Published online Mar 14, 2014. doi: 10.3748/wjg.v20.i10.2731
Revised: November 12, 2013
Accepted: January 6, 2014
Published online: March 14, 2014
Processing time: 164 Days and 21.4 Hours
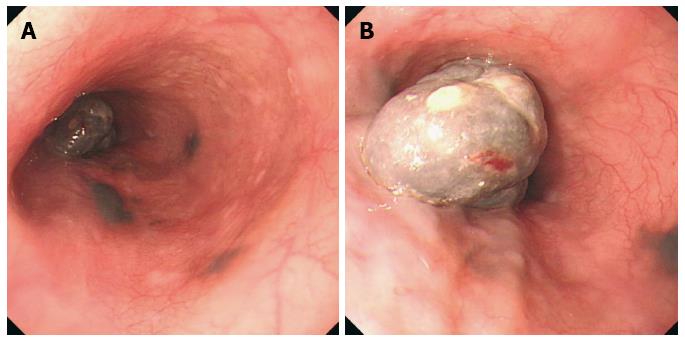
Primary malignant melanoma of the esophagus (PMME) is a malignant tumor which occurs in the melanin cells of esophageal mucosal epithelial basal layer. PMME is a rare disease with an extremely poor prognosis. PMME represents only 0.1% to 0.2% of all esophageal malignant tumors. Dysphagia, retrosternal or epigastric discomfort or pain is the most frequent symptom at presentation. Retrosternal, epigastric discomfort, melena or hematemesis are the major clinical manifestations. The tumor is often located from the middle to lower thoracic esophagus. The characteristic endoscopic finding of PMME is a polypoid lesion that is usually pigmented. Immunohistochemical examination with positive results of S100 protein, HMB45 and neuron-specific enolase allow a definitive diagnosis. PMME metastasizes via hematogenic and lymphatic pathways. Esophagectomy is believed to be an effective approach for localized PMME. Five-year survival rates of 37% or higher have been achieved recently. Herein, we report a case of an 65-year-old female admitted for progressive difficulty in swallowing for more than 4 mo. After upper gastrointestinal endoscopy and biopsy, upper gastrointestinal series and computed tomography examination, the patient accepted radical esophagectomy, and the postoperative pathologic and immunohistochemical examination showed PMME.
Core tip: We report a rare case of primary malignant melanoma of the esophagus (PMME). Although this disease is uncommon, a preoperative diagnosis of PMME is important. PMME cannot be definitely diagnosed from clinical symptoms or by X-ray barium meal examination but can be confirmed by endoscopic histological examination or a pathological report after surgical excision. The diagnosis of primary malignant melanoma should be suspected when a black or dark brown mass is observed during endoscopy. However, the endoscopic examination can complicate histological diagnosis due to poor sample quality. In the case presented here, we collected biopsies of the black surface, and the pathological report confirmed that the samples conformed to the characteristics of melanoma.
- Citation: Li YH, Li X, Zou XP. Primary malignant melanoma of the esophagus: A case report. World J Gastroenterol 2014; 20(10): 2731-2734
- URL: https://www.wjgnet.com/1007-9327/full/v20/i10/2731.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i10.2731
Primary malignant melanoma of the esophagus (PMME) is rare tumor, representing only 0.1% to 0.2% of all esophageal malignant tumors[1]. PMME often presents as polypoid lesion and usually causes dysphagia, retrosternal or epigastric discomfort or pain. With the development of the endoscopic technique, the discovery rate of PMME has gradually improved in recent years. However, prognosis is not optimistic due to the high metastatic potential of PMME. Similar to most malignant tumors, early detection and treatment of PMME can improve the five-year survival rates of patients. PMME postoperative five-year survival rates have risen from 4.2% in 1989 to 37% in 2002 and may be higher now, according to current reports[2,3]. In clinical practice upper gastrointestinal series and computed tomography (CT) are also widely used to diagnose and evaluate PMME. A definitive diagnosis could be confirmed with positive results of S100 protein, HMB45 and neuron-specific enolase from pathologic and immunohistochemical detection. We recently encountered a case of PMME in endoscopy and diagnosed it by pathologic and immunohistochemical examination.
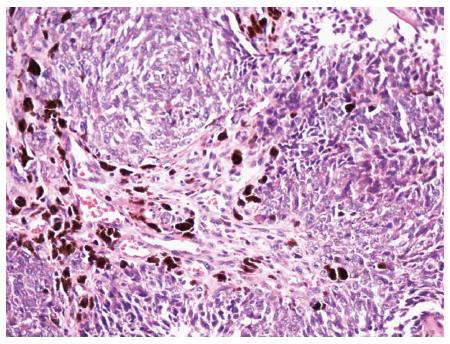
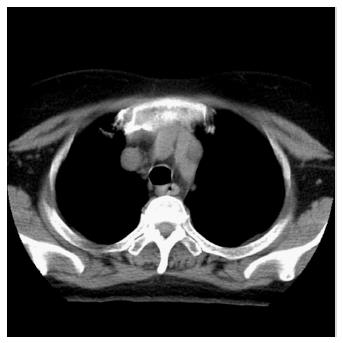
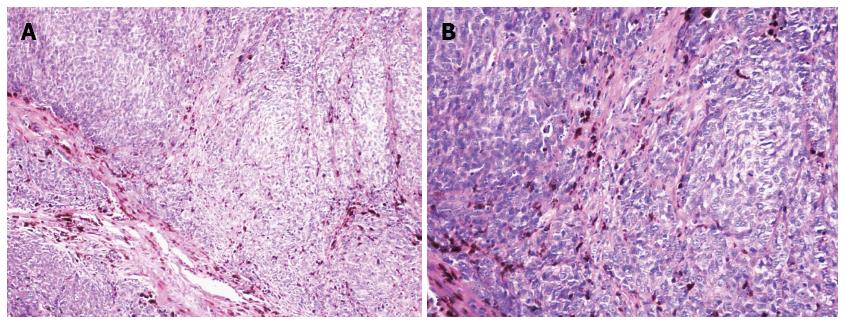
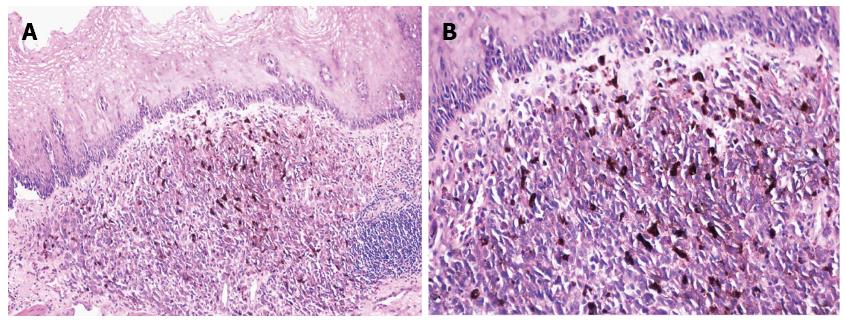
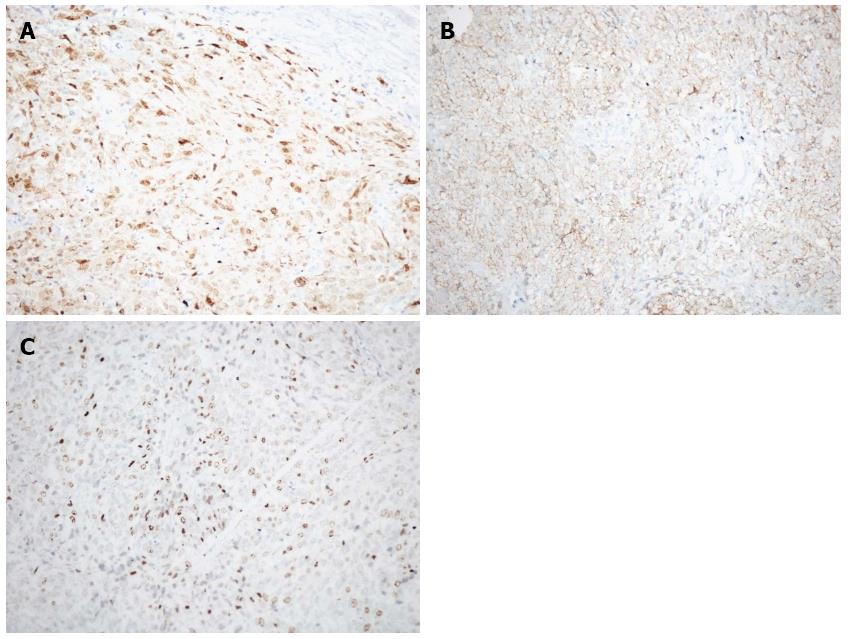
A 65-year-old woman with progressive difficulty in swallowing for more than 4 mo recently came to our institute for an examination. The dysphagia began 4 mo prior to the examination, especially when eating solid foods, and it became more serious 2 mo prior. Upper gastrointestinal endoscopy was performed and revealed a large tumor (2 cm × 4 cm) in the esophagus 33 cm from the incisors and 3 pigmented spots (satellites) adjacent to the large tumor 30-33 cm from the incisors (Figure 1A). The large tumor had a partial stalk and a black uneven surface, and the satellites had dark smooth surfaces (Figure 1B). Upon microscopic examination, the tumor was observed to contain variously pigmented unusual cells (Figure 2). An upper gastrointestinal series showed a circular filling defect in the lower esophagus (Figure 3). A plain CT scan of the cervical region, chest and upper abdomen showed thickness of the middle esophagus wall (Figure 4). The skin examination did not reveal any evidence of melanoma. Our diagnosis was primary malignant melanoma of the esophagus, and the patient underwent an esophagectomy. Postoperative specimens confirmed the diagnosis of primary melanoma, and the surgical margin of the esophagus was free from tumors (Figures 5 and 6). Immunohistochemical staining was positive for S100 (Figure 7A), HMB45 (Figure 7B), and Ki67 (Figure 7C). After the surgery, the patient’s dysphagia was significantly improved.
PMME cannot be definitely diagnosed from clinical symptoms or by X-ray barium meal examination. However, this disease can be confirmed by endoscopic histological examination or by pathology after surgical excision. An endoscopy may reveal friable pigmented polypoid masses that are rarely accompanied by ulcers[4]. The diagnosis of primary malignant melanoma should be suspected when a black or dark brown mass is observed during endoscopy. However, endoscopic examinations can sometimes complicate histological diagnoses when the sample is too small, no pigment granules are present or pigment granules can not be observed because of ulceration, erosion or necrosis. When these situations occur, PMME must be differentiated from low differentiated squamous carcinoma, sarcoma, carcinosarcoma, undifferentiated carcinoma and metastatic melanoma[1]. In addition, specific pathological staining and boundary changes around the tumor also contribute to the diagnosis[5]. Positive immunohistochemical staining results for the S100 protein, HMB45 and neuron-specific enolase aid in the diagnosis of melanoma[6]. A diagnosis can also be made by observing premelanosomes in the intracytoplasm through electron microscopy[1,7].
In conclusion, we have presented a rare case of primary malignant melanoma diagnosed by endoscopic biopsy of the esophagus. We propose that the effectiveness of diagnostic guidelines or treatment will increase with an increase in the number of PMME case reports.
Primary malignant melanoma of the esophagus (PMME) is a rare malignant disease with a poor prognosis and accounts for 0.1% to 0.2% of all esophageal malignant tumors.
This case involved PMME detected via endoscopic biopsy of the esophagus of a 65-year-old female. Dysphagia and retrosternal or epigastric discomfort or pain are the most frequent clinical symptoms.
This report summarized the characteristics of PMME, including the clinical manifestations, endoscopic features, clinical diagnosis, pathological diagnosis, treatment and prognosis
PMME is mainly located in the middle and lower esophagus, and the primary endoscopic manifestation is a polypoid lesion that is typically pigmented. Immunohistochemical assays positive for S100 protein, HMB45 and neuron-specific enolase could allow definitive diagnosis.
An esophagectomy is recommended for localized PMME. The five-year survival rate is almost 37%.
Gastrointestinal endoscopy and biopsy, upper gastrointestinal angiography and computed tomography examination, esophagectomy and the postoperative pathological and immunohistochemical examination contributed to the diagnosis of PMME in this case report.
This is a report about a primary melanoma of the esophagus. New standard procedures are missing e.g., endoscopic ultrasound and the discussion needs clinical updates.
P- Reviewers: Cao WB, Ding XW, Dormann AJ S- Editor: Gou SX L- Editor: A E- Editor: Wang CH
| 1. | Sabanathan S, Eng J, Pradhan GN. Primary malignant melanoma of the esophagus. Am J Gastroenterol. 1989;84:1475-1481. [PubMed] |
| 2. | Volpin E, Sauvanet A, Couvelard A, Belghiti J. Primary malignant melanoma of the esophagus: a case report and review of the literature. Dis Esophagus. 2002;15:244-249. [PubMed] |
| 3. | Gupta V, Kochhar R, Sinha SK, Das A. Primary malignant melanoma of the esophagus: long-term survival after radical resection. J Thorac Oncol. 2009;4:1180-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Iwanuma Y, Tomita N, Amano T, Isayama F, Tsurumaru M, Hayashi T, Kajiyama Y. Current status of primary malignant melanoma of the esophagus: clinical features, pathology, management and prognosis. J Gastroenterol. 2012;47:21-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Stranks GJ, Mathai JT, Rowe-Jones DC. Primary malignant melanoma of the oesophagus: case report and review of surgical pathology. Gut. 1991;32:828-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Joob AW, Haines GK, Kies MS, Shields TW. Primary malignant melanoma of the esophagus. Ann Thorac Surg. 1995;60:217-222. [PubMed] |
| 7. | Chalkiadakis G, Wihlm JM, Morand G, Weill-Bousson M, Witz JP. Primary malignant melanoma of the esophagus. Ann Thorac Surg. 1985;39:472-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 109] [Article Influence: 2.7] [Reference Citation Analysis (0)] |