of a hospital-wide project for appropriate antimicrobial prophylaxis. J Infect Chemother. 2010;16:418-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | McHugh SM, Corrigan M, Dimitrov B, Cowman S, Tierney S, Humphreys H, Hill A. A targeted e-learning program for surgical trainees to enhance patient safety in preventing surgical infection. J Contin Educ Health Prof. 2010;30:257-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Kent TS, Sachs TE, Callery MP, Vollmer CM. The burden of infection for elective pancreatic resections. Surgery. 2013;153:86-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 73] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 12. | Ramos N, Skeete F, Haas JP, Hutzler L, Slover J, Phillips M, Bosco J. Surgical site infection prevention initiative - patient attitude and compliance. Bull NYU Hosp Jt Dis. 2011;69:312-315. [PubMed] |
| 13. | Harbarth S, Fankhauser C, Schrenzel J, Christenson J, Gervaz P, Bandiera-Clerc C, Renzi G, Vernaz N, Sax H, Pittet D. Universal screening for methicillin-resistant Staphylococcus aureus at hospital admission and nosocomial infection in surgical patients. JAMA. 2008;299:1149-1157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 397] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 14. | Bang RL, Mustafa MD. Comparative study of skin wound closure with polybutester (Novafil) and polypropylene. J R Coll Surg Edinb. 1989;34:205-207. [PubMed] |
| 15. | Kuo F, Lee D, Rogers GS. Prospective, randomized, blinded study of a new wound closure film versus cutaneous suture for surgical wound closure. Dermatol Surg. 2006;32:676-681. [PubMed] |
| 16. | Spotnitz WD, Falstrom JK, Rodeheaver GT. The role of sutures and fibrin sealant in wound healing. Surg Clin North Am. 1997;77:651-669. [PubMed] |