Published online Jun 28, 2014. doi: 10.3748/wjg.v20.i24.7984
Revised: February 14, 2014
Accepted: March 8, 2014
Published online: June 28, 2014
Processing time: 192 Days and 21.1 Hours
An anastomotic leak is one of the major complications following colorectal surgery. Standard treatments for anastomotic leak are total parenteral nutrition or temporary ileostomy. The over-the-scope-clipping (OTSC) system was originally developed to treat intestinal perforation or to close the tissue after natural orifice transluminal endoscopic surgery. Two cases of successful management of an anastomotic leak after colorectal surgery using the OTSC system are reported. One patient avoided a temporary ileostomy. In the other, hospitalization was shortened by the use of the OTSC system. The OTSC system can be a potential option in the management of anastomotic leaks after colorectal surgery.
Core tip: Standard treatments for anastomotic leak after colorectal surgery are total parenteral nutrition or temporary ileostomy. The over-the-scope-clipping (OTSC) system was originally developed to treat intestinal perforation or to close the tissue after natural orifice transluminal endoscopic surgery. The OTSC system can be a potential option in the management of anastomotic leaks after colorectal surgery to avoid ileostomy.
- Citation: Kobayashi H, Kikuchi A, Okazaki S, Ishiguro M, Ishikawa T, Iida S, Uetake H, Sugihara K. Over-the-scope-clipping system for anastomotic leak after colorectal surgery: Report of two cases. World J Gastroenterol 2014; 20(24): 7984-7987
- URL: https://www.wjgnet.com/1007-9327/full/v20/i24/7984.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i24.7984
Colorectal cancer is one of the malignant tumors that is increasing in Japan[1,2]. Curative resection with lymphadenectomy is a standard treatment for colorectal cancer[3]. An anastomotic leak is one of the major complications after colorectal anastomosis, which is more common in low anterior resection than other colonic anastomoses. Standard treatments for an anastomotic leak are total parenteral nutrition or temporary ileostomy.
The over-the-scope-clipping (OTSC) system was made of super-elastic Nitinol and a tissue-approximating double-jaw endoscopic grasper. It was originally developed for closing the gastrointestinal perforation or the orifice in natural orifice transluminal endoscopic surger[4,5]. The OTSC system consists of an applicator cap with a mounted OTSC clip, thread, thread retriever and a handwheel for clip release. The clip is released as the target bowel wall is suctioned or anchored.
Two patients for whom the OTSC system was useful in the management of an anastomotic leak after colorectal surgery are reported.
A 58-year-old female with diabetes mellitus was admitted due to weight loss. Clinical examinations disclosed large rectal cancer with bilateral hydronephrosis and paraaortic lymph node metastases. After placing bilateral ureteral stents and creating a transverse colostomy, systemic chemotherapy was started.
After six courses of modified FOLFOX 6 plus panitumumab and three courses without oxaliplatin because of peripheral neuropathy, CT showed a partial response, and low anterior resection with D3 lymph node dissection was performed. The distance from anal verge to the anastomosis was 7 cm. The stoma of the transverse colon was not closed because she had a high risk of anastomotic leak caused by the diabetes mellitus and her condition after cytotoxic chemotherapy.
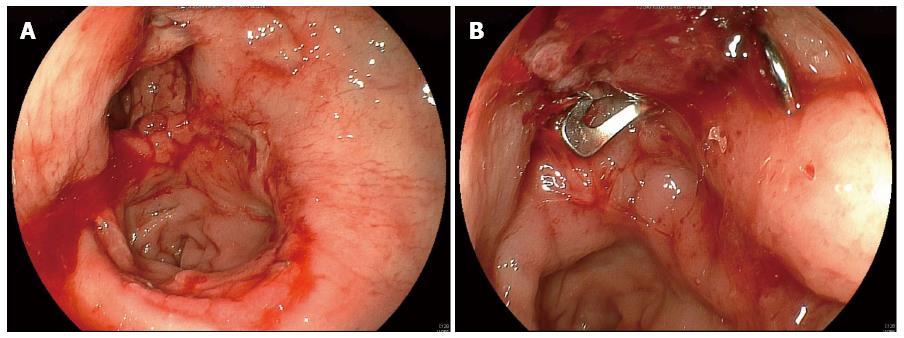
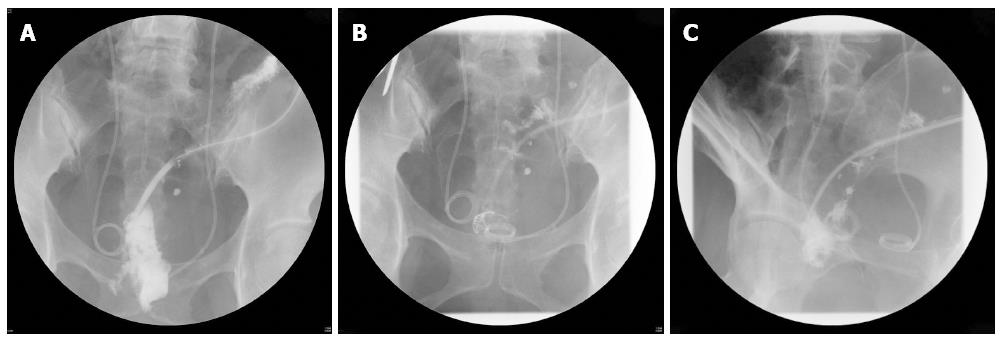
An anastomotic leak developed on the 5th postoperative day. Since she had the stoma of the transverse colon, conservative therapy was continued. Although irrigation of the abscess cavity was started from the 7th postoperative day, the abscess cavity was not improved. Closure of the breakdown site by the OTSC system was performed on the 22nd postoperative day (Figure 1). Contrast radiography through the drain two days after the OTSC system procedure demonstrated marked shrinkage of the abscess cavity (Figure 2). The drain was removed three days after the OTSC system procedure, and she was discharged from the hospital four days after the OTSC system procedure.
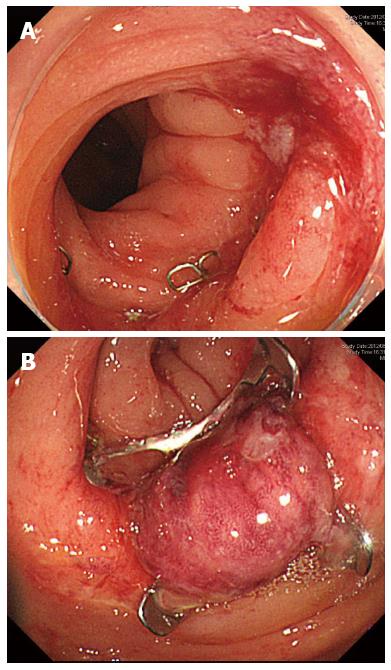
A 50-year-old woman with sigmoid colon cancer of T3N0M0 was referred to our hospital. She underwent laparoscopic sigmoidectomy with D3 lymph node dissection, and the anastomosis was created by the double stapling technique. The distance from anal verge to anastomosis was 12 cm. On the 7th postoperative day, a diatrizoate meglumine enema examination that was performed due to fever revealed a minor anastomotic leak (Figure 3). At that time, she had already started food intake, and the drain had been removed. Since she did not have any abdominal symptoms, conservative treatment with total parenteral nutrition was chosen, and she had neither abdominal symptoms nor fever. After restarting oral food intake on the 27th postoperative day, fever developed, and total parenteral nutrition was continued again until food intake was restarted on the 35th postoperative day. However, she developed fever again. Closure of the anastomotic leak using the OTSC system was tried on the 37th postoperative day (Figure 4). She successfully restarted oral food intake on the 45th postoperative day and was discharged on the 51st postoperative day.
When patients after colorectal surgery develop an anastomotic leak, it is common to perform total parenteral nutrition or temporary ileostomy. The irrigation of the abscess cavity through the drain was performed, because the drain had been inserted in the first patient. Since the abscess cavity was not improved despite two weeks’ lavage, closure of the anastomotic leak using the OTSC system was attempted. After this procedure, the abscess cavity shrank remarkably. One of the reasons for the delay in the improvement of the abscess cavity in this patient would be her post cytotoxic chemotherapy condition. The OTSC system procedure for closure of the anastomotic leak may be useful in patients after chemotherapy.
In the second patient, conservative therapy was chosen because of the minor leak and the absence of abdominal pain. However, she developed fever after restarting oral food intake. Successful closure of the anastomotic leak was achieved using the OTSC system. The problem in this patient was removal of the drain. At first, the patient had a good postoperative course, and the drain was removed after oral food intake was started. However, an abdominal abscess around the anastomosis was detected by CT after drain removal. One of the reasons for the delay in the improvement of the anastomotic leak might have been the removal of the drain. When we perform colonoscopy in patients with an anastomotic leak, air and water may be diffused into the abdomen, especially in patients without a drain. Therefore, the insufflation should be minimal, and carbon dioxide should be used.
Weiland et al[6] reported in their review that the success rate of the OTSC system procedure was 84.6%. However, the usefulness of the OTSC system for an anastomotic leak following colorectal surgery has not been reported, except for the report of Arezzo et al[7]. In their study, the OTSC system was applied in 14 patients with anastomotic leaks following colorectal surgery. Of the 14 patients, eight were acute cases and six were chronic. Their indications for use of the OTSC system for the closure of anastomotic leaks were size of breakdown less than 15 mm in diameter, no abscess outside the bowel, and no bowel obstruction. In our experience, however, even with an abscess in the abdomen, closure of the breakdown site using the OTSC system may be possible when a drain is inserted appropriately.
The OTSC system may have cost benefit compared with temporary ileostomy. When the patient with anastomotic leak after colorectal surgery undergoes temporary ileostomy, the expenses of stoma apparatus and stoma closure must be paid. The OTSC system may reduce the medical expenses in patients with anastomotic leak after colorectal surgery. On the other hand, there is a possibility of complications during the procedure of the OTSC such as perforation and mucosal laceration, because the tissue is friable under the inflammation. However, the advantage of OTSC system is full thickness wall closure. These issues should be clarified in the future.
Two patients in whom an anastomotic leak after colorectal surgery was successfully managed by closure using the OTSC system were described. The OTSC system was useful in shortening the hospital stay and in avoiding a temporary ileostomy. It is important to accumulate experience regarding the usefulness of the OTSC system in patients with an anastomotic leak after colorectal surgery.
Two patients with anastomotic leak after colorectal surgery were treated with the over-the-scope-clipping (OTSC) system to avoid temporary ileostomy.
Anastomotic leak after colorectal surgery.
In these cases, no differential diagnosis was made.
Blood tests were within normal limits.
Contrast radiography showed leak after double stapling technique.
Both patients had colorectal adenocarcinoma before surgery.
The patients were treated with the OTSC system.
The OTSC system can be a potential option in the management of anastomotic leaks after colorectal surgery.
This article applies the OTSC system to the management of patients with anastomotic leak after colorectal surgery.
P- Reviewers: Chatzimavroudis G, Kang SB, Morino M, Milito G S- Editor: Ma YJ L- Editor: A E- Editor: Wang CH
| 1. | Kotake K, Honjo S, Sugihara K, Kato T, Kodaira S, Takahashi T, Yasutomi M, Muto T, Koyama Y. Changes in colorectal cancer during a 20-year period: an extended report from the multi-institutional registry of large bowel cancer, Japan. Dis Colon Rectum. 2003;46:S32-S43. [PubMed] |
| 2. | Muto T, Kotake K, Koyama Y. Colorectal cancer statistics in Japan: data from JSCCR registration, 1974-1993. Int J Clin Oncol. 2001;6:171-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol. 2012;17:1-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 528] [Cited by in RCA: 597] [Article Influence: 42.6] [Reference Citation Analysis (0)] |
| 4. | Schurr MO, Arezzo A, Ho CN, Anhoeck G, Buess G, Di Lorenzo N. The OTSC clip for endoscopic organ closure in NOTES: device and technique. Minim Invasive Ther Allied Technol. 2008;17:262-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 5. | Schurr MO, Hartmann C, Ho CN, Fleisch C, Kirschniak A. An over-the-scope clip (OTSC) system for closure of iatrogenic colon perforations: results of an experimental survival study in pigs. Endoscopy. 2008;40:584-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 6. | Weiland T, Fehlker M, Gottwald T, Schurr MO. Performance of the OTSC System in the endoscopic closure of gastrointestinal fistulae--a meta-analysis. Minim Invasive Ther Allied Technol. 2012;21:249-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 33] [Article Influence: 2.5] [Reference Citation Analysis (2)] |
| 7. | Arezzo A, Verra M, Reddavid R, Cravero F, Bonino MA, Morino M. Efficacy of the over-the-scope clip (OTSC) for treatment of colorectal postsurgical leaks and fistulas. Surg Endosc. 2012;26:3330-3333. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |