Published online Jan 7, 2014. doi: 10.3748/wjg.v20.i1.323
Revised: September 15, 2013
Accepted: September 29, 2013
Published online: January 7, 2014
Processing time: 147 Days and 20.7 Hours
Endoscopic submucosal dissection (ESD) is now recognized as the preferred treatment modality for gastrointestinal epithelial lesions. A 21-month-old female was admitted with a giant hyperplastic polyp causing a gastric outlet obstruction. Successful ESD was performed with caution. The post-procedural course was uneventful without a bleeding episode. Although further study of the feasibility of ESD in early children is necessary, ESD could be applied to avoid laparotomy even in young children.
Core tip: We performed successful endoscopic submucosal dissection (ESD) for a giant hyperplastic polyp that obstructed the gastric outlet in a 21-month-old female patient. ESD could be applied to avoid surgery even in a young child. The present case is the youngest patient reported to date globally.
- Citation: Jung EY, Choi SO, Cho KB, Kim ES, Park KS, Hwang JB. Successful endoscopic submucosal dissection of a giant polyp in a 21-month-old female. World J Gastroenterol 2014; 20(1): 323-325
- URL: https://www.wjgnet.com/1007-9327/full/v20/i1/323.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i1.323
Endoscopic submucosal dissection (ESD) is now recognized as the preferred treatment modality for gastrointestinal epithelial lesions without lymph node metastasis. ESD achieves high rates of en bloc and complete resection with an acceptable range of complications such as bleeding and perforation. However, most ESD results have been obtained in adults, and ESD in children is rare. Here, a 21-month-old female with a giant hyperplastic polyp causing a gastric outlet obstruction was treated successfully by ESD.
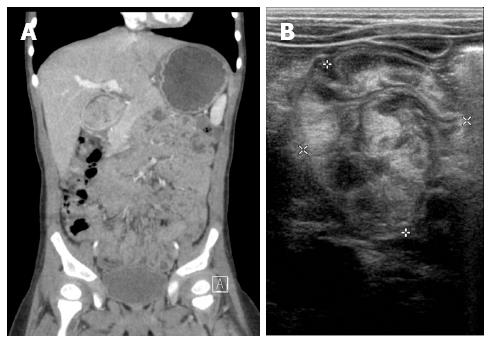
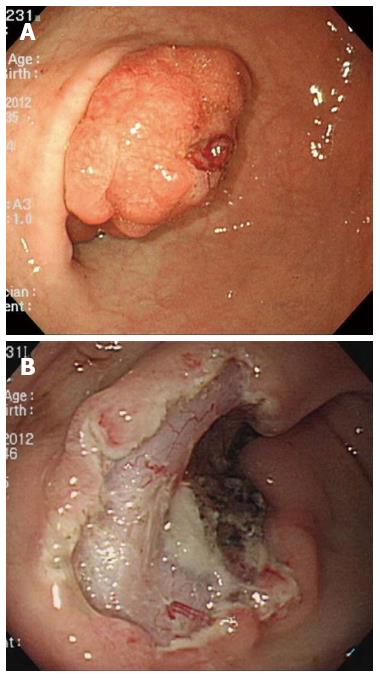
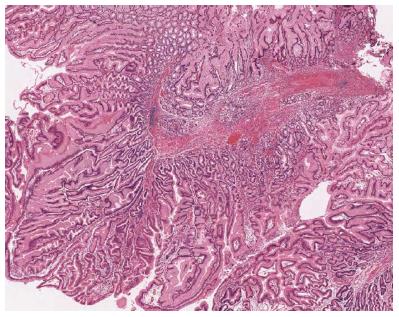
A 21-month-old female (11 kg, 85 cm), who had no remarkable medical or family history, was admitted with vomiting, abdominal distension, and epigastric pain. Ultrasonography and computed tomography with intravenous contrast showed a large, nodular soft tissue mass occupying the pylorus and duodenum with a markedly distended stomach (Figure 1). A broad-based giant sessile polyp was located on the anterior wall of the distal antrum with extended into the duodenum on esophagogastroduodenoscopy (Figure 2A). The giant polyp had a cauliflower-like appearance and easily slid down into the duodenum. An endoscopic biopsy showed a hyperplastic polyp. An upper gastrointestinal series with double contrast showed a lobulating giant mass causing gastric outlet obstruction. The mass was endoscopically removed under general anesthesia using ESD in a 2.5-h procedure using a ClearCut knife (I-type, FINEMEDIX Co., Daegu, South Korea) and a Hook knife (Olympus Co., Tokyo, Japan). The procedure started with an injection of lifting solution into the submucosal layer, followed by an endoscopic circumferential incision, and dissection from the lateral edges, working through the lifted submucosal layer until the lesion was resected in one piece (Figure 2B)[1]. The polyp was retrieved by segmentation because it was too large to remove as one piece (Figure 3). A pathological examination showed hyperplastic polyps with thick-walled vessels and organized thick bundles of arborizing smooth muscle with a prominent basal glandular component (Figure 4). The post-procedural course was uneventful without a bleeding episode. The patient was discharged at day 6 after the procedure and is doing well 4 mo after discharge with no further symptoms.
The prevalence of gastric polyps in the pediatric population is low compared with that in adults (0.7% vs 6.35%)[2,3]. The most common pathological types in children are hyperplastic polyps, and most are asymptomatic and do not require removal. However, symptoms such as abdominal pain, heartburn, dyspepsia, and/or upper gastrointestinal bleeding may occur[4]. It is rare for these polyps to cause gastric outlet obstruction. However, once they occur, they must be removed. Few case reports of management of hyperplastic polyps causing gastric outlet obstruction in a pediatric patient are available. Surgical laparotomy enables removal of a pedunculated or giant polyp in infants[5,6]. Endoscopic procedures such as snare polypectomy[7] or endoscopic mucosal resection (EMR)[8] could also be considered as treatment options. However, in pediatric patients, removing giant polyps using endoscopy is challenging because any bleeding from the large feeding vessels could induce unexpected hypovolemic shock. In particular, if the patient is a young toddler, as in this case, < 50 mL of bleeding (minor bleeding in an adult) might cause hypovolemic shock.
ESD is an option that may avoid the problems associated with EMR. ESD can be used for larger lesions regardless of their location. Although ESD techniques require a higher level of skill, ESD may assist bleeding control by means of careful submucosal dissection avoiding improper vessel cutting and applying appropriate coagulation under direct vision. A successful ESD in a 11-year-old male has been reported, which is the youngest case in the previous literature[9]. However, the present case is, to our knowledge, the youngest patient reported to date globally. We used ESD rather than conventional EMR or laparotomy even though ESD is technically difficult to perform in a young child. Maintaining the airway, keeping the child motionless, and careful dissection of the submucosal layer with vessels are important aspects of the endoscopic procedure if a grave situation is to be avoided in a very young patient.
In conclusion, we performed successful ESD for a cauliflower-like giant hyperplastic polyp that obstructed the gastric outlet in a 21-month-old female patient. ESD was applied to avoid surgery even in the young child, although further investigation of the feasibility of ESD in young children and careful follow-up for recurrence is needed.
P- Reviewers: Canbaz H, Jeon SW S- Editor: Wen LL L- Editor: Cant MR E- Editor: Ma S
| 1. | Cho KB, Jeon WJ, Kim JJ. Worldwide experiences of endoscopic submucosal dissection: not just Eastern acrobatics. World J Gastroenterol. 2011;17:2611-2617. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 23] [Cited by in RCA: 29] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Attard TM, Yardley JH, Cuffari C. Gastric polyps in pediatrics: an 18-year hospital-based analysis. Am J Gastroenterol. 2002;97:298-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Carmack SW, Genta RM, Schuler CM, Saboorian MH. The current spectrum of gastric polyps: a 1-year national study of over 120,000 patients. Am J Gastroenterol. 2009;104:1524-1532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 199] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 4. | Jain R, Chetty R. Gastric hyperplastic polyps: a review. Dig Dis Sci. 2009;54:1839-1846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 5. | Sanna CM, Loriga P, Dessi E, Frau G, Congiu G, Corrias A, Corda R. Hyperplastic polyp of the stomach simulating hypertrophic pyloric stenosis. J Pediatr Gastroenterol Nutr. 1991;13:204-208. [PubMed] |
| 6. | Brooks GS, Frost ES, Wesselhoeft C. Prolapsed hyperplastic gastric polyp causing gastric outlet obstruction, hypergastrinemia, and hematemesis in an infant. J Pediatr Surg. 1992;27:1537-1538. [PubMed] |
| 7. | Parikh M, Kelley B, Rendon G, Abraham B. Intermittent gastric outlet obstruction caused by a prolapsing antral gastric polyp. World J Gastrointest Oncol. 2010;2:242-246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 13] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Pontone S, Pironi D, Eberspacher C, Pontone P, Filippini A. Endoscopic management of multiple large antral hyperplastic polyps causing gastric outlet obstruction. Ann Ital Chir. 2011;82:297-300. [PubMed] |
| 9. | Otake K, Uchida K, Inoue M, Matsushita K, Hashimoto K, Toiyama Y, Tanaka K, Nakatani K, Kawai K, Kusunoki M. A large, solitary, semipedunculated gastric polyp in pediatric juvenile polyposis syndrome. Gastrointest Endosc. 2011;73:1313-1314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |