Published online Sep 28, 2013. doi: 10.3748/wjg.v19.i36.6125
Revised: April 26, 2013
Accepted: May 17, 2013
Published online: September 28, 2013
Processing time: 260 Days and 8.1 Hours
A 77-year-old woman complained of epigastralgia, and a tumor (5 cm in diameter) of the gallbladder neck was detected by image analysis. Following cholecystectomy, the tumor was pathologically diagnosed as intraductal papillary neoplasm (IPN), gastric type, with associated invasive carcinoma. About 10 mo later, intraluminal multiple masses (3 foci, up to 1.8 cm) were noted in the extrahepatic bile duct, and the resected specimen showed that all tumors had similar gross and microscopic features as seen in gallbladder IPN without invasion, and they were synchronous multiple lesions. This case showed a papillary tumor of the gallbladder of gastric phenotype, and confirmed that the gallbladder is a target of IPN in addition to the bile ducts.
Core tip: Recently, the papillary or tumoral neoplastic lesions within the lumen of the biliary tree including the gallbladder, papilla of Vater, and pancreatic duct have been proposed collectively as a preinvasive neoplastic lesion. The patient reported here was an interesting case of intraluminal papillary neoplasm involving the gallbladder and metachronously the extrahepatic bile duct. This letter to the editor encourages clinicians to detect more of such neoplastic lesions.
- Citation: Sato H, Sato Y, Harada K, Sasaki M, Hirano K, Nakanuma Y. Metachronous intracystic and intraductal papillary neoplasms of the biliary tree. World J Gastroenterol 2013; 19(36): 6125-6126
- URL: https://www.wjgnet.com/1007-9327/full/v19/i36/6125.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i36.6125
The World Health Organization (WHO) Classification of Tumours of the Digestive System (2010) recognizes intraductal papillary neoplasms of the bile duct (IPNBs) as a precancerous entity of cholangiocarcinoma[1,2]. Before the recognition by WHO, this entity was called by various and many different names, such as biliary papilloma and papillomatosis, and papillary adenocarcinoma[2-4]. IPNBs are occasionally multicentric along the intrahepatic and extrahepatic bile duct, synchronously and metachronously.
Interestingly, IPNB shares many features with intraductal papillary mucinous neoplasms of the pancreas (IPMN-Ps). For example, four phenotypes of epithelium are recognized in IPNB as well as IPMN-P[1,5,6]: pancreatobiliary, intestinal, oncocytic, and gastric types. Intracystic papillary neoplasm (IPN) of the gallbladder was newly described in addition to papillary adenomas in the 2010 WHO classification.
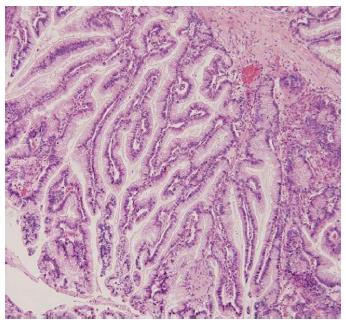
We have recently experienced a case of IPN of the gallbladder followed by metachronous IPNBs of the extrahepatic bile duct. A 77-year old woman complained of epigastralgia, and a tumor of the gallbladder neck was detected by computed tomography (CT) and magnetic resonance imaging (MRI). By cholecystectomy, a papillary, cauliflower-like tumor (5 cm × 4.8 cm) growing intraluminally was found at the gallbladder neck, and the remaining gallbladder was distended. Most of the tumor showed a well-differentiated papillary neoplasm composed of columnar epithelium with supranuclear mucin, resembling gastric mucosa, particularly gastric foveola, covering fine vasculo-fibrous cores (Figure 1), and showed moderate- to high-grade intraepithelial neoplasia. There was focal invasion of moderately differentiated tubular adenocarcinoma in the gallbladder wall. There was no metastasis, and the gallbladder mucosa, except for the tumor, did not show dysplastic or metaplastic changes. The tumor was diagnosed as IPN of the gallbladder with associated invasive carcinoma.
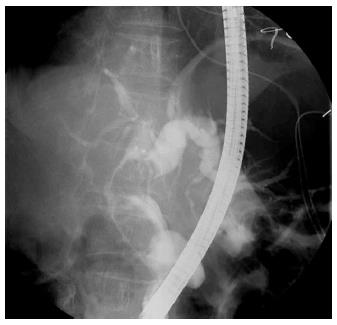
About 10 mo later, intraluminal multiple masses of the extrahepatic bile duct and secondary dilatation of the intra/extrahepatic bile ducts were demonstrated by CT, MRI and endoscopic retrograde cholangiography (Figure 2). The affected extrahepatic bile duct was surgically resected. The resected bile duct was dilated and filled with three separate brown papillary masses (1.8 cm × 1.4 cm, 1.5 cm × 1.5 cm, and 1.2 cm × 1.1 cm). There was no mucin within the resected bile ducts. These extrahepatic tumors commonly showed similar gross and microscopic features as seen in gallbladder IPN, but no invasion. There were no significant pathological changes in the background of the extrahepatic bile ducts. There was no continuity between the three lesions and they were regarded as synchronous multiple lesions.
Immunohistochemically, MUC5AC and MUC6 were diffusely positive, whereas MUC2-positive cells were scattered in these IPNs, and MUC1 was not observed in any of the four IPNs of the gallbladder and bile ducts. These IPNs were regarded as gastric type.
Similar to IPNB, IPN of the gallbladder may present with a pancreatobiliary or intestinal phenotype[2,3]. Distinguishing IPN from papillary adenomas of the gallbladder may be controversial. The vast majority of IPNs of the gallbladder have a biliary phenotype, whereas papillary adenomas exhibit an intestinal or gastric phenotype. This case showed a papillary tumor of the gallbladder of gastric phenotype, and confirmed that the gallbladder is a target of IPN in addition to the bile ducts.
P- Reviewer Han X S- Editor Huang XZ L- Editor Kerr C E- Editor Zhang DN
| 1. | Zen Y, Fujii T, Itatsu K, Nakamura K, Minato H, Kasashima S, Kurumaya H, Katayanagi K, Kawashima A, Masuda S. Biliary papillary tumors share pathological features with intraductal papillary mucinous neoplasm of the pancreas. Hepatology. 2006;44:1333-1343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 283] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 2. | Nakanuma Y, Curado MP, Franceschi S, Gores G, Paradis V, Sripa B, Tsui WMS, Wee A. Intrahepatic cholagniocarcinoma. World Classification of Tumours of the Digestive System. Lyon: IARC 2010; 217-224. |
| 3. | Albores-Saavedra J, Adsay NV, Crawfor JM, Klimstra DS, Kloppel G, Sripa B, Tsui WMS, Paradis V. Carcinoma of the gallbladder and extrahepatic bile duct. World Classification of Tumours of the Digestive System. Lyon: IARC 2010; 266-273. |
| 4. | Kim YS, Myung SJ, Kim SY, Kim HJ, Kim JS, Park ET, Lim BC, Seo DW, Lee SK, Kim MH. Biliary papillomatosis: clinical, cholangiographic and cholangioscopic findings. Endoscopy. 1998;30:763-767. [PubMed] |
| 5. | Chen TC, Nakanuma Y, Zen Y, Chen MF, Jan YY, Yeh TS, Chiu CT, Kuo TT, Kamiya J, Oda K. Intraductal papillary neoplasia of the liver associated with hepatolithiasis. Hepatology. 2001;34:651-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 191] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 6. | Naito Y, Kusano H, Nakashima O, Sadashima E, Hattori S, Taira T, Kawahara A, Okabe Y, Shimamatsu K, Taguchi J. Intraductal neoplasm of the intrahepatic bile duct: clinicopathological study of 24 cases. World J Gastroenterol. 2012;18:3673-3680. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |