Published online Oct 28, 2014. doi: 10.3748/wjg.v20.i40.14997
Revised: May 31, 2014
Accepted: June 25, 2014
Published online: October 28, 2014
Processing time: 199 Days and 23.1 Hours
Acute mediastinitis is a fatal disease that usually originates from esophageal perforation and surgical infection. Rare cases of descending necrotizing mediastinitis can occur following oral cavity and pharynx infection or can be a complication of pancreatitis. The most common thoracic complications of pancreatic disease are reactive pleural effusion and pneumonia, while rare complications include thoracic conditions, such as pancreaticopleural fistula with massive pleural effusion or hemothorax and extension of pseudocyst into the mediastinum. There have been no reports of acute mediastinitis originating from pancreatitis in South Korea. In this report, we present the case of a 50-year-old female suffering from acute mediastinitis with pleural effusion arising from recurrent pancreatitis that improved after surgical intervention.
Core tip: Acute mediastinitis is a rare complication of pancreatitis. This case presents acute mediastinitis arising from recurrent pancreatitis that improved after surgical mangement.
- Citation: Choe IS, Kim YS, Lee TH, Kim SM, Song KH, Koo HS, Park JH, Pyo JS, Kim JY, Choi IS. Acute mediastinitis arising from pancreatic mediastinal fistula in recurrent pancreatitis. World J Gastroenterol 2014; 20(40): 14997-15000
- URL: https://www.wjgnet.com/1007-9327/full/v20/i40/14997.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i40.14997
Acute mediastinitis is a fatal disease commonly caused by esophageal perforation and surgical infection. In rare cases, descending necrotizing pancreatitis can originate from oral cavity and pharynx infection[1-3], while mediastinitis secondary to pancreatitis is very rare[4]. Common thoracic complications of pancreatitis are pleural effusion and pneumonia[5,6]. Rare complications can include pancreaticopleural fistula with massive pleural effusion or hemothorax[7,8], mediastinal pseudocyst with pneumonia, pleural effusion[9-11] and cardiac tamponade[12,13]. Acute mediastinitis has not been reported as a thoracic complication of pancreatitis. Here, we report a rare case of acute mediastinitis with long fistula from the pancreatic tail to mediastinum that recovered after fistula resection.
A 50-year-old female visited a local medical center with hemoptysis, cough and chest pain that had lasted for 3 d. Chest computed tomography (CT) was used to diagnose a mediastinal mass with invasion of the right middle lung and pleural thickening. She was transferred to our hospital and admitted to our emergency department. She had a history of daily alcohol intake equivalent to 1-2 bottles of hard liquor and she had suffered from recurrent acute pancreatitis and pseudocysts since 2008.
On physical examination, the patient appeared acutely ill with a clear mental status. She was not febrile and had stable vital signs including blood pressure, 130/80 mmHg; pulse rate, 120 beats per minutes; respiratory rate, 25/min; and body temperature, 36.5 °C. Breath sounds on the right of the chest were decreased, and crackle sounds were present. Laboratory tests showed leukocytosis with a left shift; white blood cell (WBC), 14400/mm3; neutrophils, 78.0%; hemoglobin, 11.6 g/dL; platelet count, 434000 mm3. Blood chemistry showed elevated serum amylase (197.6 IU/L) and lipase (169.0 IU/L) with a normal liver panel and normal electrolyte levels.
