Published online Jul 7, 2014. doi: 10.3748/wjg.v20.i25.8312
Revised: February 27, 2014
Accepted: April 5, 2014
Published online: July 7, 2014
Processing time: 163 Days and 10.7 Hours
Diffuse liver hemangiomatosis with giant cavernous hemangioma in adult is extremely rare. A 35 year-old woman presented to hospital with main complaint of epigastric pain and abdominal fullness. An enhanced computed tomography scan revealed a massive liver tumor in right lobe about 150 mm in size. There was contrast enhancement at the periphery of the mass consistent with a cavernous hemangioma. She underwent right hepatectomy. Histologically, it was diagnosed as a cavernous hemangioma. And also, hemangiomatous lesions were scattered around the Glisson’s capsule on the back ground liver. These hemangiomatous lesions were not recognized preoperatively. Even if we couldn’t diagnose hemangiomatosis around the main giant hemangioma preoperatively, we need to take enough surgical margins because the giant hemangioma has the potential to have small hemangiomatous lesions around the tumor. We reported right hepatectomy for giant cavernous hemangioma with diffuse hepatic hemangiomatosis without an extrahepatic lesion in an adult.
Core tip: A 35-year-old woman presented to the hospital complaining of epigastric pain and abdominal fullness. Imaging findings showed a giant cavernous hemangioma approximately 150 mm in size on right lobe of the liver. We performed right hepatectomy. Histologically, this entity was diagnosed as a cavernous hemangioma. Furthermore, hemangiomatous lesions were scattered around the Glisson’s capsule of normal liver. These hemangiomatous lesions were not recognized preoperatively. Even if we were unable to diagnose the hemangiomatosis around the giant hemangioma preoperatively, we still would have had to excise sufficiently large surgical margins, as giant hemangiomas may have small hemangiomatous lesions around the tumor.
- Citation: Ohkura Y, Hashimoto M, Lee S, Sasaki K, Matsuda M, Watanabe G. Right hepatectomy for giant cavernous hemangioma with diffuse hemangiomatosis around Glisson’s capsule. World J Gastroenterol 2014; 20(25): 8312-8316
- URL: https://www.wjgnet.com/1007-9327/full/v20/i25/8312.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i25.8312
Liver cavernous hemangiomas are the most common benign tumor of the liver. On autopsy, their incidence ranges from 5% to 20%[1,2]. Most hemangiomas are small in size (< 4 cm in diameter) and remain asymptomatic, requiring no treatment. Giant hemangiomas present a different disease course. In many surgical series, giant hemangiomas are defined as cavernous hemangiomas larger than 4 cm in diameter[3]. Symptoms rarely appear unless the tumor size exceeds 4 cm. Symptomatic hepatic hemangiomas can present with abdominal pain, hemorrhage, biliary compression, or consumptive coagulopathy.
Diffuse hepatic hemangiomatosis usually occurs in neonates with an abdominal mass and unidentified congestive heart failure. The disease is associated with Rendu-Osler-Weber disease or skeletal hemangiomatosis[4,5].
Isolated diffuse hemangiomatosis of the liver in adults without extrahepatic lesions is extremely rare[6]. We report on a right hepatectomy for giant cavernous hemangioma with diffuse hepatic hemangiomatosis in the background of the liver but without an extrahepatic lesion in adults.
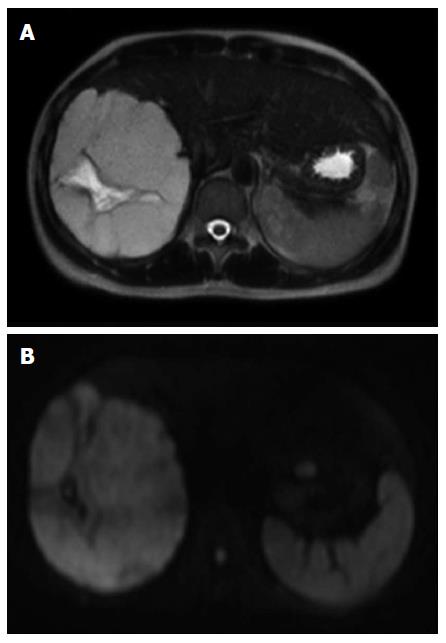
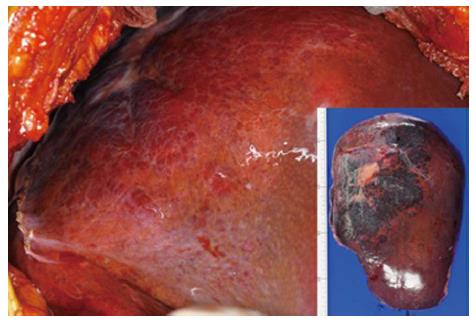
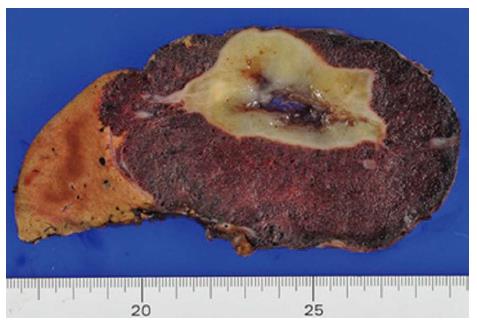
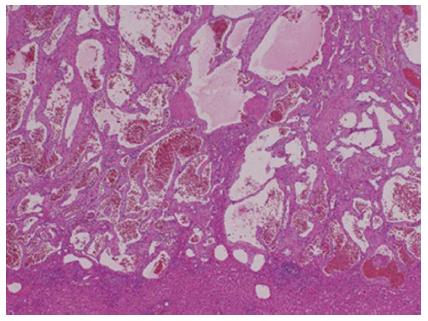
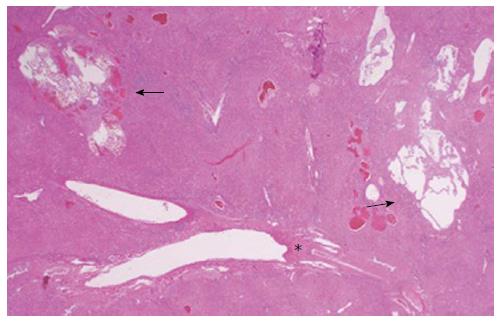
In April 2013, a 35-year-old woman presented to a nearby hospital with main complaint of epigastric pain and a sense of abdominal fullness. She was 151 cm tall and weighed 52 kg. Her past or family medical history was unremarkable. On physical examination, abdominal distension and severe tenderness were present. She has no jaundice. The results of blood routine and liver function tests were normal, including a platelet count of 18 × 104 platelets/mL. Serum tumor markers were all within the normal range. Hepatitis B and C virus markers were negative. On examination, she had a massive liver tumor on the right lobe of liver that was approximately 145 mm in size, with areas of necrosis inside of the liver according to abdominal ultrasonography. A Doppler ultrasonography revealed no remarkable tumor vascularities, except for the underlying hepatic parenchymal vascular flow. An enhanced computed tomography (CT) scan revealed a massive liver tumor in the right lobe of her liver, 153 mm × 133 mm × 95 mm in size. There was contrast enhancement at the periphery of the mass consistent with a cavernous hemangioma. A coronal view of the mass is shown in Figure 1. The massive liver tumor showed low signal intensity on T1-weighted Magnetic Resonance Imaging (MRI), high intensity on T2-weighted MRI, and high intensity on diffusion MRI (Figure 2). These image assessments were highly suggestive of a diagnosis of a giant hepatic hemangioma. The clinical and radiological evaluation showed no evidence of Rendu-Osler-Weber disease or hemangiomas in the extrahepatic region. She was referred to our hospital for treatment. She preferred surgery, so she underwent laparotomy; a right hepatectomy was performed. The duration of the operation was 190 min, and the intraoperative blood loss was 845 mL. The resected tumor was 200 mm × 140 mm × 85 mm in size and 910 g in weight (Figure 3). Figure 4 shows sections of the resected tumor, with a white area of 105 mm × 62 mm in size. Histologically, a cavernous hemangioma was diagnosed (Figure 5). The white area showed tumor degeneration and a loss of tumor cells. Hemangiomatous lesions were scattered around the Glisson’s capsule on the background of the liver (Figure 6). These hemangiomatous lesions were not recognized preoperatively. The patient’s post-operative course was uneventful, and she was discharged from the hospital 9 d postoperatively.
Cavernous hemangiomas of the liver are benign and usually small (< 4 cm) in size, but when they are larger than 4 cm in diameter, they are classified as giant cavernous hemangiomas[7]. Cavernous hemangiomas of the liver are the most common type of liver tumor and are most frequently seen in women. Most hemangiomas are asymptomatic and are detected incidentally on the imaging of the abdomen for unrelated reasons. A large hemangioma and diffuse hemangiomatosis present symptoms of abdominal pain, discomfort, and palpable mass.
A recent major argument in the treatment of liver hemangiomas is the indication of the operation. Considering the benign and non-progressive nature of the disease, it is currently accepted that the diagnosis of giant hemangioma is not necessarily an indication for surgery based on its size alone, and continued observations in asymptomatic patients or in patients with minimal abdominal symptoms appear to be justified[8]. Surgery remains the only consistently effective curative treatment for giant hemangiomas. However, Kayan et al[9] reported that the combination of preoperative percutaneous trans-catheter arterial embolization (TAE) and surgery is a safe procedure that eliminates the risk of intraoperative bleeding in the treatment of giant hepatic hemangiomas.
Hepatectomy may be accomplished by a simple enucleation or an anatomical resection. Operative series comparing enucleation and lobectomy have shown that complications, such as bleeding from damage to blood vessels and bile duct injury, were significantly more common and more serious after lobectomy. Therefore, enucleation is preferred when feasible for symptomatic giant hemangiomas[10]. In our case, the giant hemangioma was observed very near to middle hepatic vein, so we selected a right hepatectomy. Histologically, this entity was diagnosed as a giant cavernous hemangioma, 20 cm in size. Scattered small hemangiomatous lesions were found in the background of the liver with a cavernous hemangioma. In particular, they were scattered around the Glisson’s capsule. We diagnosed the hemangiomatosis, but these hemangiomatous lesions were not recognized preoperatively.
Hepatic hemangiomatosis may be a rare condition characterized by the diffuse replacement of the hepatic parenchyma with hemangiomatous lesions and can sometimes be associated with systemic hemangiomatosis[11]. The natural history and underlying etiology of diffuse hepatic hemangiomatosis remain uncertain. Diffuse hepatic hemangiomatosis has been reported in relation with hereditary hemorrhagic telangiectasia[5]. Hereditary hemorrhagic telangiectasia, also called Rendu-Osler-Weber disease, is a systemic fibrovascular dysplasia with autosomal dominant inheritance. In our patient, there were no clinical features of Rendu-Osler-Weber disease. In infancy, hemangiomatosis usually involves the entire liver, in a diffuse fashion. On the other hand, in adults, diffuse liver hemangiomatosis alone is extremely rare without extrahepatic lesions. Only a few patients with isolated liver hemangiomatosis have been reported in the English literature[6,12].
Previous reports have cited the role of steroid medications in the development of hepatic cavernous hemangiomas[13] and the administration of metoclopramide medications in a patient with diffuse hepatic hemangiomatosis. No history of steroid or estrogen use was documented in the reported cases of diffuse hepatic hemangiomatosis[14].
Cavernous hemangioma is the most common benign hepatic tumor and is typically described as a solitary, well-circumscribed lesion with a distinct fibrous interface; therefore, hepatic parenchymas are usually not included in cavernous hemangiomas[15]. Scattered hemangioma-like vessels in the hepatocellular nodular lesions were found in the present patients and resembled the findings that were described in the background liver of a cavernous hemangioma[16]. Jhaveri et al[17] reported on the association of hepatic hemangiomatosis with a giant cavernous hemangioma in an adult population. These hemangiomatosis were diagnosed in imaging tests, including abdominal ultrasonography, CT, MRI, among others; however, in our case, hemangiomatosis was not recognized preoperatively.
The management strategy for giant hepatic hemangiomas can differ depending on the presence of associated hemangiomatosis and on the amount and distribution of the residual hepatic parenchyma[17]. As previously explained, enucleation is preferred when feasible for symptomatic giant hemangiomas due to the potential for complications from surgery. However, surgical candidates must be carefully selected to avoid surgical complications related to excessive blood loss from oozing due to the deroofing of the areas of hemangiomatosis after the enucleation of a giant hepatic hemangioma[17].
Symptomatic patients with giant hemangiomas and associated extensive hemangiomatosis can be difficult subjects for enucleation and are better managed by means of an extensive lobectomy. Because we were unable to diagnose the hemangiomatosis around the main giant hemangioma preoperatively, we needed to use large surgical margins, as the giant hemangioma may have small hemangiomatous lesions around the tumor. Although there have been no previous reports of these accessory lesions, if we can decrease main tumor size, shrinkage or disappear hemangiomatosis around main tumor by TAE, we may be able to resect smaller range of the liver.
In conclusion, we reported on a right hepatectomy for a giant cavernous hemangioma with diffuse hepatic hemangiomatosis in the liver background without extrahepatic lesions in an adult. Further research and examinations of similar cases are required to confirm this relationship and to further assess the clinical significance of a giant cavernous hemangioma with diffuse hepatic hemangiomatosis in adults.
A 35-year-old woman presented to nearby hospital with main complaint of epigastric pain and a sense of abdominal fullness.
Diagnosis of a giant cavernous hemangioma of the liver.
Hepatocellular carcinoma, Focal nodular hyperplasia
She results of blood routine and liver function tests were normal, including platelet count of 18 × 104 platelets/mL, and serum tumor markers and hepatitis B and C virus markers were all within normal range.
Computed tomography scan revealed a massive liver tumor in right lobe of liver, 153 mm × 133 mm × 95 mm in size and there was contrast enhancement at the periphery of the mass consistent with a cavernous hemangioma.
It was diagnosed as a cavernous hemangioma and also hemangiomatous lesions were scattered around the Glisson’s capsule on the back ground liver
This reported on a right hepatectomy for a giant cavernous hemangioma with diffuse hepatic hemangiomatosis in the liver background without extrahepatic lesions in an adult.
Because we were unable to diagnose the hemangiomatosis around the main giant hemangioma preoperatively, they needed to use large surgical margins, as the giant hemangioma may have small hemangiomatous lesions around the tumor.
This make reference to surgical precaution and operative procedures of giant cavernous hemangioma with hemangiomatosis following pathological findings in their report.
P- Reviewers: Kanda T, Lorber A, Stanojevic GZ S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
| 1. | Weimann A, Ringe B, Klempnauer J, Lamesch P, Gratz KF, Prokop M, Maschek H, Tusch G, Pichlmayr R. Benign liver tumors: differential diagnosis and indications for surgery. World J Surg. 1997;21:983-990; discussion 990-991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 184] [Cited by in RCA: 178] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 2. | Ishak KG, Rabin L. Benign tumors of the liver. Med Clin North Am. 1975;59:995-1013. [PubMed] |
| 3. | Adam YG, Huvos AG, Fortner JG. Giant hemangiomas of the liver. Ann Surg. 1970;172:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 161] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Gutierrez RM, Spjut HJ. Skeletal angiomatosis: report of three cases and review of the literature. Clin Orthop Relat Res. 1972;85:82-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 51] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Haitjema T, Westermann CJ, Overtoom TT, Timmer R, Disch F, Mauser H, Lammers JW. Hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease): new insights in pathogenesis, complications, and treatment. Arch Intern Med. 1996;156:714-719. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 83] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Lehmann FS, Beglinger C, Schnabel K, Terracciano L. Progressive development of diffuse liver hemangiomatosis. J Hepatol. 1999;30:951-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Mungovan JA, Cronan JJ, Vacarro J. Hepatic cavernous hemangiomas: lack of enlargement over time. Radiology. 1994;191:111-113. [PubMed] |
| 8. | Zhou JX, Huang JW, Wu H, Zeng Y. Successful liver resection in a giant hemangioma with intestinal obstruction after embolization. World J Gastroenterol. 2013;19:2974-2978. [PubMed] |
| 9. | Kayan M, Cetin M, Aktaş AR, Yilmaz O, Ceylan E, Eroğlu HE. Pre-operative arterial embolization of symptomatic giant hemangioma of the liver. Prague Med Rep. 2012;113:166-171. [PubMed] |
| 10. | Lerner SM, Hiatt JR, Salamandra J, Chen PW, Farmer DG, Ghobrial RM, Busuttil RW. Giant cavernous liver hemangiomas: effect of operative approach on outcome. Arch Surg. 2004;139:818-821; discussion 821-823. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 80] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Vilgrain V, Boulos L, Vullierme MP, Denys A, Terris B, Menu Y. Imaging of atypical hemangiomas of the liver with pathologic correlation. Radiographics. 2000;20:379-397. [PubMed] |
| 12. | Moon WS, Yu HC, Lee JM, Kang MJ. Diffuse hepatic hemangiomatosis in an adult. J Korean Med Sci. 2000;15:471-474. [PubMed] |
| 13. | Conter RL, Longmire WP. Recurrent hepatic hemangiomas. Possible association with estrogen therapy. Ann Surg. 1988;207:115-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 78] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Feurle GE. Arteriovenous shunting and cholestasis in hepatic hemangiomatosis associated with metoclopramide. Gastroenterology. 1990;99:258-262. [PubMed] |
| 15. | Miettinen M, Fletcher C, Kindblom L, Zimmermann A, Tsui W. Mesenchymal tumours of the liver. WHO classification of tumours of the digestive system. 4th ed. Lyon: IARC 2010; 241-250. |
| 16. | Sasaki M, Ikeda T, Hatanaka KC, Nakanuma Y. Hyperplastic hepatocellular nodule with localized hemangiomatosis: A hither-to unrecognized type of hypervascular hepatic lesion. Hepatol Res. 2013;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Jhaveri KS, Vlachou PA, Guindi M, Fischer S, Khalili K, Cleary SP, Ayyappan AP. Association of hepatic hemangiomatosis with giant cavernous hemangioma in the adult population: prevalence, imaging appearance, and relevance. AJR Am J Roentgenol. 2011;196:809-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |