Published online Feb 7, 2013. doi: 10.3748/wjg.v19.i5.773
Revised: October 25, 2012
Accepted: November 6, 2012
Published online: February 7, 2013
Processing time: 125 Days and 9.9 Hours
Increased ischemic stroke risk is observed in patients with inflammatory bowel disease (IBD). Causes and physiopathological aspects of cerebral infarct, in this specific population, are less often described. There is little information to provide guidelines for the best curative and preventive treatment. We report 2 cases of ischemic strokes due to internal carotid thrombus in patients during active phase of IBD. Ulceration of early atherosclerotic plaques activated by a hypercoagulation state may cause a thrombus. A combined therapy with heparin and corticosteroids was used for both our patients. Lysis of the thrombus was obtained after several days without surgical treatment and shown by ultrasonography. These cases highlight an aetiology of stroke in patients with IBD and use of a synergic treatment to respond to hypercoagulability in link with IBD. Benefits and safety of this therapy should be confirmed with clinical studies.
- Citation: Richard S, Mione G, Perrin J, Toussaint-Hacquard M, Lacour JC, Ducrocq X. Internal carotid thrombus in patients with inflammatory bowel disease: Two cases. World J Gastroenterol 2013; 19(5): 773-775
- URL: https://www.wjgnet.com/1007-9327/full/v19/i5/773.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i5.773
Patients with inflammatory bowel diseases (IBD) have a higher risk of arterial cerebral infarction even if they are young with few cardio-vascular risk factors[1]. Causes and physiopathological aspects are less known. We describe 2 cases of IBD patients who presented ischemic strokes due to homolateral internal carotid thrombus.
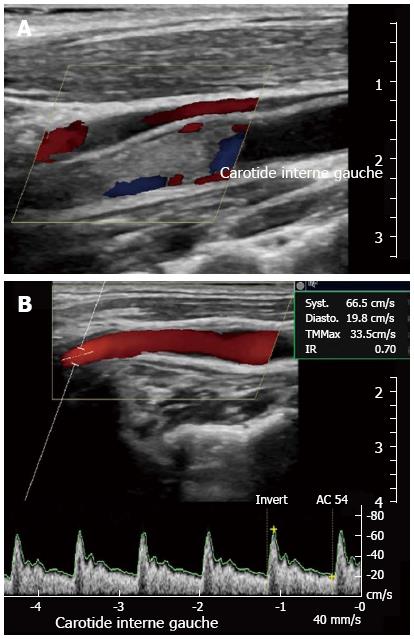
A 32 year-old man, with Crohn’s disease (CD) without immunosuppressive treatment for several years, was admitted for sudden right hemiplegia. He was a light smoker without any other vascular risk factor like hypertension, dyslipidemia, diabetes, and had no family history of vascular disease. At admission the National Institute of Health Stroke Scale (NIHSS) was 13, and blood pressure was 110/70 mm Hg. Brain magnetic resonance imaging (MRI) revealed ischemic stroke with thrombosis of the initial part of the left middle cerebral artery (MCA). Intravenous thrombolysis with plasminogen tissue activator was administered. Cervical ultrasonography (US) revealed occlusion of the left internal carotid artery (Figure 1A), due to a thrombus, confirmed by computed tomography (CT) angiography. Blood tests were performed: the platelet count was 342 G/L, hyperhomocysteinemia 137 μmol/L; C-reactive protein (CRP) 15.4 mg/L; low-density lipoprotein (LDL)-cholesterol 0.87g/L; preprandial blood glucose level 1.01g/L, and the erythrocyte sedimentation rate (ESR) was elevated at 40 mm. Digestive endoscopy found signs of active CD. Unfractionated heparin and corticosteroid treatment (prednisolone 0.5 mg/kg per day) were initiated and 15 d later, there was total resorption of the thrombus, apart from a tiny plaque as controlled by cervical US (Figure 1B) and CT angiography. One month later, the NIHSS was 6, an overlap treatment of vitamin K antagonist was initiated and the patient was transferred to a rehabilitation center with a daily dose of prednisolone and folic acid. Proctectomy with terminal ileostomy was performed 4 mo later.
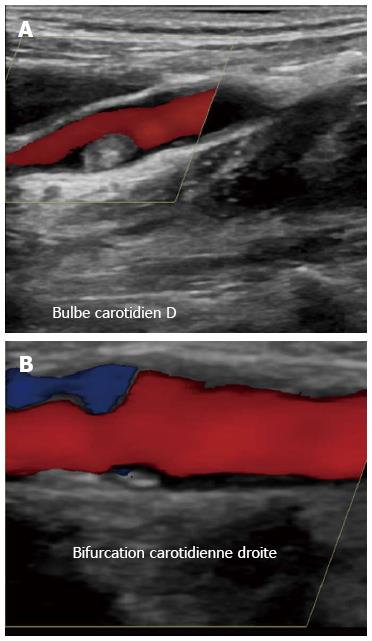
A non-smoker 42 year-old woman with ulcerative colitis diagnosed 3 years previously and treated with corticosteroids and mesalazine, was hospitalised for sudden right hemiplegia. She had no personal medical history of diabetes, hypertension and dyslipidemia and no family history of vascular disease. She had already presented several ischemic strokes, revealing intra-cardiac thrombus, but had refused any oral anticoagulant treatment. At admission, the NIHSS was 19 and blood pressure was 120/80 mmHg. A brain MRI showed a recent ischemic stroke with occlusion of the origin of the right MCA. Cerebral angiography with thrombectomy was performed and complicated by hemorrhagic transformation of the cerebral infarct. Severe bloody diarrhoea was controlled by a high dose of corticosteroids (methylprednisolone 1 mg/kg for 10 d before progressive decrease). Cervical US showed a thrombus in the right internal carotid (Figure 2A). There were biological signs of inflammation with an elevated ESR at 64 mm and CRP at 14.4 mg/L, slight hyperhomocysteinemia (17.9 μmol/L), a low level of LDL-cholesterol at 0.80 g/L, a normal preprandial blood glucose level at 0.90 g/L, and a platelet count of 462 G/L. Ten days later, after partial resorption of cerebral haemorrhage, low molecular weight heparin (LWMH), enoxaparine, was introduced at a dose of 100 UI/kg twice a day. After one week of treatment, cervical US revealed regression of the thrombus with only a tiny plaque on the right internal carotid wall (Figure 2B). LWMH was switched for aspirin as the patient rejected any oral anticoagulant. She was finally transferred to a rehabilitation center with a NIHSS of 6.
These observations suggest that 2 factors can contribute to carotid thrombus: abnormalities of the coagulation system and disease of arterial wall[2].
Hypercoagulability is almost always observed during the active phase of IBD and can lead to an arterial or intracardiac thrombus, as described in the second case. Elevated platelets (with hyperactivation), fibrinogen, factor V, VIII, plasminogen activator inhibitor and decreased antithrombin and tissue plasminogen activator have been described. Vitamin K malabsorption causes not only short partial thromboplastin times but also protein C and S deficiency[3]. There may also be a higher prevalence of antiphospholipid antibodies in IBD patients[4]. Common carotid artery intima-media thickness is significantly higher in IBD patients compared with controls with a significant association with homocysteine levels and age[5]. This is due to modifications of the vessel-wall induced by chronic inflammation: cytokines activate endothelium with conversion to a pro-inflammatory thrombogenic phenotype and increased von Willebrand factor[6]. Accelerated atherosclerosis is found in systemic inflammatory disorders[7], and atherosclerotic plaques were found after resorption of carotid thrombus in both the cases described here, as well as in a similar case described by Lafitte et al[8]. In IBD patients, an inflammatory state may also lead to endothelial damage and early atherosclerotic lesions. In the cases we describe, the formation of carotid thrombus may have been due to ulceration of plaques which have activated a pro-thrombotic coagulation state. For both our patients, lysis of the thrombus was obtained after several days of heparin treatment with double impact: fibrinolysis and the still debated anti-inflammatory action[9]. Nevertheless, this approach has only been described in a few cases and should be evaluated with clinical studies, especially as it may provoke mucosal[10] and cerebral bleeding in case of extensive stroke. We also administered corticosteroids to both our patients to decrease the inflammation, hypercoagulation state, to promote mucosal regeneration and then, to potentiate the benefits of heparin.
Internal carotid thrombus is a cause of ischemic stroke in IBD patients, and is a consequence of the combination of early atherosclerotic lesions and hypercoagulation state. Combining heparin and anti-inflammatory therapy may be considered as a synergic treatment but, further work is required to establish efficacy and safety.
P- Reviewer Mowat C S- Editor Song XX L- Editor A E- Editor Zhang DN
| 1. | Andersohn F, Waring M, Garbe E. Risk of ischemic stroke in patients with Crohn’s disease: a population-based nested case-control study. Inflamm Bowel Dis. 2010;16:1387-1392. [PubMed] |
| 2. | Yoshida H, Granger DN. Inflammatory bowel disease: a paradigm for the link between coagulation and inflammation. Inflamm Bowel Dis. 2009;15:1245-1255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 128] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 3. | Conlan MG, Haire WD, Burnett DA. Prothrombotic abnormalities in inflammatory bowel disease. Dig Dis Sci. 1989;34:1089-1093. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Twig G, Zandman-Goddard G, Szyper-Kravitz M, Shoenfeld Y. Systemic thromboembolism in inflammatory bowel disease: mechanisms and clinical applications. Ann N Y Acad Sci. 2005;1051:166-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 62] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Papa A, Santoliquido A, Danese S, Covino M, Di Campli C, Urgesi R, Grillo A, Guglielmo S, Tondi P, Guidi L. Increased carotid intima-media thickness in patients with inflammatory bowel disease. Aliment Pharmacol Ther. 2005;22:839-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 72] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 6. | Nachman RL, Silverstein R. Hypercoagulable states. Ann Intern Med. 1993;119:819-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 37] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Kayahan H, Sari I, Cullu N, Yuksel F, Demir S, Akarsu M, Goktay Y, Unsal B, Akpinar H. Evaluation of early atherosclerosis in patients with inflammatory bowel disease. Dig Dis Sci. 2012;57:2137-2143. [PubMed] |
| 8. | Lafitte M, Debruxelles S, Sibon I, Rouanet F, Couffinhal T. Cerebral embolism from subclinical carotid atherosclerotic lesion in a young woman with inflammatory Crohn disease. Eur Heart J. 2009;30:575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Chande N, MacDonald JK, Wang JJ, McDonald JW. Unfractionated or low molecular weight heparin for induction of remission in ulcerative colitis: a Cochrane inflammatory bowel disease and functional bowel disorders systematic review of randomized trials. Inflamm Bowel Dis. 2011;17:1979-1986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Nogami H, Iiai T, Maruyama S, Tani T, Hatakeyama K. Common carotid arterial thrombosis associated with ulcerative colitis. World J Gastroenterol. 2007;13:1755-1757. [PubMed] |