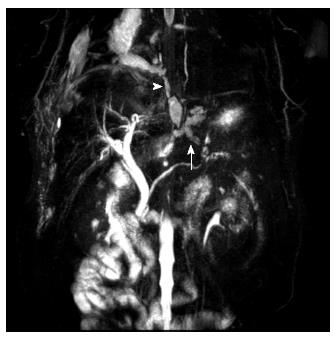
A chest radiograph on admission showed right lung field haziness subsequently eliminated as pneumonia. Chest CT (Figure 1) revealed mediastinitis with fat lysis due to pseudocyst rupture (black arrow), loculated effusion at the right anterior paramediastinal space (white arrow), pleural effusion (black arrowhead), and pneumonic infiltration of the paracardiac area (white arrowhead). A contrast study of the esophagus excluded the possibility of esophageal perforation. Biochemistry from a right thoracentesis revealed a highly elevated amylase level at 83495 IU/mL. These results suggested mediastinitis and loculated effusion of pancreatic etiology. To confirm the relationship between the pancreas and mediastinum, we performed magnetic resonance cholangiopancreatography (MRCP). MRCP showed an 8-mm pseudocyst at the pancreatic tail connected with the distal pancreatic duct (arrow). This pseudocyst communicated with another 2.6 cm pseudocyst in the right paraesophageal area. This second pseudocyst was connected with the mediastinum, as indicated by the arrowhead (Figure 2).
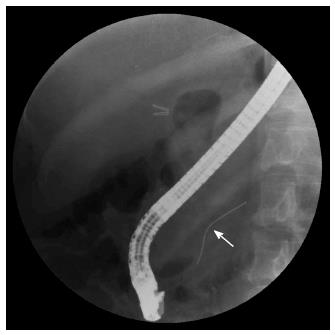
An abdominal CT scan did not reveal severe inflammation around the pancreas. We attempted to insert a pancreatic duct stent by endoscopic retrograde cholangiopancreatography (ERCP). However, due to severe stenosis in the middle pancreatic duct, we could not insert the stent into the pancreatic duct (Figure 3). We located a 5-Fr pig-tail catheter at the proximal pancreatic duct and tried conservative therapy with octreotide. However, the laboratory findings and symptoms of the patient did not improve. Ten days after ERCP, surgery was performed and the operative findings included severe adhesion due to chronic pancreatitis at the distal pancreas and stomach with fistula formation caused by severe adhesion and pseudocyst rupture. Adhesiolysis and fistula resection were performed (Figure 4). A follow-up chest CT scan after surgery showed complete recovery of the mediastinitis. The patient remained under observation in the outpatient department of our hospital.
The general etiology of acute mediastinitis includes esophageal rupture and complications of thoracic operation, although bacterial infection of the oral and pharyngeal cavity may be rare causes that can lead to a fatal clinical course due to conditions such as septic shock[1-3]. Other reports describing mediastinitis secondary to pancreatitis have determined that it was accompanied by bacterial infection and the primary treatment was antibiotics with surgical drainage of the infected mediastinum[3,14]. In contrast, our patient had no abnormal findings on the esophagogram and no retrograde bacterial infection though the fistula tract. The patient suffered from chemical mediastinitis, rather than infectious mediastinitis, and the primary treatment was fistula resection instead of antibiotics.
The pathophysiology of this patient’s condition was similar to internal fistula. The fistulous tract passes either through the aortic or esophageal diaphragmatic orifices or directly through the diaphragm. If pancreatic duct disruption occurs anteriorly and is not walled off, a pancreatic-peritoneal fistula will develop, manifesting with ascites. If the disruption develops posteriorly, the pancreatic juice will flow into the retroperitoneal space and may dissect through the aortic or esophageal hiatus into the mediastinum to form a pleural fistula or present as a mediastinal pseudocyst, which ruptures into the pleural cavity and forms a pleural fistula[15].
In this case, chronic recurrent pancreatitis produced multiple pseudocysts that communicated with long fistula in a manner similar to a tunnel. We postulated that acute mediastinitis occurred because of continuous pancreatic juice leakage through the fistula. Most of the pancreaticopleural fistula patients are admitted to the hospital with respiratory symptoms since common complaints include dyspnea, chest pain, cough, sputum and fever[7]. Analysis of internal pancreatic fistula reports from 1990 to 2004 revealed that 84% of patients had a history of chronic alcoholic use, 74% had a past history of pancreatitis and 81% were male. The most common symptom was dyspnea, in 70% of patients. Other common complaints were chest pain and cough in 30% and 22% of patients, respectively[16]. Thus, before diagnosing a pancreatic form of the disease, patients might undergo respiratory testing, which could delay the diagnosis and contribute to the high mortality and morbidity.
Our case was a female who suffered from coughing with hemoptysis during the initial stage and she had nearly stopped drinking due to chronic pancreatitis. A chest imaging study showed a mass-like lesion at the mediastinum with pneumonia. Thus, the patient was admitted to the respiratory division and later transferred to the gastroenterology division. Thoracentesis and body fluid analysis are important in evaluating the etiology of this condition[3,5,7,8]. Pancreatic pleural effusion originating from pancreatitis can usually be identified by high levels of amylase, lipase, and albumin[15]. The patient in our cases did not have sufficient pleural effusion to suggest pancreatitis, although chest CT showed a specific loculated form of pleural effusion. Analysis of body fluids showed a high level of amylase indicative of mediastinitis with pleural effusion secondary to pancreatitis.
MRCP performed an important role in making a treatment decision in this case[17] because we recognized that the main pancreatic duct communicated with each pseudocyst to the mediastinum, which allowed identification of mediastinitis origin. We postulated that the pathophysiology of this mediastinitis was similar to pleural and peritoneal fistula.
The primary treatment for pancreaticopleural fistula is non-surgical drainage of pleural effusion, fasting, medications such as octreotide, and pancreatic duct stent insertion under ERCP. There are some reports that these types of therapies can result in a complete cure, although recurrence can occur in the presence of distal pancreatic duct stenosis or a failure of stent insertion. Two reports have determined that 62% and 69% of pancreaticopleural fistula patients require surgical treatment[16], and two cases of pancreaticopleural fistula in South Korea resulted in a full recovery after surgical intervention[7,8]. Surgical treatment can differ depending on location and visualization of the fistula. Generally, a pancreatic tail resection is performed when the fistula is located at the pancreatic tail. Pancraticojejunostomy can be performed when the fistula is at the pancreatic head or when there is proximal duct stenosis at the pancreatic head. The success rate of surgery was reported to be 80%-95%[16]. In this case, we initially attempted medical intervention; however, due to severe stenosis of the mid-portion of the pancreatic duct, we did not insert a guiding wire. After inserting the stent in the proximal pancreatic duct, we proceeded with medical therapy. However, serum amylase levels remained elevated and the patient’s symptoms did not improve, which led to surgical treatment. Following pancreatic tail and pancreatic-mediastinal fistula resection, follow-up chest and abdominal CT showed near-total recovery.
In conclusion, acute mediastinitis is a rare complication of pancreatitis. The primary indicators are respiratory symptoms such as hemoptysis and cough, which delay the diagnosis. In the absence of bacterial infection, physicians should consider stent insertion and conservative therapy as the primary treatment, although rapid progression of acute mediastinitis may require prompt surgical intervention when the response to medical treatment is not sufficient.
A 50-year-old female with respiratory symptoms such as hemoptysis and cough.
She presented decreased breath sound and crackles on auscultation of the right lung.
Mediastinal mass, mediastinitis.
White blood cell 14400/mm3; neutrophils, 78.0%; hemoglobin, 11.6 g/dL; platelet counts, 434000 mm3; elevated serum amylase (197.6 IU/L) and lipase (169.0 IU/L); liver panel and electrolyte levels were within normal limits.
Magnetic resonance cholangiopancreatography revealed mediastinitis with fat lysis due to pancreatic mediastinal fistula that communicated with the distal pancreatic duct.
The cytologic examination of pleural effusion did not show malignant cells.
After failure of stent insertion under endoscopic retrograde cholangiopancreatography, adhesiolysis and fistula resection were performed.
Acute mediastinitis is rare complication of pancreatitis. Respiratory symptoms can delay diagnosis. Acute mediastinitis may require prompt surgical intervention when the response to medical treatment is not sufficient.
This paper presents a rare case of acute mediastinitis that is a complication of pancreatitis with long pancreatic mediastinal fistula that needs surgical intervention.
P- Reviewer: Chiang TA, Kayadibi H, Martignoni ME S- Editor: Ding Y L- Editor: Wang TQ E- Editor: Ma S
| 1. | Alsoub H, Chacko KC. Descending necrotising mediastinitis. Postgrad Med J. 1995;71:98-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 25] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Kim JH, Ryu DM, Jee YJ, Lee JW, Lee DW. Mediastinitis: a case report. J Korean Assoc Oral MaxillofacSurg. 2010;36:538. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Chang YC, Chen CW. Thoracoscopic drainage of ascending mediastinitis arising from pancreatic pseudocyst. Interact Cardiovasc Thorac Surg. 2009;9:144-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Iacono C, Procacci C, Frigo F, Andreis IA, Cesaro G, Caia S, Bassi C, Pederzoli P, Serio G, Dagradi A. Thoracic complications of pancreatitis. Pancreas. 1989;4:228-236. [PubMed] |
| 5. | Kim YT. [Medical management of acute pancreatitis and complications]. Korean J Gastroenterol. 2005;46:339-344. [PubMed] |
| 6. | Kim HY, Seo DW, Lee TY, Kang HH, Lee SK, Kim MH, Min YI. A Clinical review on chronic pancreatitis. Korean J Gastroenterol. 2002;40:191-196. |
| 7. | Park SY, Jang JY, Lee SE, Yang SH, Kim SW. Pancreaticopleural fistula: complication of chronic pancreatitis. Korean J Hepato-Biliary-Pancreat Surg. 2006;10:29-33. |
| 8. | Sul YH, Shin HS, Lee KH, Chun KS, Song IS. Pancreaticopleural fistula with hemothorax. J Korean Surg Soc. 2009;76:187. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Nam KW, Chae HS, Kim HR, Kwok SK, Lee BI, Cho YS, KimSS , Han SW, Lee CD, Choi KY. A case of mediastinal pancreatic pseudocyst presenting with pneumonia. Korean J Gastroenterol. 2002;40:414-418. |
| 10. | Maeng HY, Jung JH, Lee SW, Park MS, Chung JH, Kim DH, Park SW, Choi BW, Kim SK, Chang J. A Case of mediastinal pancreatic pseudocyst. Tuberc Respir Dis. 2002;52:271-277. |
| 11. | Park SH, Kim SJ, Kim EJ, Lee MH, Kim HS, Chung IK, Kim C, Lee CE. A Case of mediastinal pancreatic pseudocyst treated with octreotide. Korean J Gastroenterol. 1999;34:417-421. |
| 12. | Jung HC, Nah DY, Park KU, Lee CH, Jung SY, Chun WJ, Yoon BG, Kang SW, Lee CD, Lee SK. A Case of cardiac tamponade caused by acute pancreatitis. J Korean Soc Echocardiogr. 2001;9:66-69. |
| 13. | Lee JS, Kim YS, Chang WC, Lee JW, Moon JS, Yum HK, Choi SK. Cardiac tamponade complicated by chronic recurrent pancreatitis. Korean J Med. 2003;65:S693-S697. |
| 14. | Ayuso-Velasco R, García-Barajas S, García-Sáez M. Mediastinitis secondary to acute pancreatitis. Arch Bronconeumol. 2011;47:319-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Dhebri AR, Ferran N. Nonsurgical management of pancreaticopleural fistula. JOP. 2005;6:152-161. [PubMed] |
| 16. | Oh YS, Edmundowicz SA, Jonnalagadda SS, Azar RR. Pancreaticopleural fistula: report of two cases and review of the literature. Dig Dis Sci. 2006;51:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Materne R, Vranckx P, Pauls C, Coche EE, Deprez P, Van Beers BE. Pancreaticopleural fistula: diagnosis with magnetic resonance pancreatography. Chest. 2000;117:912-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |