Published online Dec 7, 2013. doi: 10.3748/wjg.v19.i45.8445
Revised: June 6, 2013
Accepted: June 18, 2013
Published online: December 7, 2013
Processing time: 264 Days and 20.8 Hours
Gastric duplication cyst is a very rare gastrointestinal tract malformation that accounts for 2%-4% of alimentary tract duplications. Most cases are diagnosed within the first year of life, following presentation of abdominal pain, vomiting, and weight loss and clinical discovery of an abdominal palpable mass. This case report describes a very uncommon symptomatic gastric duplication cyst diagnosed for the first time in adulthood. Only a few other case reports of similar condition exist, and all were identified by endosonography. The current case involves a 52-year-old male who presented with a one-month history of progressive iron deficiency anemia without overt gastrointestinal bleeding. The patient underwent esophagogastroduodenoscopy, which revealed a 2.0 cm pinkish subepithelial lesion, suspected to be a gastrointestinal stromal tumor (GIST) and source of gastrointestinal bleeding. The endosonography showed inhomogeneous hypoechoic lesions with focal anechoic areas arising from a second and third layer of the gastric wall. Differential diagnoses of GIST, neuroendocrine tumor, or pancreatic heterotopia were made. The lesion was removed using an endoscopic submucosal resection technique. Histopathology revealed an erosive gastric mass composed of a complex structure of dilated gastric glands surrounded by fibro-muscular tissue, fibroblasts, and smooth muscle bundles, which led to the diagnosis of gastric duplication.
Core tip: Gastric duplication cyst is a very rare gastrointestinal malformation and most of the cases are diagnosed within the first year of life following clinical investigations of abdominal symptoms including pain, vomiting, and palpable mass. Gastrointestinal hemorrhage is a rare clinical manifestation. Here, we report a 52-year-old man who presented with a one-month history of progressive iron deficiency anemia without overt gastrointestinal bleeding. Esophagogastroduodenoscopy revealed general gastrointestinal bleeding and a 2.0 cm subepithelial tumor originating from the third layer of gastric wall. After complete removal by endoscopic mucosal resection, histopathological findings indicated a diagnosis of gastric duplication cyst with erosion.
- Citation: Deesomsak M, Aswakul P, Junyangdikul P, Prachayakul V. Rare adult gastric duplication cyst mimicking a gastrointestinal stromal tumor. World J Gastroenterol 2013; 19(45): 8445-8448
- URL: https://www.wjgnet.com/1007-9327/full/v19/i45/8445.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i45.8445
Gastric duplication cyst is a rare congenital malformation of the upper gastrointestinal tract, accounting for 2%-4% of all duplications of the alimentary tract[1]. Most cases are diagnosed in the first year of life, following presentation of abdominal pain, vomiting, and weight loss and clinical discovery of an abdominal palpable mass or upon clinical investigation of gastrointestinal obstruction and/or perforation[1-3]. Bleeding was a very rare clinical manifestation of this condition, and very few cases of gastric duplication cysts have been diagnosed in adulthood[2-6]. Some of the adult cases have been incidentally detected during upper endoscopy [endoscopic ultrasound (EUS) technology] or abdominal imaging studies for other reasons[3,5,6]. Yet, the reported radiographic and endosonographic findings from these limited cases have not revealed any characteristic profile useful for diagnosis.
Herein we describe an unusual case of gastric duplication cyst which was identified in an adult male following endosonographic investigations of subacute anemia and discovery of upper gastrointestinal bleeding.
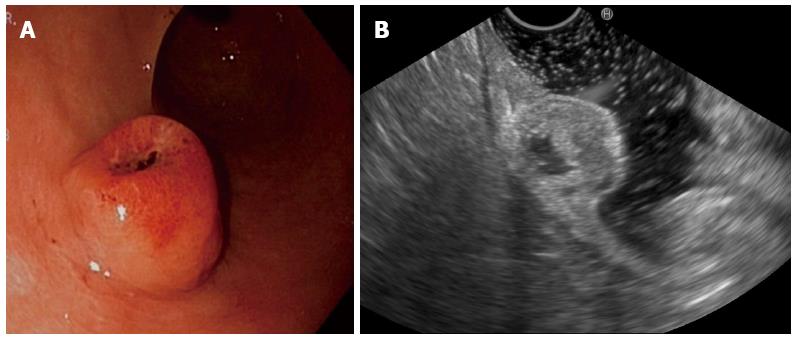
A 52-year-old man presented with a one-month history of progressive iron deficiency anemia without overt gastrointestinal bleeding. Laboratory tests indicated remarkably low hemoglobin level (9.0 mg/dL; reference range: 13.0-17.0 mg/dL) and slightly low ferritin level (18.0 ng/mL; reference range: 12-200 ng/mL). Esophagogastroduodenoscopy was performed and revealed a 2.0 cm pinkish umbilicated subepithelial lesion located at antrum and accompanied by evidence of ulceration and blood clotting (Figure 1A). Gastrointestinal stromal tumor (GIST) was suspected, and subsequent endosonographic evaluation was ordered.
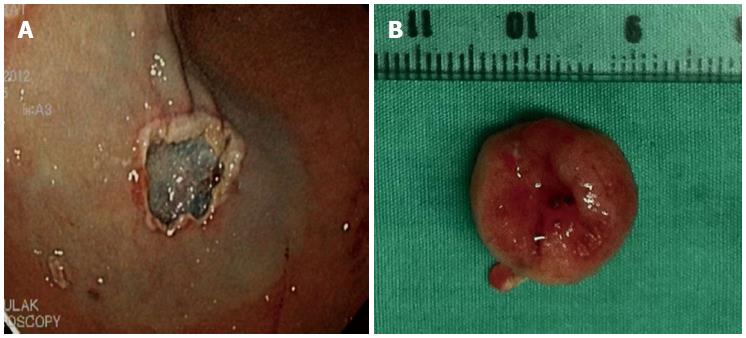
In the endoscopic suite, the patient underwent total intravenous anesthesia using propofol with full anesthetic monitoring. A curvilinear echoscope (EG-3870UTK; Pentax, Miyaki, Japan) was used and revealed a 1.8 cm hypoechoic mass arising from the second and third layer of the gastric wall, with a centralized anechoic area lacking vascular flow (Figure 1B). The findings suggested small GIST with cystic change. An endoscopic submucosal resection (EMR) technique was applied with an 8.8 mm gastroscope (GIF-Q180; Olympus, Tokyo, Japan) and creation of a submucosal cushion by injecting a 4 mL mixture of adrenaline (1 mg), Indigo carmine (0.4% solution) and Gelofucin® (500 mL) using a 23 gauge needle [Heyinovo™; Wilson Instruments Co., Ltd., Shanghai, China]. The lesion was removed in an en-bloc fashion by an electrical snare (Figure 2).
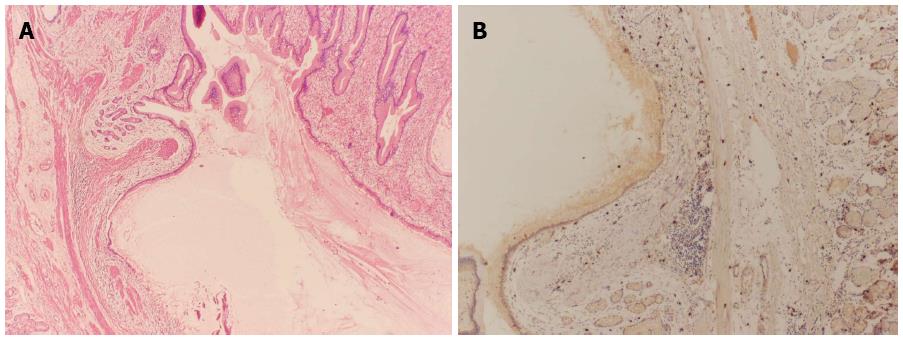
Histopathological analysis of the resected tissue revealed an erosive gastric mass that was composed of a complex structure characterized by dilated gastric glands surrounded by fibromuscular tissue, fibroblasts, and smooth muscle bundles. Immunohistochemistry analysis showed negativity for CD117, DOG-1, and S-100, but focal positivity for smooth muscle actin. Although these pathology findings suggested a differential diagnosis of pancreatic heterotopia, no evidence was found for this diagnosis (Figure 3) and the diagnosis of gastric duplication was made.
Gastric duplication cysts are rare congenital malformations with frequent localization in the alimentary tract that follows the incidence hierarchy of ileum > esophagus > jejunum > colon > stomach > appendix[2-4]. Yet, the etiopathogenetic origin of gastric duplication cysts remains undefined. These duplications, however, are usually found to be distributed dorsally to the primitive gut during development, so that most gastric duplication cysts appear along the greater curvature of the stomach, adjacent to the gastric wall (only 5.5% are found in the lesser curvature[3]). The stomach is lined by typical gastric mucosa, which is often accompanied by patches of ectopic intestinal epithelium; in addition, a smooth muscle coat fuses with the muscularis propria of the stomach, making it contiguous with the wall of the stomach, and shares a common blood supply. The cyst in the current case was located at the greater curvature of the antral area.
The rarity of the current case was furthered by the manifestation of symptoms and diagnosis having occurred in later adulthood. Furthermore, gastric duplication cysts are usually asymptomatic in adult patients, yet this case presented with anemia from upper gastrointestinal bleeding. Based upon the pathological findings, we speculate that acid erosion of the gastric lining near the cyst led to the hemorrhage, as well as the observed ulceration.
Throughout the case management course, various differential diagnoses were suggested and rejected. In particular, the endoscopic and EUS findings of small subepithelial lesions with umbilication suggested potential diagnoses of GIST, neuroendocrine tumor, or pancreatic heterotopia. The endosonographic characteristics of this patient are very distinctive from those reported for previous cases, even though all cases involved cystic lesions at greater curvature sites of the stomach. The cysts of previous cases have ranged in diameter from 5 to 7 cm, and were located adjacent to the fourth layer of the gastric wall. In addition, most of these cysts showed an inhomogeneous echoic pattern, which was suspected to reflect secretions from the gastric gland composed of both mucous and serous material[3,5,6]. We hypothesized the atypical endosonographic findings of the current case corresponded to the smaller cyst size and low fluid volume, which caused the lesion to appear more like a solid mass with cystic degeneration than a cystic lesion. Therefore, the final diagnosis was gastric duplication cyst. Finally, even though fine needle aspiration cytology may have been able to achieve the differential diagnosis[4], we felt that complete removal of the lesion was justified by the patient’s symptoms and unknown risk for malignant transformation[1].
P- Reviewers: Basu S, Braat H, Tomizawa M S- Editor: Wen LL L- Editor: A E- Editor: Ma S
| 1. | Pokorny CS, Cook WJ, Dilley A. Gastric duplication: endoscopic appearance and clinical features. J Gastroenterol Hepatol. 1997;12:719-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Hlouschek V, Domagk D, Naehrig J, Siewert JR, Domschke W. Gastric duplication cyst: a rare endosonographic finding in an adult. Scand J Gastroenterol. 2005;40:1129-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Takahara T, Torigoe T, Haga H, Yoshida H, Takeshima S, Sano S, Ishii Y, Furuya T, Nakamura E, Ishikawa M. Gastric duplication cyst: evaluation by endoscopic ultrasonography and magnetic resonance imaging. J Gastroenterol. 1996;31:420-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Blinder G, Hiller N, Adler SN. A double stomach in an adult. Am J Gastroenterol. 1999;94:1100-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Seijo Ríos S, Lariño Noia J, Abdulkader Nallib I, Lozano León A, Vieites Pérez-Quintela B, Iglesias García J, Domínguez Muñoz JE. [Adult gastric duplication cyst: diagnosis by endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA)]. Rev Esp Enferm Dig. 2008;100:586-590. [PubMed] |
| 6. | Napolitano V, Pezzullo AM, Zeppa P, Schettino P, D’Armiento M, Palazzo A, Della Pietra C, Napolitano S, Conzo G. Foregut duplication of the stomach diagnosed by endoscopic ultrasound guided fine-needle aspiration cytology: case report and literature review. World J Surg Oncol. 2013;11:33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |