Published online Mar 28, 2014. doi: 10.3748/wjg.v20.i12.3388
Revised: January 13, 2014
Accepted: February 20, 2014
Published online: March 28, 2014
Processing time: 134 Days and 14 Hours
Fishbones are the most commonly ingested foreign bodies that cause gastrointestinal tract penetration. However, fishbones embedded in the gastrointestinal tract that lead to foreign body granulomas that mimic submucosal tumors are rare. Herein, we describe a 56-year-old woman who presented with a 20-day-history of upper abdominal pain. Endoscopy revealed an elevated lesion in the gastric antrum. An abdominal computed tomography scan showed a mass in the gastric antrum and a linear calcified lesion in the mass. An endoscopic ultrasonography examination revealed a 3.9 cm × 2.2 cm, irregular, hypoechoic mass with indistinct margins in the muscularis propria layer. The patient was initially diagnosed as having a submucosal tumor, and subsequent surgical resection showed that the lesion was a foreign body granuloma caused by an embedded fishbone. Our case indicated that the differential diagnosis of a foreign body granuloma should be considered in cases of elevated lesions in the gastrointestinal tract.
Core tip: Gastric foreign body granulomas caused by embedded fishbones that mimic submucosal tumors are rare. A gastric intestinal stromal tumor, gastric leiomyoma, and gastric neurofibroma should be considered as differential diagnoses. A computed tomography scan is the most sensitive diagnostic choice, and endoscopic ultrasonography can also be helpful for diagnosis.
- Citation: Shan GD, Chen ZP, Xu YS, Liu XQ, Gao Y, Hu FL, Fang Y, Xu CF, Xu GQ. Gastric foreign body granuloma caused by an embedded fishbone: A case report. World J Gastroenterol 2014; 20(12): 3388-3390
- URL: https://www.wjgnet.com/1007-9327/full/v20/i12/3388.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i12.3388
In countries where fish is often consumed, fishbones are the most commonly ingested foreign bodies that become impacted in the upper gastrointestinal tract[1]. When a foreign body becomes impacted in the upper gastrointestinal tract, 80%-90% of cases resolve spontaneously. However, 10%-20% require nonoperative intervention, and 1% or fewer require surgery[2]. However, the chronic lodging of a foreign body in the gastrointestinal tract is rare, especially in the stomach. Here, we report a case of a gastric foreign body granuloma caused by an embedded fishbone that presented with upper abdominal pain. Endoscopy and a computed tomography (CT) scan revealed an elevated lesion in the gastric antrum, which was suspected to be a submucosal gastric tumor. Subsequent surgical resection showed that the lesion was caused by an embedded fishbone.
A 56-year-old woman presented with a 20-d-history of upper abdominal pain. The pain had developed gradually over a 20-d-period, with left back radiation. No vomiting or weight loss was reported. She was a farmer without a significant past medical history or a family history of malignancy. Physical examination and routine blood tests, including tumor markers and inflammatory markers, showed no abnormalities. An impression of chronic gastritis was made, and upper gastrointestinal endoscopy was arranged.
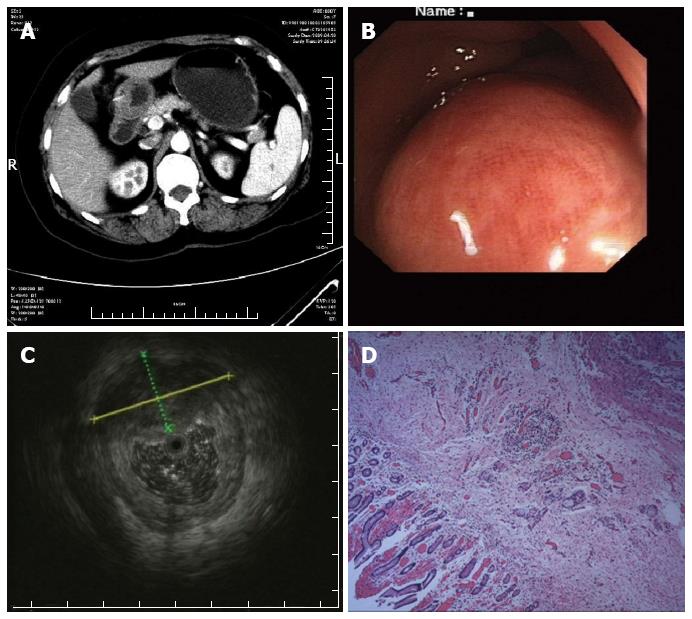
The endoscopy revealed an elevated lesion in the gastric antrum, and histopathological examination of a biopsy specimen showed mild chronic inflammatory changes and mild intestinal metaplasia. An abdominal CT scan showed a mass in the gastric antrum and a linear calcified lesion in the mass (Figure 1A). A subsequent endoscopic ultrasonography (EUS) examination revealed a 3.9 cm × 2.2 cm, irregular, hypoechoic mass with indistinct margins in the muscularis propria layer. EUS also revealed that the mucosal and submucosal layers were mildly thickened, whereas the other layers, the peripheral gastric wall, and the regional lymph nodes were not involved (Figure 1B and C).
A diagnosis of a suspected submucosal gastric tumor was made. The patient underwent uneventful distal gastrectomy. Histopathological examination of the resected specimen showed that the suspected tumor was a foreign body granuloma surrounding an embedded fishbone (Figure 1D).
Fishbones embedded in the stomach wall, forming elevated submucosal lesions that mimic submucosal tumors, are rare. Because the symptoms and signs are vague and nonspecific, the accurate diagnosis of an embedded fishbone remains a challenge for clinicians. Gastric cancer, gastric intestinal stromal tumors, gastric leiomyoma, gastric neurofibroma, and gastric tuberculosis should be considered as differential diagnoses of a gastric foreign body granuloma.
Endoscopy with biopsy is a common method for diagnosing a gastric mucosal lesion. However, regarding gastric submucosal lesions, endoscopic biopsies are usually small and superficial, and it is difficult to obtain a clear diagnosis. In the present case, histopathological examination of an endoscopic biopsy specimen revealed mild chronic inflammatory changes and mild intestinal metaplasia. To improve the endoscopic diagnosis of a submucosal lesion, forceps biopsy, endoscopic mucosal resection, or endoscopic submucosal dissection should be considered.
EUS is a valuable diagnostic tool for submucosal tumors and for the detection of foreign bodies in the gastric wall[3]. A fishbone presents as a hyperechoic focus on EUS and can appear as a fine needle when the echo is in parallel with the fishbone. However, in the patient described here, 360-degree EUS was performed, and only a cross-section of the fishbone was observed; this hyperechoic spot was confused with calcification and necrosis. Therefore, longitudinal EUS can have greater sensitivity for the diagnosis of an embedded fishbone than 360-degree EUS.
CT is a useful tool for diagnosing foreign bodies impacted in the gastrointestinal tract. According to previous studies, CT detects impacted fishbones in the esophagus with a sensitivity of 90.9%-100% and a specificity of 100%[1,4,5]. A fishbone will usually present as a linear calcified lesion on CT images[6]. In the present case, the CT scan also revealed a linear calcified lesion in the stomach mass.
Endoscopic removal of the fishbone was impossible in this patient because the bone was invisible on the stomach surface. Surgery is usually preferred for patients with embedded fishbones. However, if the embedded fishbone is relatively superior, with an absence of peritonism, endoscopic retrieval might also be possible. In a case of gastric perforation caused by a chicken bone, endoscopic extraction and clipping were successfully performed without peritoneal irritation[7].
In conclusion, embedded fishbones are rare causes of gastric foreign body granulomas. A CT scan is the most sensitive diagnostic choice, and EUS can also be helpful for diagnosis.
A 56-year-old woman presented with a 20-d-history of upper abdominal pain.
An impression of chronic gastritis was made.
A gastric intestinal stromal tumor, gastric leiomyoma, or gastric neurofibroma.
Routine blood tests, including tests for tumor markers and inflammatory markers, showed no abnormalities.
An abdominal computed tomography scan showed a mass in the gastric antrum and a linear calcified lesion in the mass.
Histopathological examination of the resected specimen showed that the suspected tumor was a foreign body granuloma surrounding an embedded fishbone.
The patient underwent uneventful distal gastrectomy.
To our knowledge, no cases of gastric foreign body granulomas caused by embedded fishbones have been reported previously.
A foreign body granuloma occurs due to prolonged exposure to an endogenous or exogenous inflammatory agent. Under these conditions, the mononuclear macrophage system is activated, and foreign bodies steadily accumulate cell infiltrates due to the action of adhesion molecules and chemokines.
The case indicated that the differential diagnosis of a foreign body granuloma should be considered in cases of elevated lesions in the gastrointestinal tract.
The authors present a strange case of a foreign body (fishbone) in the gastric wall that simulated a gastric tumor. The case is quite interesting.
P- Reviewers: Biondi A, Loffredo L, Yonem O S- Editor: Gou SX L- Editor: A E- Editor: Wu HL
| 1. | Watanabe K, Kikuchi T, Katori Y, Fujiwara H, Sugita R, Takasaka T, Hashimoto S. The usefulness of computed tomography in the diagnosis of impacted fish bones in the oesophagus. J Laryngol Otol. 1998;112:360-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Ginsberg GG. Management of ingested foreign objects and food bolus impactions. Gastrointest Endosc. 1995;41:33-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 168] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 3. | Park SR, Lee JS, Kim CG, Kim HK, Kook MC, Kim YW, Ryu KW, Lee JH, Bae JM, Choi IJ. Endoscopic ultrasound and computed tomography in restaging and predicting prognosis after neoadjuvant chemotherapy in patients with locally advanced gastric cancer. Cancer. 2008;112:2368-2376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 4. | Akazawa Y, Watanabe S, Nobukiyo S, Iwatake H, Seki Y, Umehara T, Tsutsumi K, Koizuka I. The management of possible fishbone ingestion. Auris Nasus Larynx. 2004;31:413-416. [PubMed] |
| 5. | Eliashar R, Dano I, Dangoor E, Braverman I, Sichel JY. Computed tomography diagnosis of esophageal bone impaction: a prospective study. Ann Otol Rhinol Laryngol. 1999;108:708-710. [PubMed] |
| 6. | Goh BK, Tan YM, Lin SE, Chow PK, Cheah FK, Ooi LL, Wong WK. CT in the preoperative diagnosis of fish bone perforation of the gastrointestinal tract. AJR Am J Roentgenol. 2006;187:710-714. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 137] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 7. | Ngan JH, Fok PJ, Lai EC, Branicki FJ, Wong J. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg. 1990;211:459-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 167] [Article Influence: 4.8] [Reference Citation Analysis (0)] |