Published online Jul 28, 2014. doi: 10.3748/wjg.v20.i28.9618
Revised: January 7, 2014
Accepted: March 5, 2014
Published online: July 28, 2014
Processing time: 225 Days and 6.6 Hours
Splenic rupture (SR) after colonoscopy is a very rare but potentially serious complication. Delayed diagnosis is common, and may increase morbidity and mortality associated. There is no clear relation between SR and difficult diagnostic or therapeutic procedures, but it has been suggested that loop formation and excessive torquing might be risk factors. This is a case of a 65-year-old woman who underwent endoscopic submucosal dissection (ESD) for lateral spreading tumor in the descending colon, and 36 h afterwards presented symptoms and signs of severe hypotension due to SR. Standard splenectomy was completed and the patient recovered uneventfully. Colorectal ESD is usually a long and position-demanding technique, implying torquing and loop formation. To our knowledge this is the first case of SR after colorectal ESD reported in the literature. Endoscopists performing colorectal ESD in the left colon must be aware of this potential complication.
Core tip: Splenic rupture after colonoscopy is a very rare but potentially serious complication. This is a case of a 65-year-old woman who suffered severe splenic rupture after colorectal endoscopic submucosal dissection (ESD) for lateral spreading tumor in the descending colon. Colorectal ESD is usually a long and position-demanding technique, implying torquing and loop formation. To our knowledge this is the first case of splenic rupture after colorectal ESD reported in the literature.
- Citation: Tejada AH, Giménez-Alvira L, Brule EVD, Sánchez-Yuste R, Matallanos P, Blázquez E, Calleja JL, Abreu LE. Severe splenic rupture after colorectal endoscopic submucosal dissection. World J Gastroenterol 2014; 20(28): 9618-9620
- URL: https://www.wjgnet.com/1007-9327/full/v20/i28/9618.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i28.9618
Splenic rupture (SR) after colonoscopy is a very rare complication, with an estimated incidence rate of 1-21 cases/100000 colonoscopies/year[1,2], with a higher proportion in female population[2-5]. It was first reported in the mid-70 s[5,6], and since then slightly over 100 cases have been reported worldwide[2], probably due to underreporting or due to a bias toward the publication of severe cases[2,3,7].
Delay in diagnosis is common and may be related to increased morbidity and mortality (up to 5%)[2,3], as well as to a source of professional liability[8]. Sudden upper left quadrant abdominal pain and left shoulder pain (Kehr´s sign), significant hemoglobin drop or symptoms associated with low blood pressure should alert us[2-4,7,8]. Diagnosis of this complication may be right during colonoscopy withdrawn (free blood sign in the left colon)[7], but usually happens several days after[2-4,9]. Emergent abdominal computerized tomography (CT) provides diagnostic confirmation[2,3].
Most of the cases published in the literature were not related to difficult diagnostic or therapeutic colonoscopies[2-4]. It has been suggested that loop formation and excessive torquing might induce significant stress over the splenocolic attachments and trigger splenic surface avulsion[2,3,7]. Some authors consider that tension over iatrogenic adhesions between left colon and spleen in patients with previous abdominal surgery may be related[3,6,8], but conclusive data have not been reported so far. Though mild cases with favorable prognosis can be treated conservatively (observation or splenic embolization)[2,3], those with significant bleeding (hemoglobin drop > 3 g/dL) require emergent surgery and splenectomy[2-4,10].
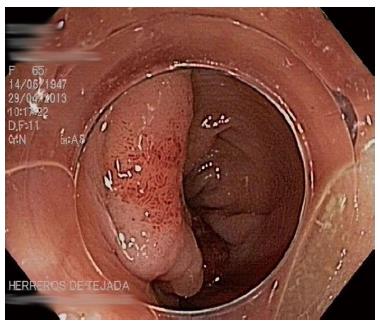
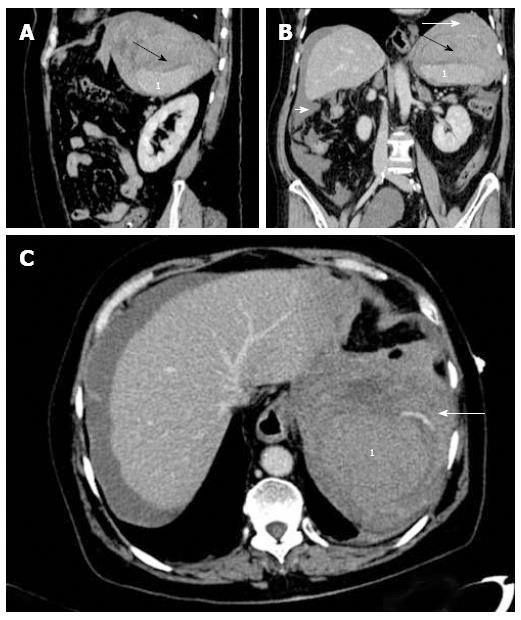
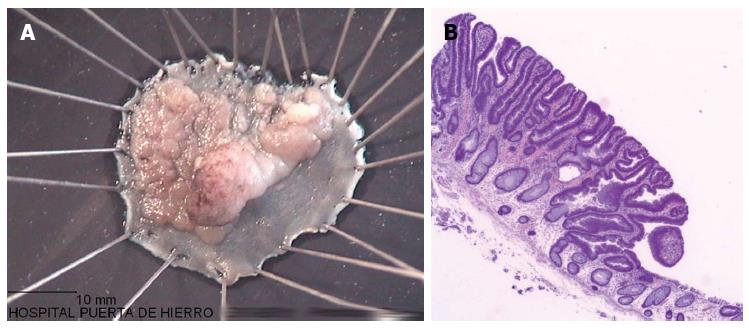
A 65-year-old woman with no significant medical history and no prior surgery was admitted for endoscopic submucosal dissection (ESD) of a lateral spreading tumor granular mixed type (0-Is + IIa), 30 mm in larger diameter, located in the proximal descending colon (Figure 1). Procedure was performed under deep sedation controlled by anesthesiologist in the endoscopy unit. A pediatric colonoscope (PCF-H180 AI/L, Olympus Co.) with a regular 11.8 mm plastic cap attached (D-201-11304, Olympus Co.) was used to perform ESD; special knifes utilized were Flush knife 1.5 BT (Fujifilm, Co) and Hook knife (Olympus, Co.). En-bloc resection was completed successfully in 74 min without apparent complications. The patient started experiencing dizziness and significant hypotension 36 h after the procedure, with a drop in hemoglobin level of 7 g/dL. Resuscitation maneuvers were initiated and emergent CT showed signs of SR, with active vascular contrast extravasation, perisplenic hematoma and large hemoperitoneum (Figure 2). The patient was taken to the operating room and emergent laparotomy demonstrated 2.5 L hemoperitoneum and multiple splenic lacerations, with no signs of colonic lesions. Standard splenectomy was completed, with no further events. According to guidelines, standard post-splenectomy vaccination on the patient was started right after surgery. The patient was discharged 6 d after. Final pathology of the ESD specimen showed a 32 mm × 22 mm tubular adenoma with low-grade dysplasia and free lateral and deep margins (R0) (Figure 3), whereas the assessment of the spleen did not show any significant abnormality.
To the best of our knowledge, SR after colorectal ESD has not previously been described, probably due to the fact that the number of procedures worldwide is exceedingly small compared to the number of diagnostic or regular therapeutic colonoscopies. Nevertheless, it is expected that increasing number of colorectal ESD will be performed every year with the progressive adoption of this technique. In addition, this technique commonly implies long procedures, with frequent changes of patient´s position and scope movements (torquing and bending) to get the best of gravity for adequate working field, a risk factor suggested in several studies[2,3,7].
In the present report the timeline between the procedure and the onset of symptoms supports the causal relationship between colorectal ESD and splenic injury. The location of the colonic neoplasia next to the splenic flexure and the extended time (> 1 h) with repeated torquing and bending might have contributed to this uncommon complication. Endoscopists performing ESD worldwide must be aware of this rare but potentially deadly complication, particularly if the target lesion is located next to the splenic flexure. We recommend that in those cases informed consent for ESD should particularly address this potential risk for legal purposes.
A 65-year-old woman presenting with dizziness 36 h after colorectal endoscopic submucosal dissection (ESD) for lateral spreading tumor (LST) had been performed.
Hypotension and severe hemoglobin drop.
Acute digestive bleeding, colonic perforation, splenic rupture, acute gastrointestinal ischemia.
Hemoglobin drop from baseline (Hb 7 g/dL).
Emergent computerized tomography showed splenic rupture with active vascular contrast extravasation and perisplenic hematoma and large hemoperitoneum.
Splenic rupture with no other pathological features.
Resuscitation maneuvers were completed and emergent standard splenectomy was performed.
LST (lateral spreading tumor) refers to large (> 10 mm) flat colorectal lesions, usually equivalent to advanced adenomas or minimally invasive adenocarcinoma.
Colorectal ESD is increasingly extending in the world, and endoscopists must be aware of the possibility of splenic rupture as a delayed and life-threatening complication.
This is the first case of splenic rupture after colorectal ESD ever reported, and despite its uncommonness, it should be included in the list of possible complications.
P- Reviewer: Luigiano C, Lo GH, Meister T S- Editor: Ma YJ L- Editor: A E- Editor: Liu XM
| 1. | Kamath AS, Iqbal CW, Sarr MG, Cullinane DC, Zietlow SP, Farley DR, Sawyer MD. Colonoscopic splenic injuries: incidence and management. J Gastrointest Surg. 2009;13:2136-2140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 2. | Singla S, Keller D, Thirunavukarasu P, Tamandl D, Gupta S, Gaughan J, Dempsey D. Splenic injury during colonoscopy--a complication that warrants urgent attention. J Gastrointest Surg. 2012;16:1225-1234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 48] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Ha JF, Minchin D. Splenic injury in colonoscopy: a review. Int J Surg. 2009;7:424-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 47] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Michetti CP, Smeltzer E, Fakhry SM. Splenic injury due to colonoscopy: analysis of the world literature, a new case report, and recommendations for management. Am Surg. 2010;76:1198-1204. [PubMed] |
| 5. | Smith LE. Fiberoptic colonoscopy: complications of colonoscopy and polypectomy. Dis Colon Rectum. 1976;19:407-412. [PubMed] |
| 6. | Wherry DC, Zehner H. Colonoscopy-fiberoptic endoscopic approach to the colon and polypectomy. Med Ann Dist Columbia. 1974;43:189-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 114] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Rex DK. Colonoscopic splenic injury warrants more attention. Gastrointest Endosc. 2013;77:941-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Zandonà C, Turrina S, Pasin N, De Leo D. Medico-legal considerations in a case of splenic injury that occurred during colonoscopy. J Forensic Leg Med. 2012;19:229-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Ellis WR, Harrison JM, Williams RS. Rupture of spleen at colonoscopy. Br Med J. 1979;1:307-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Rasul T, Leung E, McArdle K, Pathak R, Dalmia S. Splenic rupture following routine colonoscopy. Dig Endosc. 2010;22:351-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |