Published online Jul 21, 2014. doi: 10.3748/wjg.v20.i27.9154
Revised: January 13, 2014
Accepted: April 2, 2014
Published online: July 21, 2014
Processing time: 251 Days and 15.6 Hours
AIM: To systematically characterize specific pain patterns in the most frequent pancreatic diseases.
METHODS: Pain in patients with chronic pancreatitis (n = 314), pancreatic cancer (n = 469), and other pancreatic tumors (n = 249) including mucinous (n = 20) and serous cystadenoma (n = 31), invasive (n = 37) and non-invasive intraductal papillary mucinous neoplasia (IPMN; n = 48), low stage (n = 18) and high stage neuroendocrine neoplasia (n = 44), and ampullary cancer (n = 51) was registered and correlated with clinicopathological data. Survival times were estimated by the Kaplan-Meier method. Patients alive at the follow-up time were censored. Survival curves were compared statistically using the log-rank test.
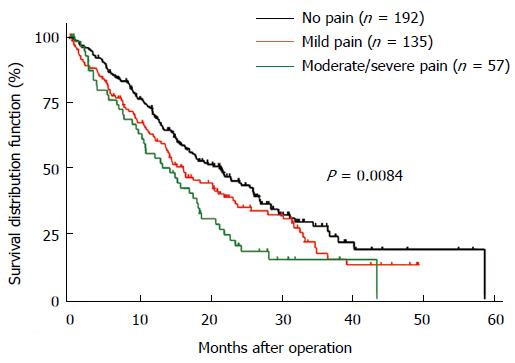
RESULTS: Forty-nine point one percent of pancreatic cancer patients revealed no pain, whereas in chronic pancreatitis only 18.3% were pain free. In contrary, moderate/severe pain was registered in 15.1% in pancreatic cancer patients that was increased in chronic pancreatitis with up to 34.2%. Serous cystadenoma was asymptomatic in most cases (58.1%), whereas 78.9% of all mucinous cystadenoma patients suffered pain. In neuroendocrine neoplasia pain was not a key clinical symptom since 64% of low stage neuroendocrine neoplasia and 59% of high stage neuroendocrine neoplasia patients were pain free. Cancer localization in the pancreatic body and patients with malignant pancreatic neoplasms were associated with more severe pain. Tumor grading and stage did not show any impact on pain. Only in pancreatic cancer, pain was directly associated with impaired survival.
CONCLUSION: Pancreatic pain depicts different patterns of abdominal pain sensation according to the respective pancreatic disorder and does not allow a unification of the term pancreatic pain.
Core tip: Abdominal pain is a major clinical feature in chronic pancreatitis and pancreatic cancer. Little is known about pain sensations in other, less frequent pancreatic tumors. This study is to our knowledge the first to systematically record pain patterns in all pancreatic tumors. Additionally, these were correlated with clinicopathological data. Pain patterns in pancreatic diseases turned out to be very diverse and mainly dependent on tumor type, anatomic localization and dignity. In pancreatic cancer pain was significantly associated with impaired survival.
- Citation: D’Haese JG, Hartel M, Demir IE, Hinz U, Bergmann F, Büchler MW, Friess H, Ceyhan GO. Pain sensation in pancreatic diseases is not uniform: The different facets of pancreatic pain. World J Gastroenterol 2014; 20(27): 9154-9161
- URL: https://www.wjgnet.com/1007-9327/full/v20/i27/9154.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i27.9154
Chronic enduring visceral pain frequently develops in pancreatic diseases, especially in chronic pancreatitis and advanced pancreatic cancer. However, little is known about the impact of pain in less frequent pancreatic diseases like cystadenomas, intraductal papillary mucinous neoplasia (IPMN), neuroendocrine neoplasia and ampullary cancer.
Abdominal pain is the most (80%-94%) common and the most difficult to manage clinical feature among chronic pancreatitis patients[1,2]. It is often characterized as burning, intermittent, and shooting pain but can as well occur as constant or continuous pain with superimposed acute flares. The pathophysiology of chronic pancreatitis pain is poorly understood. A large recent prospective study including 540 chronic pancreatitis patients demonstrated that disease duration did not correlate with pain severity or frequency in their cohort[1]. Hence, this observation contradicts the opposite hypothesis: i.e., “burn-out-hypothesis” of chronic pancreatitis progression during which pain improves with progressive pancreatic insufficiency[3].
Pancreatic cancer is a devastating disease with poor long-term survival, which is often accompanied by abdominal or back pain limiting the quality of life. Pancreatic pain in pancreatic cancer is associated with a poor prognosis and is typically described as deep-delving pain penetrating to the back[4]. Early stage pancreatic cancer is associated with abdominal pain in only 30% of patients, while 60% of patients with limited and 80% of patients with advanced pancreatic cancer complain of abdominal and/or back pain[5]. At the time of diagnosis, the disease is often advanced and up to 73% of patients suffer from abdominal pain[6]. The localization of the tumor seems to play a major role, since patients with tumors in the head of the pancreas had less pain than patients with cancer in the body or tail of the pancreas, independent of tumor stage or size[6].
Mechanisms of pain generation in pancreatic cancer and chronic pancreatitis have not been completely understood. At first glance, pain was reported to occur by completely different mechanisms in pancreatic cancer and chronic pancreatitis. In chronic pancreatitis, pain generation was attributed to ductal strictures, increased intraductal pressure, interstitial hypertension, and pancreatic pseudocysts[7,8]. The initial hypothesis on the generation of abdominal pain in pancreatic cancer was based on the mechanical pressure and/or invasion of neighboring organs, and especially by cancer cell invasion of the neural plexus. Nowadays a variety of ligands and their respective receptors have been identified to play roles in the initiation of pancreatic pain[9]. It is now widely accepted that pain sensation in both pancreatic cancer and chronic pancreatitis has been identified as neuropathic due to the prominent neuroplastic alterations which cannot be seen to that extent in any other gastrointestinal disorders[10,11]. This specific pancreatic neuropathy is characterized by enlarged intrapancreatic nerves which are increased in number and frequently infiltrated by inflammatory and/or cancer cells, leading to pancreatic neuritis and perineural cancer cell invasion[12-15]. Furthermore, pancreatic neuropathy is characterized by numerous molecular and morphological alterations at both the peripheral and the central nervous system level[10]. Increased peripheral nociceptive signals mediated by neurotransmitters and neurotrophic factors together with neural damage and neuroplastic alterations are paralleled by hypersensitive dorsal root ganglia and spinal cord neurons[10]. At lasts, the cerebral cortex adapts to these changes by increasing its basal activity[16]. These phenomena are closely associated with increased abdominal pain sensation in the respective patients[4]. Such neuropathic changes or neuropathic pain sensation were not registered in other pancreatic tumors like, cystadenomas, IPMN, neuroendocrine neoplasia and ampullary cancer.
Little is known about pain sensation and their mechanisms in pancreatic neoplasms other than pancreatic cancer and chronic pancreatitis and their pain patterns have not yet been fully characterized. Therefore, the current study aimed at systematically analyzing pain sensation in patients with different pancreatic neoplasms. Both chronic pancreatitis and all pancreatic tumors including pancreatic cancer, mucinous and serous cystadenoma, IPMN, neuroendocrine neoplasia, and ampullary cancer were evaluated regarding their pain intensity and frequency and associated with tumor localization, dignity, stage and grading.
Pancreatic tissue samples were collected from patients following pancreatic resection due to the following pathologies: Pancreatic adenocarcinoma (n = 469), chronic pancreatitis (n = 314) and other pancreatic tumors/PTm (n = 249) including mucinous (n = 20) and serous cystadenoma (n = 31), invasive intraductal papillary mucinous neoplasia (IPMN; n = 37) and non-invasive IPMN (n = 48), low stage (UICC Stage 1-2) neuroendocrine neoplasia (n = 18) and high stage (UICC Stage 2-4) neuroendocrine neoplasia (n = 44), and ampullary cancer (n = 51). The stage of pancreatic cancer, invasive IPMN, neuroendocrine neoplasia and ampullary cancer was graded according to the international classification of the UICC. The study protocol was approved by the ethics committee of the University of Heidelberg (Germany), Tissue preservation was performed as reported previously[13].
Consecutive sections obtained from paraformaldehyde-fixed and paraffin-embedded pancreatic tissue from each patient were stained with hematoxylin and eosin for concomitant histomorphological examination. Histopathological verification of the diagnosis and cancer classification was performed by an expert in pancreatic pathology.
In all patients, the individual pain score was prospectively recorded prior to the operation in hospital one day before surgery, including pain intensity and frequency. The intensity of pain was graded by using the following scale: 0 = none, 1 = mild, 2 = moderate (abdominal discomfort or pain which is non-disabling but requires analgesics) and 3 = severe pain (pain which is disabling and controlled only by narcotic analgesics) In addition, the frequency of pain was graded as 3 = daily, 2 = weekly, and 1 = monthly. To calculate the severity of pain, pain intensity and pain frequency of each individual were multiplied. According to the final pain score, the patients were categorized into 3 groups: Pain 0 (0) representing the group of patients who did not have any pain; Pain I (1-3) representing the group of patients with mild pain; and Pain II (4-9), the group that suffered from moderate to severe pain, as demonstrated previously[13,17,18].
Overall survival was defined as the time from the date of tumor resection to either death from any cause or last follow-up. At the time of analysis, 384 patients with pancreatic cancer (81.9%) were dead, and 85 (18.1%) were alive.
Statistical analysis was performed by an expert statistician (UH) using the SAS (Release 9.1; SAS Institute, Inc, Cary, NC, United States) and GraphPad Prism 4 Software. Survival times were estimated by the Kaplan-Meier method. Patients alive at the follow-up time were censored. Survival curves were compared statistically using the log-rank test. The χ2 test, if appropriate or the Fisher’s exact test was used to compare subgroups with respect to pain severity. Two-sided P values were always computed, and a P value was considered statistically significant at the 5% level.
Almost 50% of patients with pancreatic cancer did not have any pain (Pain 0), while only 15.1% of patients suffered from moderate to severe pain (Pain II; Table 1). Distinct differences in pancreatic pain are evident when especially comparing the pain pattern of patients with chronic pancreatitis to those with pancreatic cancer. Nearly half of all pancreatic cancer patients (49.1%) revealed no pain at all, whereas this figure was noticeably less in chronic pancreatitis patients with only 18.3% of the total chronic pancreatitis population (Table 1). In other words, while almost 50% of pancreatic cancer patients were pain free, more than 80% of chronic pancreatitis patients had at least mild pain sensations. In detail, patients with pancreatic cancer showed generally less pain, with 154 cases of mild pain (Pain I: 35.8%) and 65 cases of moderate to severe pain (Pain II: 15.1%) in direct comparison to significantly greater mild pain (Pain I : 47.5%) and moderate to severe pain sensation (Pain II: 34.2%, P < 0.0001, Table 1) in chronic pancreatitis.
| Diagnosis | Pain | P value | ||
| Pain 0 | Pain I | Pain II | ||
| Pancreatic cancer | 211 | 154 | 65 | < 0.0001 |
| (49.0) | (35.8) | (15.1) | ||
| Chronic pancreatitis | 54 | 140 | 101 | |
| (18.3) | (47.5) | (34.2) | ||
| Serous cystadenoma | 18 | 12 | 1 | < 0.02 |
| (58.0) | (38.7) | (3.2) | ||
| Mucinous cystadenoma | 4 | 11 | 4 | |
| (21.0) | (57.9) | (21.0) | ||
| Non-invasive IPMN | 19 | 20 | 2 | 0.235 |
| (46.3) | (48.8) | (4.9) | ||
| Invasive IPMN | 11 | 18 | 5 | |
| (32.4) | (52.9) | (14.7) | ||
| Low stage neuroendocrine neoplasia | 9 | 5 | 0 | 0.565 |
| (64.3) | (35.7) | (0.0) | ||
| High stage neuroendocrine neoplasia | 23 | 13 | 3 | |
| (59.0) | (33.3) | (7.7) | ||
| AmpC | 27 | 13 | 4 | |
| (61.4) | (29.6) | (9.1) | ||
| Total | 322 | 246 | 84 | |
| (49.4) | (37.7) | (12.9) | ||
Particularly striking were the differences in pain sensation comparing the two different cystadenomas of the pancreas. Whereas, patients with serous cystadenoma seem to be almost free of pain in the majority of cases (Pain 0: 58.1%), nearly 80% of all patients with mucinous cystadenoma suffered at least from mild to severe pain (P < 0.02, Table 1). There was no significant difference in the presence of pain between the non-invasive vs. invasive IPMN but with a trend towards higher pain sensations in patients with invasive IPMN (14.7% vs 4.9%, Table 1). Interestingly, abdominal pain in patients with neuroendocrine neoplasia seems not to be a key clinical symptom since 64% of patients with low stage neuroendocrine neoplasia and 59% of patients with high stage neuroendocrine neoplasia did not report of any pain at all (Table 1). Although not significant, it was again noticeable that patients with the more invasive disorder/ high stage neuroendocrine neoplasia showed greater moderate to severe pain sensations than low stage neuroendocrine neoplasia (7.7% vs 0.0%, Table 1). Similar to neuroendocrine neoplasia of the pancreas most patients with ampullary cancer did not report any symptoms of pain (61.4%, Table 1).
The pancreatic head was by far the most common tumor localization (63%) among all pancreatic tumors and represented the most frequent tumor site for pancreatic cancer and IPMN (Table 2). On the other hand, serous and mucinous cystadenomas were the only pancreatic tumors that were most commonly observed in the pancreatic body and tail (Table 2). To clarify whether anatomical tumor localization is affecting the patient’s pain status, pancreatic tumor localization was related to individual pain sensation. Here, patients with ampullary cancer were excluded due to their solely localization at the ampullary region and patients with chronic pancreatitis since these special subtype of patients display an inflammatory disease which is frequently affecting several parts of the pancreas. Pancreatic tumor localization tends to influence pain sensation independent of tumor histology. The percentage of patients with no pain (Pain 0) was considerably lower in patients with tumors in the pancreatic body (39.0%) or tail (42.0%) compared to those in the pancreatic head (51.0%). In the entire pancreatic tumor population the most severe pain was detected in patients with a tumor located in the pancreatic body (16.9% vs 13.5% in the pancreatic head and 14.8% in the pancreatic tail), but this difference showed no statistical significance. Thirty-five point nine percent of patients with a tumor in the pancreatic head showed mild pain (Pain I) sensations (vs 44.2% of patients with a tumor in the pancreatic body and 43.2% of patients with a tumor in the pancreatic tail). But regarding the largest subgroup of patients with pancreatic cancer, it was evident (P < 0.02) that 29.8% of these pancreatic cancer patients with a tumor at the pancreatic body were pain free (Pain 0), 46.8% revealed mild (Pain I) and 23.4% moderate/severe (Pain II) pain. In contrast, the majority of patients with pancreatic cancer in the pancreatic head had no pain (53.0% vs 33.0% Pain I and 14% Pain II). Accordingly, the rate of patients with moderate to severe pain (Pain II) was considerably higher for pancreatic cancer patients with a pancreatic body tumor when compared to pancreatic cancer patients with a pancreatic head or tail cancer (23.4% vs 14.0% and 17.5% respectively).
| Diagnosis | Tumor localization | |||||
| Pancreatic head | Pancreatic body | Pancreatic tail | > 1 pancreatic area | Pancreas unspecified | Papilla vateri | |
| Pancreatic cancer | 362 | 50 | 44 | 11 | 1 | 1 |
| (77.2) | (10.7) | (9.4) | (2.4) | (0.2) | (0.2) | |
| Serous cystadenoma | 8 | 9 | 9 | 4 | 1 | 0 |
| (25.8) | (29.0) | (29.0) | (12.9) | (3.2) | (0.0) | |
| Mucinous cystadenoma | 2 | 6 | 9 | 1 | 1 | 1 |
| (10.0) | (30.0) | (45.0) | (5.0) | (5.0) | (5.0) | |
| Non-invasive IPMN | 33 | 2 | 3 | 6 | 2 | 2 |
| (68.8) | (4.2) | (6.3) | (12.5) | (4.2) | (4.2) | |
| Invasive IPMN | 26 | 3 | 4 | 4 | 0 | 0 |
| (70.3) | (8.1) | (10.8) | (10.8) | (0.0) | (0.0) | |
| Low stage neuroendocrine neoplasia | 5 | 4 | 4 | 2 | 2 | 1 |
| (27.8) | (22.2) | (22.2) | (11.1) | (11.1) | (5.6) | |
| High stage neuroendocrine neoplasia | 16 | 7 | 14 | 1 | 2 | 4 |
| (36.4) | (15.9) | (31.8) | (2.3) | (4.5) | (9.1) | |
| Ampullary cancer | 0 | 0 | 0 | 0 | 0 | 51 |
| (0.0) | (0.0) | (0.0) | (0.0) | (0.0) | (100) | |
| Total | 452 | 81 | 87 | 29 | 9 | 60 |
| (63.0) | (11.3) | (12.1) | (4.0) | (1.3) | (8.4) | |
Regarding the tumor dignity, it was evident that within the malignant and benign pancreatic tumors (excluding chronic pancreatitis patients) a comparable number of patients existed who had no abdominal pain at all (Pain 0: 49.2% vs 47.6%). However, patients with more malignant tumors showed still a significantly higher rate of moderate to severe pain (Pain II) when compared to patients with benign pancreatic lesions (14.4% vs 6.7%, P < 0.05).
Tumor grading and staging did not show any significant correlation to pain sensation in all of the analyzed pancreatic cancer cases. Patients with more advanced disease showed a tendency to suffer from more severe pain than those with earlier tumor stages (moderate/severe pain in 5.9% of pT2 tumors vs 16.0% of pT3 and 36.4% of pT4 tumors). On the other hand, most patients with pT2 tumors were pain free (61.8%) while only 47.9% of patients with pT3 and 36.4% of patients with pT4 tumors did not have any pain. We could not detect any influence of the number of lymph nodes and/or the number of metastases on the existence or severity of pancreatic pain in pancreatic cancer patients (data not shown).
Out of 314 patients with chronic pancreatitis, 225 patients had normal endocrine pancreatic function with no diabetes mellitus. 14 patients presented with latent diabetes and 58 patients with manifest diabetes. In 17 patients, the endocrine function was unknown. The additional presence of diabetes did not have any effect on pancreatic pain sensation since pain pattern of chronic pancreatitis patients with or without diabetes mellitus did not differ (data not shown).
Since recently, pain was found to be associated with impaired survival in pancreatic cancer[6], we have re-investigated this interesting phenomenon in a nearly 3 times larger study group of pancreatic cancer patients and also in the other pancreatic tumors. The survival of pancreatic cancer patients was significantly influenced by the severity of pain (P = 0.0084). Patients without pain had a 3-year survival rate of 27.9%, with mild pain 15.3%, and with moderate to severe pain a 3 year survival rate of 15.2% (Figure 1). The survival of patients with other pancreatic neoplasms was not influenced by the severity of pain (data not shown).
The present study is the currently largest study to extensively assess and compare pain sensation among the most frequent pancreatic diseases. With the attained data it becomes obvious that pancreatic pain depicts different facets and patterns of abdominal pain sensation according to the respective pancreatic disorder and does not allow a unification of the term pancreatic pain.
It has been shown that pain in pancreatic cancer is probably not as frequent as commonly stated[6]. In our study population, only 51% of patients with pancreatic cancer suffered from pain, which is even somewhat lower than the majority of previously published frequencies. But once pain is detected in pancreatic adenocarcinoma, it serves as a predictor of poor outcome, which was also the case in the presented study[4,19,20]. In all other pancreatic malignancies, where neural invasion of cancer cells is not a key pathomorphological phenomenon, no association of pain and survival was registered. We can only speculate why pancreatic cancer patients with pain do have a dismal prognosis. Besides increased neural cancer cell invasion, patients with severe pain may develop more comorbidities. They will most likely be on analgesics and narcotics and probably be not as mobile and physically fit as patients without any pain. They may therefore easier develop thrombosis and pneumonia which may further immobilize and worsen prognosis. However, since pain is a predictor of poor outcome, the sole presence of pain and especially severe pain may be used as an indication for more aggressive regional therapies such as radiotherapy or prolonged adjuvant therapies in pancreatic cancer but not in other pancreatic malignancies. When interpreting these results, however, one has to bear in mind that in the present study we only analyzed patients that were resected, meaning that there may be a bias towards less advanced, resectable tumors in our study cohort. On the other hand, 82% of patients with chronic pancreatitis suffered from pain in our study population which is similar to previously published data[1]. Also here, a possible bias towards more painful chronic pancreatitis leading to surgery has to be considered. Nevertheless, it becomes evident that pancreatic pain is very distinct and much more frequent and severe in chronic pancreatitis when compared to pancreatic cancer. It was interesting to detect, that the great majority of pancreatic disorders like serous cystadenoma, low stage neuroendocrine neoplasia, high stage neuroendocrine neoplasia, and ampullary cancer were not associated with abdominal pain at all. To our knowledge, there are no previous reports on pain patterns in these pancreatic diseases. One may speculate on the reasons why these entities are not associated with significant pain. It seems most likely, that these entities are detected rather early through symptoms other than pain (e.g., jaundice in ampullary cancer) and are consequently treated and may never get to a stage where they can cause significant pain. On the other hand it may also be the difference in tumor biology that leads to less neuropathic changes as we have previously shown[4].
The anatomic localization of the primary pancreatic tumor has a major impact on the respective pain pattern. We were able to confirm previously published data showing the highest prevalence of pain in patients with pancreatic cancer in the pancreatic body when compared to tumors in the pancreatic head or tail[21]. The underlying mechanisms for this evident phenomenon may be due to the close anatomical affiliation of the pancreatic body with the coeliac plexus and with the respective peripancreatic neural network. Abdominal pain in pancreatic cancer has a strong neuropathic component due to the characteristic intrapancreatic neuropathic alterations like neural hypertrophy, increased neural density and especially due to the prominent perineural cancer cell invasion[4,14,15,17,22,23]. The increase in neurite formation suggests that neurotropic factors, growth factors, and axonal guidance molecules can be key molecules in the development and maintenance of these phenomena. A few mediators of these neuroplastic changes have been identified, like artemin and neurturin as the members of the glial cell-derived neurotrophic factor family of ligands[17,23,24]. We have recently demonstrated that the severity of pain increases in parallel with the degree of neural invasion and that therefore the anatomic affiliation of the pancreatic body with the close nerve plexus may be one of the leading reasons for increased pain sensation in tumors at this special anatomic location. This hypothesis is underlined by the fact that in up to 70% of the cases intrapancreatic neural invasion in pancreatic cancer is directly associated with an evident extrapancreatic plexus invasion of cancer cells[25]. Furthermore, in a post mortem cadaver study pancreatic body tumors featured a special neural route to the coeliac plexus showing a direct anatomic connection[26]. Keeping these data in mind, it is not over speculated when regarding abdominal pain sensation as a reliable parameter that mirrors neuro-cancer interactions in pancreatic cancer patients. Interestingly, the other investigated pancreatic tumors showed a similar correlation between the localization in the pancreatic body and pain sensation even though these tumors are known to show significantly less neural invasion and neuroplastic changes when compared to pancreatic cancer[4]. Even though these neuropathic alterations were detected significantly less often, they were still all present in these pancreatic neoplasms[4]. Therefore, it is possible that the observed pain pattern in other pancreatic tumors may be explained by similar mechanism as in pancreatic cancer. This is moreover underlined by our finding that pain was more frequently present and more severe in patients with malignant pancreatic neoplasms as compared to their benign counterparts. Therefore, pain history should be carefully investigated since malignancy could be suspected in patients with especially severe pain states and apparently benign pancreatic neoplasms. Pain should therefore be integrated in the diagnostic workup and may help us in our indications for surgery.
Neither the TNM status nor tumor grading of the malignant tumor entities showed any significant correlation to the presence or severity of abdominal pain sensation. However, it has been previously shown that even T1 tumors can show the features of neural invasion and pain in pancreatic cancer[27]. Therefore, it seems that the size of the tumor is not terminating the extent of neuropathic alterations and that the sole presence of these neuropathic changes can lead to pancreatic pain irrespective of tumor size, grade or location.
Chronic alcohol abuse is the most common etiological factor of chronic pancreatitis. Alcoholic chronic pancreatitis was shown to be associated with more constant pain sensation as compared to non-alcoholic chronic pancreatitis which could be reproduced also in our series (data not shown)[1,28]. However, previous studies could not find a difference in the severity of pain between alcoholic and non-alcoholic chronic pancreatitis[1,28], as we found in our study. The underlying mechanisms for increased abdominal pain in alcoholic chronic pancreatitis remain to be unravelled. Although diabetes and consequent peripheral neural damage is known to largely influence general pain sensation, this does unexpectedly not seem to be the case for pancreatic pain in our study. There was no difference in pain sensation between diabetic and non-diabetic chronic pancreatitis patients in our study population. A recently published study investigated the association of diabetes in pancreatic pain in the case of pancreatic cancer. Here, the authors report that patients with diabetes had a significantly lower frequency of abdominal pain[29] with at the same time significantly higher prevalence of perineural invasion. Further studies will be needed to investigate whether diabetes as such can induce neural plasticity in pancreatic diseases.
In summary, the results of the presented study demonstrate that pain patterns in pancreatic diseases are very diverse and mainly dependent on tumor type, anatomic localization and dignity. Abdominal pain sensation in pancreatic diseases should therefore be observed and documented much more carefully since they may be used as an additional diagnostic tool to estimate pancreatic tumor dignity and patient’s prognosis.
Pain is an important symptom of both pancreatitis and pancreatic cancer, which are the most common pancreatic diseases. There are numerous other, more seldom pancreatic diseases and little is known about pain patterns in these rare conditions.
Pancreatic pain in pancreatic cancer and in chronic pancreatitis is increasingly acknowledged as of neuropathic origin. The neuroplastic changes seen in pancreatic cancer and chronic pancreatitis have not been observed to that extend in other pancreatic diseases.
This is the first study evaluating pain patterns in patients with less common pancreatic diseases. The results of the presented study demonstrate that pain patterns in pancreatic diseases are very diverse and mainly dependent on tumor type, anatomic localization and dignity.
Pain history in pancreatic diseases may be used as an additional diagnostic tool to estimate disease dignity.
Abdominal pain is a major clinical feature in chronic pancreatitis and pancreatic cancer. It is the first study about the pain patterns in all pancreatic tumors and correlate pain with the respective clinicopathological data. This study is well designed and properly performed. The statistical analysis is reasonable. The result is credible. The conclusion is helpful in clinical practice.
P- Reviewers: Camara-Lemarroy CR, Mezhir JJ, Merrett ND, Sun LM S- Editor: Gou SX L- Editor: A E- Editor: Liu XM
| 1. | Mullady DK, Yadav D, Amann ST, O’Connell MR, Barmada MM, Elta GH, Scheiman JM, Wamsteker EJ, Chey WD, Korneffel ML. Type of pain, pain-associated complications, quality of life, disability and resource utilisation in chronic pancreatitis: a prospective cohort study. Gut. 2011;60:77-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 232] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 2. | Andrén-Sandberg A, Hoem D, Gislason H. Pain management in chronic pancreatitis. Eur J Gastroenterol Hepatol. 2002;14:957-970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 71] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 3. | Ammann RW, Akovbiantz A, Largiader F, Schueler G. Course and outcome of chronic pancreatitis. Longitudinal study of a mixed medical-surgical series of 245 patients. Gastroenterology. 1984;86:820-828. [PubMed] |
| 4. | Ceyhan GO, Bergmann F, Kadihasanoglu M, Altintas B, Demir IE, Hinz U, Müller MW, Giese T, Büchler MW, Giese NA. Pancreatic neuropathy and neuropathic pain--a comprehensive pathomorphological study of 546 cases. Gastroenterology. 2009;136:177-186.e1. [PubMed] |
| 5. | Krech RL, Walsh D. Symptoms of pancreatic cancer. J Pain Symptom Manage. 1991;6:360-367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 95] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Grahm AL, Andrén-Sandberg A. Prospective evaluation of pain in exocrine pancreatic cancer. Digestion. 1997;58:542-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Ebbehøj N, Borly L, Bülow J, Rasmussen SG, Madsen P. Evaluation of pancreatic tissue fluid pressure and pain in chronic pancreatitis. A longitudinal study. Scand J Gastroenterol. 1990;25:462-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 81] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Di Sebastiano P, di Mola FF, Buchler MW, Friess H. Pathogenesis of pain in chronic pancreatitis. Dig Dis. 2004;22:267-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 9. | Barreto SG, Saccone GT. Pancreatic nociception--revisiting the physiology and pathophysiology. Pancreatology. 2012;12:104-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Demir IE, Tieftrunk E, Maak M, Friess H, Ceyhan GO. Pain mechanisms in chronic pancreatitis: of a master and his fire. Langenbecks Arch Surg. 2011;396:151-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 11. | Drewes AM, Krarup AL, Detlefsen S, Malmstrøm ML, Dimcevski G, Funch-Jensen P. Pain in chronic pancreatitis: the role of neuropathic pain mechanisms. Gut. 2008;57:1616-1627. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 127] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 12. | Bockman DE, Buchler M, Malfertheiner P, Beger HG. Analysis of nerves in chronic pancreatitis. Gastroenterology. 1988;94:1459-1469. [PubMed] |
| 13. | Ceyhan GO, Bergmann F, Kadihasanoglu M, Erkan M, Park W, Hinz U, Giese T, Müller MW, Büchler MW, Giese NA. The neurotrophic factor artemin influences the extent of neural damage and growth in chronic pancreatitis. Gut. 2007;56:534-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 84] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 14. | Ceyhan GO, Demir IE, Rauch U, Bergmann F, Müller MW, Büchler MW, Friess H, Schäfer KH. Pancreatic neuropathy results in „neural remodeling“ and altered pancreatic innervation in chronic pancreatitis and pancreatic cancer. Am J Gastroenterol. 2009;104:2555-2565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 123] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 15. | Demir IE, Ceyhan GO, Rauch U, Altintas B, Klotz M, Müller MW, Büchler MW, Friess H, Schäfer KH. The microenvironment in chronic pancreatitis and pancreatic cancer induces neuronal plasticity. Neurogastroenterol Motil. 2010;22:480-490, e112-113. [PubMed] |
| 16. | Drewes AM, Gratkowski M, Sami SA, Dimcevski G, Funch-Jensen P, Arendt-Nielsen L. Is the pain in chronic pancreatitis of neuropathic origin? Support from EEG studies during experimental pain. World J Gastroenterol. 2008;14:4020-4027. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 39] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 17. | Ceyhan GO, Giese NA, Erkan M, Kerscher AG, Wente MN, Giese T, Büchler MW, Friess H. The neurotrophic factor artemin promotes pancreatic cancer invasion. Ann Surg. 2006;244:274-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 118] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 18. | D'Haese JG, Demir IE, Kehl T, Winckler J, Giese NA, Bergmann F, Giese T, Büchler MW, Friess H, Hartel M. The impact of MFG-E8 in chronic pancreatitis: potential for future immunotherapy? BMC Gastroenterol. 2013;13:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Müller MW, Friess H, Köninger J, Martin D, Wente MN, Hinz U, Ceyhan GO, Blaha P, Kleeff J, Büchler MW. Factors influencing survival after bypass procedures in patients with advanced pancreatic adenocarcinomas. Am J Surg. 2008;195:221-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 73] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 20. | Okusaka T, Okada S, Ueno H, Ikeda M, Shimada K, Yamamoto J, Kosuge T, Yamasaki S, Fukushima N, Sakamoto M. Abdominal pain in patients with resectable pancreatic cancer with reference to clinicopathologic findings. Pancreas. 2001;22:279-284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Eyigor C, Karaca B, Kuzeyli-Yildirim Y, Uslu R, Uyar M, Coker A. Does the tumor localization in advanced pancreatic cancer have an influence on the management of symptoms and pain? J BUON. 2010;15:543-546. [PubMed] |
| 22. | Ceyhan GO, Demir IE, Altintas B, Rauch U, Thiel G, Müller MW, Giese NA, Friess H, Schäfer KH. Neural invasion in pancreatic cancer: a mutual tropism between neurons and cancer cells. Biochem Biophys Res Commun. 2008;374:442-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 116] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 23. | Ceyhan GO, Schäfer KH, Kerscher AG, Rauch U, Demir IE, Kadihasanoglu M, Böhm C, Müller MW, Büchler MW, Giese NA. Nerve growth factor and artemin are paracrine mediators of pancreatic neuropathy in pancreatic adenocarcinoma. Ann Surg. 2010;251:923-931. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 94] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 24. | Wang K, Demir IE, D’Haese JG, Tieftrunk E, Kujundzic K, Schorn S, Xing B, Kehl T, Friess H, Ceyhan GO. The neurotrophic factor neurturin contributes toward an aggressive cancer cell phenotype, neuropathic pain and neuronal plasticity in pancreatic cancer. Carcinogenesis. 2014;35:103-113. [PubMed] |
| 25. | Nakao A, Harada A, Nonami T, Kaneko T, Takagi H. Clinical significance of carcinoma invasion of the extrapancreatic nerve plexus in pancreatic cancer. Pancreas. 1996;12:357-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 152] [Cited by in RCA: 158] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 26. | Yi SQ, Miwa K, Ohta T, Kayahara M, Kitagawa H, Tanaka A, Shimokawa T, Akita K, Tanaka S. Innervation of the pancreas from the perspective of perineural invasion of pancreatic cancer. Pancreas. 2003;27:225-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 89] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 27. | Reiser-Erkan C, Gaa J, Kleeff J. T1 pancreatic cancer with lymph node metastasis and perineural invasion of the celiac trunk. Clin Gastroenterol Hepatol. 2008;6:e41-e42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 28. | Ammann RW, Muellhaupt B. The natural history of pain in alcoholic chronic pancreatitis. Gastroenterology. 1999;116:1132-1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 284] [Cited by in RCA: 234] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 29. | Sahin IH, Shama MA, Tanaka M, Abbruzzese JL, Curley SA, Hassan M, Li D. Association of diabetes and perineural invasion in pancreatic cancer. Cancer Med. 2012;1:357-362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |