Published online Jun 28, 2014. doi: 10.3748/wjg.v20.i24.7777
Revised: December 31, 2013
Accepted: March 8, 2014
Published online: June 28, 2014
Processing time: 244 Days and 9.5 Hours
Obesity is an increasingly serious health problem in nearly all Western countries. It represents an important risk factor for several gastrointestinal diseases, such as gastroesophageal reflux disease, erosive esophagitis, hiatal hernia, Barrett’s esophagus, esophageal adenocarcinoma, Helicobacter pylori infection, colorectal polyps and cancer, non-alcoholic fatty liver disease, cirrhosis, and hepatocellular carcinoma. Surgery is the most effective treatment to date, resulting in sustainable and significant weight loss, along with the resolution of metabolic comorbidities in up to 80% of cases. Many of these conditions can be clinically relevant and have a significant impact on patients undergoing bariatric surgery. There is evidence that the chosen procedure might be changed if specific pathological upper gastrointestinal findings, such as large hiatal hernia or Barrett’s esophagus, are detected preoperatively. The value of a routine endoscopy before bariatric surgery in asymptomatic patients (screening esophagogastroduodenoscopy) remains controversial. The common indications for endoscopy in the postoperative bariatric patient include the evaluation of symptoms, the management of complications, and the evaluation of weight loss failure. It is of critical importance for the endoscopist to be familiar with the postoperative anatomy and to work in close collaboration with bariatric surgery colleagues in order to maximize the outcome and safety of endoscopy in this setting. The purpose of this article is to review the role of the endoscopist in a multidisciplinary obesity center as it pertains to the preoperative and postoperative management of bariatric surgery patients.
Core tip: Gastrointestinal endoscopists play an integral role in the multidisciplinary treatment of obese patients undergoing bariatric surgery, particularly in the treatment of postoperative complications. Endoscopy is emerging as an effective procedure in the treatment of bariatric surgery complications in selected patients, while avoiding invasive surgical reoperation.
- Citation: De Palma GD, Forestieri P. Role of endoscopy in the bariatric surgery of patients. World J Gastroenterol 2014; 20(24): 7777-7784
- URL: https://www.wjgnet.com/1007-9327/full/v20/i24/7777.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i24.7777
Obesity is an increasingly serious health problem in nearly all Western countries. Estimates of prevalence suggest that 7%-15% of subjects in developed countries are obese[1-8].
Obesity is usually defined in terms of body mass index (BMI, kg/m2). The World Health Organization, the National Institutes of Health, Healthy People 2010, and the 2000 Dietary Guidelines for Americans, proposed guidelines for the classification of weight status based on the BMI[9-11]. Accordingly, a BMI of 25-30 is considered overweight, a BMI of 30 to 35 is considered class 1 obesity, 35-40 as class 2, and over 40 as class 3. Morbid obesity is usually defined as a BMI of over 40 or a BMI over 35 in combination with comorbidities. Underweight is usually defined as a BMI of less than 18.5 kg/m2.
Obesity is an independent risk factor for a variety of chronic diseases such as diabetes, hypertension, coronary heart disease, knee osteoarthritis, and cancer[12-18]. A recent study on the association between different grades of obesity and the number of life-years lost indicated that life expectancy can be up to 20 years shorter in severe obesity[19].
Intentional weight loss offers substantial benefits to patients and is associated with an overall reduction in mortality[20]. Current treatment modalities for obesity include lifestyle modification, diet, and pharmacologic agents; however, their effectiveness and durability is limited[21]. Surgery is the most effective treatment to date, resulting in sustainable and significant weight loss along with the resolution of metabolic comorbidities in up to 80% of cases[22-24].
The next frontier in the treatment of obesity might be represented by the development of endoscopic approaches to bariatric procedures[25-31]. Endoluminal surgery, performed entirely by using flexible endoscopes, offers the potential for less invasive approaches that may be safer and more cost-effective compared with current laparoscopic approaches, thus extending surgical indications to those with multiple comorbidities, older age, and those with mild obesity (BMI: 30-35).
The purpose of this article is to review the role of the endoscopist in the preoperative and postoperative management of bariatric surgery patients, in the context of a multidisciplinary obesity center.
Obesity is an important risk factor for several digestive diseases, such as gastroesophageal reflux disease, erosive esophagitis, hiatal hernia (HH), Barrett’s esophagus, esophageal adenocarcinoma, Helicobacter pylori infection, colorectal polyps and cancer, non-alcoholic fatty liver disease (NAFLD), cirrhosis, and hepatocellular carcinoma. Most of these diseases are observed up to 2-3 times more frequently in obese patients than in normal weight individuals[32].
Many of these conditions can be clinically relevant and have a significant impact on patients undergoing bariatric surgery. There is evidence that the chosen procedure might be changed if specific pathological upper GI findings, such as a large HH or Barrett’s esophagus, are detected preoperatively.
The published guidelines of the European Association for Endoscopic Surgery state that esophagogastroduodenoscopy (EGDS), or upper-GI series, is advisable for all bariatric procedures and strongly recommended for gastric bypass patients [Roux-en-Y gastric bypass (RYGB)]. Similarly, the recently published guidelines from the ASGE recommended that EGDS should be performed in all symptomatic patients undergoing bariatric surgery, and considered in all candidates[33,34]. Symptomatic patients should undergo EGDS (diagnostic) in accordance with accepted practice guidelines, regardless of whether they are being considered for bariatric surgery or not.
The value of a routine endoscopy before bariatric surgery in asymptomatic patients (screening EGDS) remains controversial[35]. A lack of correlation between patient symptoms and endoscopic findings has been documented by many authors, suggesting that routine preoperative endoscopy might be useful in detecting both lesions and inflammation[36-40]. However, considering the relatively weak clinical relevance of the majority of lesions discovered on routine EGDS and the cost and invasiveness of the procedure, as well as the amount of secondary unnecessary workup prompted by irrelevant findings, several authors have instead advocated a non-endoscopic approach for asymptomatic patients[41,42].
One of the concerns of performing routine preoperative upper endoscopy is the risk of sedation. Cardiopulmonary complications are the most serious adverse reactions associated with conscious sedation at the time of EGDS, with a mortality rate of 0.03% and a serious morbidity rate of 0.54%[43]. In cases of morbidly obese patients, the risk may be higher due to the higher incidence of restrictive lung disease, obstructive sleep apnea, pulmonary hypertension, and cardiac diseases. It is of paramount importance that endoscopy procedures in obese patients are carried out in a fully equipped setting and by a well-organized team of anesthetists trained in the use of anesthetic drugs and in the treatment of adverse events.
Several surgical procedures are currently performed to induce weight loss in obese patients. These procedures have been simplified into three categories: predominantly restrictive procedures, predominantly malabsorptive procedures, and combined procedures (Table 1).
| Predominantly restrictive | Predominantly malabsorptive | Mixed |
| Vertical banded gastroplasty | Biliopancreatic diversion | Gastric bypass surgery |
| Adjustable gastric band | Sleeve gastrectomy with duodenal switch | |
| Sleeve gastrectomy | ||
| Gastric plication |
The common indications for endoscopy in postoperative bariatric patients include the evaluation of symptoms, the management of complications, and the evaluation of weight loss failure.
Of critical importance is for the endoscopist to be familiar with the postoperative anatomy and work in close collaboration with bariatric surgery colleagues to maximize outcomes and the safety of endoscopy in this setting[44].
Although nausea, vomiting, and abdominal pain are commonly encountered symptoms after bariatric surgery and may result from dietary non-compliance, patients with persistent symptoms should be evaluated, as these symptoms may indicate the development of a complication, especially within the first 6 postoperative months.
Each procedure is associated with specific GI complications (Table 2).
| Intervention | Complications |
| Banded gastroplasty | Band erosion |
| Adjustable gastric banding | Band erosion |
| Overinflated band | |
| Roux-en-Y gastric bypass | Gastrointestinal bleeding |
| Marginal ulceration | |
| Anastomotic leak and fistula | |
| Gastrojejunal stricture | |
| Biliary-pancreatic diversion and duodenal switch | Anastomotic leak, fistula and stricture |
Gastrointestinal complications prompting endoscopy after surgery may be summarized as follow: acute bleeding and/or anemia, staple-line complications (such as anastomotic leaks, fistulae, and strictures), band stenosis, erosion and slippage, bezoars, and choledocholithiasis.
An endoscopy is the preferred strategy, unless there is a suspicion of leaks or fistulae, in which case preliminary contrast radiography may be more appropriate.
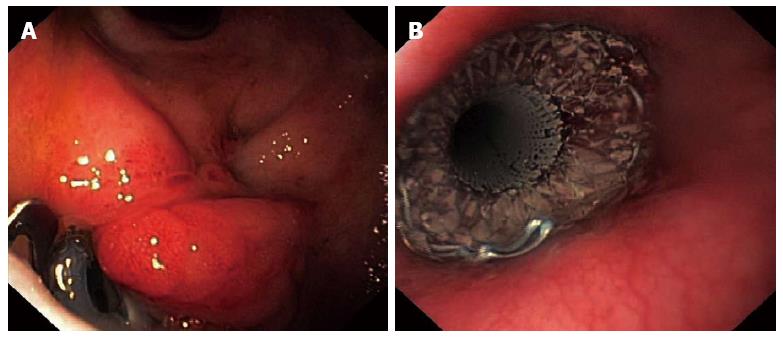
Early upper hemorrhage (within 48 h) are mostly reported after laparoscopic RYGB surgery (1%-4%)[45-49]. The bleeding lesions are often identified at the staple lines of the gastrojejunostomy and rarely at the jejunojejunostomy, gastric pouch, or bypassed stomach. Although there are few published case series, endoscopic management of hemorrhage from the gastrojejunal anastomosis has been shown to be highly successful when using standard hemostatic modalities[50-53]. Late hemorrhage may often arise from marginal ulcers or erosion (Figures 1 and 2), and generally requires medical therapy (PPIs) or, in cases of acute bleeding, endoscopic treatment. Balloon enteroscopy has been reported in patients with GI bleeding arising from the bypassed stomach, but should be undertaken only with great caution[54-56].
Endoscopic treatment plays an important role in the management of a variety of staple-line complications, such as stomal stenosis and anastomotic leaks.
Stricture of the gastrojejunal anastomosis: Stricture of the gastrojejunal anastomosis resulting in dysphagia, vomiting, and nutritional deficiencies, is a relatively common late complication of both open and laparoscopic RYGBP, occurring in approximately 3% to 12% of patients after RYGB[57-61].
There is no formal definition of stricture size, but generally an anastomosis with a diameter < 10 mm or the inability to allow passage of a standard upper endoscope (diameter 8.6-9.8 mm) is considered a significant stricture.
Endoscopic dilation of stomal stenosis via through-the scope balloon dilation or wire-guided bougie dilation is safe and highly effective, and should be considered the primary treatment for this complication[62-67]. The majority of patients can be successfully treated with 1 or 2 sessions, and surgical revision is rarely necessary[62].
A potential risk of stricture dilation is inadvertent over-dilatation, leading to weight regain. Overall, it appears that stricture dilation to a maximum of 15 mm is not associated with impaired postoperative weight loss outcomes[62,68].
Staple-line dehiscence, or leak formation: Staple-line dehiscence, or leak formation can lead to abdominal pain, thoracic pain nausea, vomiting, intra-abdominal abscess, and acute peritonitis.
Leak rates vary by type of surgical intervention, with large series reporting 2.05% to 5.20% for laparoscopic RYGB, and 1.68% to 2.60% for open RYGB. Sleeve gastrectomy has an associated leak rate of 0.6% to 7%[49,58,59,69-73].
The most common sites for RYGB leaks are at the gastrojejunal anastomosis, followed by the jejunojejunostomy anastomosis; in sleeve gastrectomy, leaks usually occur at the proximal border within 2 cm of the angle of His.
The first step is the treatment of sepsis and supportive care, including total parenteral nutrition and transcutaneous drainage catheter placement. Some leaks may resolve with these conservative steps. For stable patients in whom conservative management has failed, laparoscopic repair should be considered. Additionally, in these patients, endoscopy is emerging as an effective procedure in the treatment of anastomotic leakage, while avoiding invasive surgical reoperation.
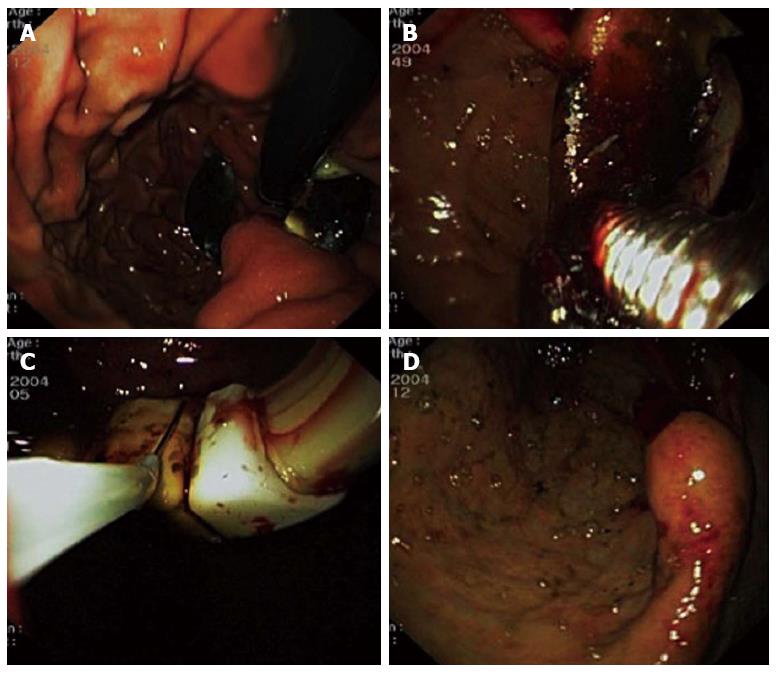
Chronic leaks have been successfully repaired endoscopically by using fibrin-glue injection[74-76], clip placement[77], self-expanding stents[78-82], and endoscopic suturing devices[83] (Figure 3).
Although endoscopic therapy for gastric leak management holds promise, these procedures cannot be routinely recommended, due to the lack of controlled data.
The laparoscopic adjustable gastric band (LAGB) is well-established as a safe, effective, and durable bariatric procedure[84-86].
Several complications are related to LAGB, including reflux esophagitis, stenosis with esophageal dilation, band slippage, and erosion.
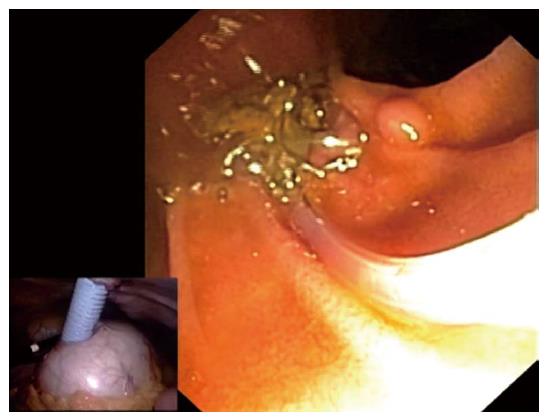
LAGB erosions typically occur 1-2 years after placement. The prevalence varies in published studies from 0.9% to 3.8%[86-88]. Gastric band erosion may occur with abdominal pain, nausea, vomiting, abdominal access port-site infection, increased food intake, or weight gain, and is easily identified with endoscopy. The traditional approach is surgical revision; however, there are reports of conservative management with endoscopic removal on complete intragastric erosion[89-92] (Figure 4).
Morbid obesity is a risk factor for gallstone formation, and rapid weight loss is an independent and potentially compounding risk factor[93-95].
Whereas an endoscopic retrograde cholangiopancreatography (ERCP) can usually be performed after gastric banding or sleeve gastrectomy, an ERCP in a patient with an RYGB presents significant technical challenges.
Several options are available to gain access to the biliary tree in patients after RYGB. Laparoscopic creation of a point of access to the gastric remnant or small bowel allows the duodenoscope to reach the papilla, but carries the inherent risks of general anesthesia and surgery[96-100] (Figure 5). Enteroscopes, colonoscopes, and more recent double-balloon and single-balloon endoscopes have also been used. However, duct cannulation is difficult with the forward-viewing enteroscope, and precut biliary sphincterotomy is often required. Furthermore, accessories are limited due to the length of the enteroscope[101-107].
GI endoscopists play an integral role in the multidisciplinary treatment of obese patients undergoing bariatric surgery, particularly in the treatment of postoperative complications. Direct communication and coordination with the surgical team is critical in the preoperative and immediate postoperative setting. Endoscopy is emerging as an effective procedure in the treatment of bariatric surgery complications in selected patients, while avoiding invasive surgical reoperation.
P- Reviewers: Abd Ellatif, ME, Hirahara N, Luigiano C, Shibata T S- Editor: Ma YJ L- Editor: Rutherford A E- Editor: Zhang DN
| 1. | Laurier D, Guiguet M, Chau NP, Wells JA, Valleron AJ. Prevalence of obesity: a comparative survey in France, the United Kingdom and the United States. Int J Obes Relat Metab Disord. 1992;16:565-572. [PubMed] |
| 2. | Epstein FH, Higgins M. Human obesity: general aspects. Epidemiology of Obesity. Philadelphia: JB Lippincott 1992; 330-342. |
| 3. | Mendez MA, Monteiro CA, Popkin BM. Overweight exceeds underweight among women in most developing countries. Am J Clin Nutr. 2005;81:714-721. [PubMed] |
| 4. | Malik VS, Willett WC, Hu FB. Global obesity: trends, risk factors and policy implications. Nat Rev Endocrinol. 2013;9:13-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 841] [Cited by in RCA: 887] [Article Influence: 73.9] [Reference Citation Analysis (0)] |
| 5. | Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes. 2006;1:11-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1705] [Cited by in RCA: 1639] [Article Influence: 91.1] [Reference Citation Analysis (0)] |
| 6. | Sturm R. Stemming the global obesity epidemic: what can we learn from data about social and economic trends? Public Health. 2008;122:739-746. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | James WP. The fundamental drivers of the obesity epidemic. Obes Rev. 2008;9 Suppl 1:6-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 92] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 8. | Kopelman PG. Obesity as a medical problem. Nature. 2000;404:635-643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3230] [Cited by in RCA: 3130] [Article Influence: 125.2] [Reference Citation Analysis (0)] |
| 9. | Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obes Res. 1998;6 Suppl 2:51S-209S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 890] [Cited by in RCA: 763] [Article Influence: 28.3] [Reference Citation Analysis (0)] |
| 10. | US Department of Health and Human Services. Healthy People 2010. Washington, DC: US Government Printing Office 2000; Available from: http://www.healthypeople.gov/document/html/uih/uih_4.htm#overandobese. |
| 11. | US Department of Agriculture and US Department of Health and Human Services. Nutrition and Your Health: Dietary Guidelines for Americans. 5th ed. Washington, DC: US Government Printing Office 2000; Home and Garden Bulletin no. 232. |
| 12. | Rippe JM, Crossley S, Ringer R. Obesity as a chronic disease: modern medical and lifestyle management. J Am Diet Assoc. 1998;98:S9-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 123] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 13. | Compston J. Obesity and bone. Curr Osteoporos Rep. 2013;11:30-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 71] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 14. | Gu W, Chen C, Zhao KN. Obesity-associated endometrial and cervical cancers. Front Biosci (Elite Ed). 2013;5:109-118. [PubMed] |
| 15. | Aleksandrova K, Nimptsch K, Pischon T. Obesity and colorectal cancer. Front Biosci (Elite Ed). 2013;5:61-77. [PubMed] |
| 16. | Cheraghi Z, Poorolajal J, Hashem T, Esmailnasab N, Doosti Irani A. Effect of body mass index on breast cancer during premenopausal and postmenopausal periods: a meta-analysis. PLoS One. 2012;7:e51446. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 179] [Cited by in RCA: 186] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 17. | Allott EH, Masko EM, Freedland SJ. Obesity and prostate cancer: weighing the evidence. Eur Urol. 2013;63:800-809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 417] [Article Influence: 32.1] [Reference Citation Analysis (0)] |
| 18. | Preston SH, Mehta NK, Stokes A. Modeling obesity histories in cohort analyses of health and mortality. Epidemiology. 2013;24:158-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 54] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 19. | Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289:187-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1546] [Cited by in RCA: 1436] [Article Influence: 65.3] [Reference Citation Analysis (0)] |
| 20. | Astrup A. Healthy lifestyles in Europe: prevention of obesity and type II diabetes by diet and physical activity. Public Health Nutr. 2001;4:499-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 135] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 21. | Padwal R, Li SK, Lau DC. Long-term pharmacotherapy for obesity and overweight. Cochrane Database Syst Rev. 2003;CD004094. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 102] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 22. | Gastrointestinal surgery for severe obesity: National Institutes of Health Consensus Development Conference Statement. Am J Clin Nutr. 1992;55:615S-619S. [PubMed] |
| 23. | Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724-1737. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5073] [Cited by in RCA: 4713] [Article Influence: 224.4] [Reference Citation Analysis (1)] |
| 24. | Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ, Bantle JP, Sledge I. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248-256.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1816] [Cited by in RCA: 1734] [Article Influence: 108.4] [Reference Citation Analysis (0)] |
| 25. | Stimac D, Majanović SK. Endoscopic approaches to obesity. Dig Dis. 2012;30:187-195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Coté GA, Edmundowicz SA. Emerging technology: endoluminal treatment of obesity. Gastrointest Endosc. 2009;70:991-999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 27. | Swidnicka-Siergiejko A, Wróblewski E, Andrzej D. Endoscopic treatment of obesity. Can J Gastroenterol. 2011;25:627-633. [PubMed] |
| 28. | Tsesmeli N, Coumaros D. The future of bariatrics: endoscopy, endoluminal surgery, and natural orifice transluminal endoscopic surgery. Endoscopy. 2010;42:155-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 29. | Kethu SR, Banerjee S, Barth BA, Desilets DJ, Kaul V, Pedrosa MC, Pfau PR, Pleskow DK, Tokar JL, Wang A. Endoluminal bariatric techniques. Gastrointest Endosc. 2012;76:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 30. | Kumar N, Thompson CC. Endoscopic solutions for weight loss. Curr Opin Gastroenterol. 2011;27:407-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 31. | Singhal S, Le DL, Duddempudi S, Anand S. The role of endoscopy in bariatrics: past, present, and future. J Laparoendosc Adv Surg Tech A. 2012;22:802-811. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 32. | Gerson LB. Impact of obesity on endoscopy. Gastrointest Endosc. 2009;70:758-762. [PubMed] [DOI] [Full Text] |
| 33. | Sauerland S, Angrisani L, Belachew M, Chevallier JM, Favretti F, Finer N, Fingerhut A, Garcia Caballero M, Guisado Macias JA, Mittermair R. Obesity surgery: evidence-based guidelines of the European Association for Endoscopic Surgery (EAES). Surg Endosc. 2005;19:200-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 282] [Cited by in RCA: 259] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 34. | Anderson MA, Gan SI, Fanelli RD, Baron TH, Banerjee S, Cash BD, Dominitz JA, Harrison ME, Ikenberry SO, Jagannath SB. Role of endoscopy in the bariatric surgery patient. Gastrointest Endosc. 2008;68:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 83] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 35. | Martin M. Routine preoperative endoscopy: necessity or excess? Surg Obes Relat Dis. 2008;4:713-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 36. | Sharaf RN, Weinshel EH, Bini EJ, Rosenberg J, Sherman A, Ren CJ. Endoscopy plays an important preoperative role in bariatric surgery. Obes Surg. 2004;14:1367-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 122] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 37. | Muñoz R, Ibáñez L, Salinas J, Escalona A, Pérez G, Pimentel F, Guzmán S, Boza C. Importance of routine preoperative upper GI endoscopy: why all patients should be evaluated? Obes Surg. 2009;19:427-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 69] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 38. | Csendes A, Burgos AM, Smok G, Beltran M. Endoscopic and histologic findings of the foregut in 426 patients with morbid obesity. Obes Surg. 2007;17:28-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 73] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 39. | Küper MA, Kratt T, Kramer KM, Zdichavsky M, Schneider JH, Glatzle J, Stüker D, Königsrainer A, Brücher BL. Effort, safety, and findings of routine preoperative endoscopic evaluation of morbidly obese patients undergoing bariatric surgery. Surg Endosc. 2010;24:1996-2001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 40. | de Moura Almeida A, Cotrim HP, Santos AS, Bitencourt AG, Barbosa DB, Lobo AP, Rios A, Alves E. Preoperative upper gastrointestinal endoscopy in obese patients undergoing bariatric surgery: is it necessary? Surg Obes Relat Dis. 2008;4:144-149; discussion 150-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 41. | Loewen M, Giovanni J, Barba C. Screening endoscopy before bariatric surgery: a series of 448 patients. Surg Obes Relat Dis. 2008;4:709-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 80] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 42. | Peromaa-Haavisto P, Victorzon M. Is routine preoperative upper GI endoscopy needed prior to gastric bypass? Obes Surg. 2013;23:736-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 43. | Arrowsmith JB, Gerstman BB, Fleischer DE, Benjamin SB. Results from the American Society for Gastrointestinal Endoscopy/U.S. Food and Drug Administration collaborative study on complication rates and drug use during gastrointestinal endoscopy. Gastrointest Endosc. 1991;37:421-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 363] [Cited by in RCA: 320] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 44. | Stellato TA, Crouse C, Hallowell PT. Bariatric surgery: Creating new challenges for the endoscopist. Gastrointest Endosc. 2003;57:86-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 45. | Azagury DE, Lautz DB. Endoscopic techniques in bariatric patients: Obesity basics and normal postbariatric surgery anatomy. Tech Gastrointest Endosc. 2010;12:124-129. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 46. | Spaw AT, Husted JD. Bleeding after laparoscopic gastric bypass: Case report and literature review. Surg Obes Relat Dis. 2005;1:99-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 47. | Nguyen NT, Longoria M, Chalifoux S, Wilson SE. Gastrointestinal hemorrhage after laparoscopic gastric bypass. Obes Surg. 2004;14:1308-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 48. | Steffen R. Early gastrointestinal hemorrhage after laparoscopic gastric bypass. Obes Surg. 2003;13:466; author reply 466-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 49. | Podnos YD, Jimenez JC, Wilson SE, Stevens CM, Nguyen NT. Complications after laparoscopic gastric bypass: a review of 3464 cases. Arch Surg. 2003;138:957-961. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 541] [Cited by in RCA: 448] [Article Influence: 20.4] [Reference Citation Analysis (0)] |
| 50. | Ferreira LE, Song LM, Baron TH. Management of acute postoperative hemorrhage in the bariatric patient. Gastrointest Endosc Clin N Am. 2011;21:287-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 51. | Jamil LH, Krause KR, Chengelis DL, Jury RP, Jackson CM, Cannon ME, Duffy MC. Endoscopic management of early upper gastrointestinal hemorrhage following laparoscopic Roux-en-Y gastric bypass. Am J Gastroenterol. 2008;103:86-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 52. | Fernández-Esparrach G, Bordas JM, Pellisé M, Gimeno-García AZ, Lacy A, Delgado S, Cárdenas A, Ginès A, Sendino O, Momblán D. Endoscopic management of early GI hemorrhage after laparoscopic gastric bypass. Gastrointest Endosc. 2008;67:552-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 53. | Moretto M, Mottin CC, Padoin AV, Berleze D, Repetto G. Endoscopic management of bleeding after gastric bypass -- a therapeutic alternative. Obes Surg. 2004;14:706. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 54. | Tang SJ, Rivas H, Tang L, Lara LF, Sreenarasimhaiah J, Rockey DC. Endoscopic hemostasis using endoclip in early gastrointestinal hemorrhage after gastric bypass surgery. Obes Surg. 2007;17:1261-1267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 55. | Tagaya N, Kasama K, Inamine S, Zaha O, Kanke K, Fujii Y, Kanehira E, Hiraishi H, Kubota K. Evaluation of the excluded stomach by double-balloon endoscopy after laparoscopic Roux-en-Y gastric bypass. Obes Surg. 2007;17:1165-1170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 56. | Kuga R, Safatle-Ribeiro AV, Sakai P. Utility of Double Balloon Endoscopy for the Diagnosis and Treatment of Stomach and Small Intestine Disorders in Patients with Gastric Bypass. Tech Gastrointest Endosc. 2008;10:136-140. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 57. | Csendes A, Burgos AM, Burdiles P. Incidence of anastomotic strictures after gastric bypass: a prospective consecutive routine endoscopic study 1 month and 17 months after surgery in 441 patients with morbid obesity. Obes Surg. 2009;19:269-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 58. | Sanyal AJ, Sugerman HJ, Kellum JM, Engle KM, Wolfe L. Stomal complications of gastric bypass: incidence and outcome of therapy. Am J Gastroenterol. 1992;87:1165-1169. [PubMed] |
| 59. | Blachar A, Federle MP. Gastrointestinal complications of laparoscopic roux-en-Y gastric bypass surgery in patients who are morbidly obese: findings on radiography and CT. AJR Am J Roentgenol. 2002;179:1437-1442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 85] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 60. | Nguyen NT, Stevens CM, Wolfe BM. Incidence and outcome of anastomotic stricture after laparoscopic gastric bypass. J Gastrointest Surg. 2003;7:997-1003; discussion 1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 125] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 61. | Goitein D, Papasavas PK, Gagné D, Ahmad S, Caushaj PF. Gastrojejunal strictures following laparoscopic Roux-en-Y gastric bypass for morbid obesity. Surg Endosc. 2005;19:628-632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 62. | Peifer KJ, Shiels AJ, Azar R, Rivera RE, Eagon JC, Jonnalagadda S. Successful endoscopic management of gastrojejunal anastomotic strictures after Roux-en-Y gastric bypass. Gastrointest Endosc. 2007;66:248-252. [PubMed] |
| 63. | Ukleja A, Afonso BB, Pimentel R, Szomstein S, Rosenthal R. Outcome of endoscopic balloon dilation of strictures after laparoscopic gastric bypass. Surg Endosc. 2008;22:1746-1750. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 114] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 64. | Ahmad J, Martin J, Ikramuddin S, Schauer P, Slivka A. Endoscopic balloon dilation of gastroenteric anastomotic stricture after laparoscopic gastric bypass. Endoscopy. 2003;35:725-728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 77] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 65. | Barba CA, Butensky MS, Lorenzo M, Newman R. Endoscopic dilation of gastroesophageal anastomosis stricture after gastric bypass. Surg Endosc. 2003;17:416-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 70] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 66. | Sataloff DM, Lieber CP, Seinige UL. Strictures following gastric stapling for morbid obesity. Results of endoscopic dilatation. Am Surg. 1990;56:167-174. [PubMed] |
| 67. | Kretzschmar CS, Hamilton JW, Wissler DW, Yale CE, Morrissey JF. Balloon dilation for the treatment of stomal stenosis complicating gastric surgery for morbid obesity. Surgery. 1987;102:443-446. [PubMed] |
| 68. | Swartz DE, Gonzalez V, Felix EL. Anastomotic stenosis after Roux-en-Y gastric bypass: A rational approach to treatment. Surg Obes Relat Dis. 2006;2:632-636; discussion 637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 69. | Gagner M, Deitel M, Kalberer TL, Erickson AL, Crosby RD. The Second International Consensus Summit for Sleeve Gastrectomy, March 19-21, 2009. Surg Obes Relat Dis. 2009;5:476-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 256] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 70. | Nocca D, Krawczykowsky D, Bomans B, Noël P, Picot MC, Blanc PM, de Seguin de Hons C, Millat B, Gagner M, Monnier L. A prospective multicenter study of 163 sleeve gastrectomies: results at 1 and 2 years. Obes Surg. 2008;18:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 219] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 71. | Fuks D, Verhaeghe P, Brehant O, Sabbagh C, Dumont F, Riboulot M, Delcenserie R, Regimbeau JM. Results of laparoscopic sleeve gastrectomy: a prospective study in 135 patients with morbid obesity. Surgery. 2009;145:106-113. [PubMed] |
| 72. | Aurora AR, Khaitan L, Saber AA. Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients. Surg Endosc. 2012;26:1509-1515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 427] [Cited by in RCA: 439] [Article Influence: 31.4] [Reference Citation Analysis (0)] |
| 73. | Stroh C, Birk D, Flade-Kuthe R, Frenken M, Herbig B, Höhne S, Köhler H, Lange V, Ludwig K, Matkowitz R. Results of sleeve gastrectomy-data from a nationwide survey on bariatric surgery in Germany. Obes Surg. 2009;19:632-640. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 74. | Liu CD, Glantz GJ, Livingston EH. Fibrin glue as a sealant for high-risk anastomosis in surgery for morbid obesity. Obes Surg. 2003;13:45-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 72] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 75. | Kowalski C, Kastuar S, Mehta V, Brolin RE. Endoscopic injection of fibrin sealant in repair of gastrojejunostomy leak after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2007;3:438-442. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 76. | Papavramidis ST, Eleftheriadis EE, Apostolidis DN, Kotzampassi KE. Endoscopic fibrin sealing of high-output non-healing gastrocutaneous fistulas after vertical gastroplasty in morbidly obese patients. Obes Surg. 2001;11:766-769. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 77. | Iacopini F, Di Lorenzo N, Altorio F, Schurr MO, Scozzarro A. Over-the-scope clip closure of two chronic fistulas after gastric band penetration. World J Gastroenterol. 2010;16:1665-1669. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 42] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 78. | Eisendrath P, Cremer M, Himpens J, Cadière GB, Le Moine O, Devière J. Endotherapy including temporary stenting of fistulas of the upper gastrointestinal tract after laparoscopic bariatric surgery. Endoscopy. 2007;39:625-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 172] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 79. | Eubanks S, Edwards CA, Fearing NM, Ramaswamy A, de la Torre RA, Thaler KJ, Miedema BW, Scott JS. Use of endoscopic stents to treat anastomotic complications after bariatric surgery. J Am Coll Surg. 2008;206:935-98; discussion 935-98;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 161] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 80. | Nguyen NT, Nguyen XM, Dholakia C. The use of endoscopic stent in management of leaks after sleeve gastrectomy. Obes Surg. 2010;20:1289-1292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 63] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 81. | Serra C, Baltasar A, Andreo L, Pérez N, Bou R, Bengochea M, Chisbert JJ. Treatment of gastric leaks with coated self-expanding stents after sleeve gastrectomy. Obes Surg. 2007;17:866-872. [PubMed] |
| 82. | Puli SR, Spofford IS, Thompson CC. Use of self-expandable stents in the treatment of bariatric surgery leaks: a systematic review and meta-analysis. Gastrointest Endosc. 2012;75:287-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 124] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 83. | Overcash WT. Natural orifice surgery (NOS) using StomaphyX for repair of gastric leaks after bariatric revisions. Obes Surg. 2008;18:882-885. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 84. | Favretti F, Ashton D, Busetto L, Segato G, De Luca M. The gastric band: first-choice procedure for obesity surgery. World J Surg. 2009;33:2039-2048. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 56] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 85. | Favretti F, Segato G, Ashton D, Busetto L, De Luca M, Mazza M, Ceoloni A, Banzato O, Calo E, Enzi G. Laparoscopic adjustable gastric banding in 1,791 consecutive obese patients: 12-year results. Obes Surg. 2007;17:168-175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 173] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 86. | Weiner R, Blanco-Engert R, Weiner S, Matkowitz R, Schaefer L, Pomhoff I. Outcome after laparoscopic adjustable gastric banding - 8 years experience. Obes Surg. 2003;13:427-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 176] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 87. | Moreno P, Alastrué A, Rull M, Formiguera X, Casas D, Boix J, Fernández-Llamazares J, Broggi MA. Band erosion in patients who have undergone vertical banded gastroplasty: incidence and technical solutions. Arch Surg. 1998;133:189-193. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 88. | Abu-Abeid S, Szold A. Results and complications of laparoscopic adjustable gastric banding: an early and intermediate experience. Obes Surg. 1999;9:188-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 89. | Evans JA, Williams NN, Chan EP, Kochman ML. Endoscopic removal of eroded bands in vertical banded gastroplasty: a novel use of endoscopic scissors (with video). Gastrointest Endosc. 2006;64:801-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 90. | De Palma GD, Formato A, Pilone V, Rega M, Giuliano ME, Simeoli I, Forestieri P. Endoscopic management of intragastric penetrated adjustable gastric band for morbid obesity. World J Gastroenterol. 2006;12:4098-4100. [PubMed] |
| 91. | Chisholm J, Kitan N, Toouli J, Kow L. Gastric band erosion in 63 cases: endoscopic removal and rebanding evaluated. Obes Surg. 2011;21:1676-1681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 92. | Nocca D, Frering V, Gallix B, de Seguin des Hons C, Noël P, Foulonge MA, Millat B, Fabre JM. Migration of adjustable gastric banding from a cohort study of 4236 patients. Surg Endosc. 2005;19:947-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 93. | Shiffman ML, Sugerman HJ, Kellum JM, Brewer WH, Moore EW. Gallstone formation after rapid weight loss: a prospective study in patients undergoing gastric bypass surgery for treatment of morbid obesity. Am J Gastroenterol. 1991;86:1000-1005. [PubMed] |
| 94. | Shiffman ML, Sugerman HJ, Kellum JM, Moore EW. Changes in gallbladder bile composition following gallstone formation and weight reduction. Gastroenterology. 1992;103:214-221. [PubMed] |
| 95. | Amaral JF, Thompson WR. Gallbladder disease in the morbidly obese. Am J Surg. 1985;149:551-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 124] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 96. | Peters M, Papasavas PK, Caushaj PF, Kania RJ, Gagné DJ. Laparoscopic transgastric endoscopic retrograde cholangiopancreatography for benign common bile duct stricture after Roux-en-Y gastric bypass. Surg Endosc. 2002;16:1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 67] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 97. | Pimentel RR, Mehran A, Szomstein S, Rosenthal R. Laparoscopy-assisted transgastrostomy ERCP after bariatric surgery: case report of a novel approach. Gastrointest Endosc. 2004;59:325-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 58] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 98. | Nguyen NT, Hinojosa MW, Slone J, Lee J, Khiatani V, Wilson SE. Laparoscopic transgastric access to the biliary tree after Roux-en-Y gastric bypass. Obes Surg. 2007;17:416-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 99. | Ceppa FA, Gagné DJ, Papasavas PK, Caushaj PF. Laparoscopic transgastric endoscopy after Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2007;3:21-24. [PubMed] |
| 100. | Roberts KE, Panait L, Duffy AJ, Jamidar PA, Bell RL. Laparoscopic-assisted transgastric endoscopy: current indications and future implications. JSLS. 2008;12:30-36. [PubMed] |
| 101. | Gostout CJ, Bender CE. Cholangiopancreatography, sphincterotomy, and common duct stone removal via Roux-en-Y limb enteroscopy. Gastroenterology. 1988;95:156-163. [PubMed] |
| 102. | Hintze RE, Adler A, Veltzke W, Abou-Rebyeh H. Endoscopic access to the papilla of Vater for endoscopic retrograde cholangiopancreatography in patients with billroth II or Roux-en-Y gastrojejunostomy. Endoscopy. 1997;29:69-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 146] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 103. | Chu YC, Yang CC, Yeh YH, Chen CH, Yueh SK. Double-balloon enteroscopy application in biliary tract disease-its therapeutic and diagnostic functions. Gastrointest Endosc. 2008;68:585-591. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 68] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 104. | Koornstra JJ. Double balloon enteroscopy for endoscopic retrograde cholangiopancreaticography after Roux-en-Y reconstruction: case series and review of the literature. Neth J Med. 2008;66:275-279. [PubMed] |
| 105. | Aabakken L, Bretthauer M, Line PD. Double-balloon enteroscopy for endoscopic retrograde cholangiography in patients with a Roux-en-Y anastomosis. Endoscopy. 2007;39:1068-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 151] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 106. | Haruta H, Yamamoto H, Mizuta K, Kita Y, Uno T, Egami S, Hishikawa S, Sugano K, Kawarasaki H. A case of successful enteroscopic balloon dilation for late anastomotic stricture of choledochojejunostomy after living donor liver transplantation. Liver Transpl. 2005;11:1608-1610. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 99] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 107. | Emmett DS, Mallat DB. Double-balloon ERCP in patients who have undergone Roux-en-Y surgery: a case series. Gastrointest Endosc. 2007;66:1038-1041. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 139] [Article Influence: 7.7] [Reference Citation Analysis (0)] |