Published online Sep 28, 2013. doi: 10.3748/wjg.v19.i36.6122
Revised: May 21, 2013
Accepted: August 16, 2013
Published online: September 28, 2013
Processing time: 156 Days and 23 Hours
Biliary ascariasis is a common problem in rural areas in China. The common presentations include biliary colic, acute cholangitis, obstructive jaundice, choledocholithiasis and acute cholecystitis. Here, we describe a case with biliary ascariasis two days after endoscopic sphincterotomy for choledocholithiasis. A living ascaris was successfully removed by endoscopic retrograde cholangiopancreatography. This case indicated that biliary ascariasis is not an uncommon complication of endoscopic sphincterotomy in some regions where ascariasis is epidemic.
Core tip: Biliary ascariasis is a common problem in rural areas in China. The common presentations include biliary colic, acute cholangitis, obstructive jaundice, choledocholithiasis and acute cholecystitis. Here, we describe a case with biliary ascariasis two days after endoscopic sphincterotomy for choledocholithiasis. A living ascaris was successfully removed by endoscopic retrograde cholangiopancreatography. This case indicated that biliary ascariasis is not an uncommon complication of endoscopic sphincterotomy in some regions where ascariasis is epidemic.
- Citation: Wang J, Pan YL, Xie Y, Wu KC, Guo XG. Biliary ascariasis in a bile duct stones-removed female patient. World J Gastroenterol 2013; 19(36): 6122-6124
- URL: https://www.wjgnet.com/1007-9327/full/v19/i36/6122.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i36.6122
Biliary ascariasis is a common problem in rural areas in China, especially in the Northwest region. Common presentations include biliary colic, acute cholangitis, obstructive jaundice, choledocholithiasis and acute cholecystitis[1]. In this report we describe a case with biliary ascariasis after endoscopic sphincterotomy for choledocholithiasis.
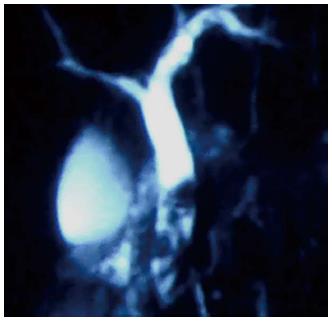
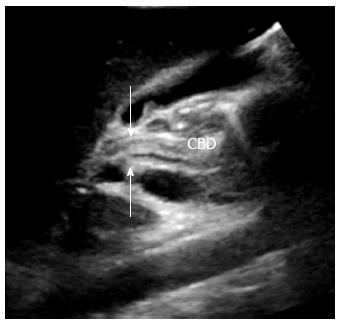
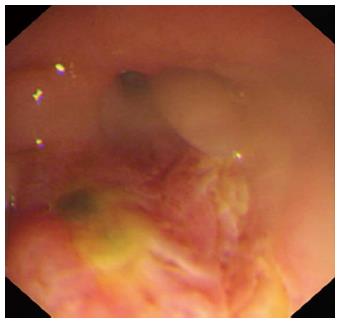
An 18-year-old Chinese woman presented with complaints of abdominal pain, fever and jaundice. Magnetic resonance cholangiopancreatography (MRCP) showed multiple common bile duct (CBD) stones (Figure 1). Routine endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic sphincterotomy were performed and several CBD stones were retrieved successfully. The recovery was uneventful until the onset of progressively intolerable abdominal pain two days later. Abdominal ultrasonography revealed a dilated common bile duct (10 mm) with an ill-defined linear echogenic shadow inside (Figure 2). The gallbladder was normal. Biliary ascariasis was suspected and ERCP was repeated. The head of a worm was at the sphincterotomy-performed papilla (Figure 3). One living ascaris of about 25 cm in length was removed using a dormia basket (Figure 4).
Endoscopic sphincterotomy is the treatment of choice for patients with choledocholithiasis. Its main complications include bleeding, pancreatitis, perforation and infection[2]. Biliary ascariasis, one of contributing factors of biliary stones, does not figure in the list. However, biliary ascariasis is a common complication of endoscopic sphincterotomy in some regions where ascariasis is epidemic. For example, Gupta et al[3] reported four cases of biliary ascariasis among 273 cases with post-endoscopic sphincterotomy for choledocholithiasis in Kashmir, India. Biliary ascariasis occurred only two days after sphincterotomy in the present study, which contrasts with the interval period of 2-24 wk in Gupta’s report[3].
Abdominal ultrasonography can facilitate the diagnosis of biliary ascariasis in most of cases. The characteristic sonographic feature of worms in the common bile duct is a long, linear, parallel echogenic strip, usually without acoustic shadowing[4]. ERCP, considered the gold standard for the diagnosis of biliary ascariasis, should be reserved for therapeutic rather than diagnostic use, because papillotomy may lead to reentry of the worm into the common bile duct[5]. In addition, sphincterotomy is not recommended unless a basket cannot be introduced inside the common bile duct to hold the ascaris[6]. Dead ascaris and stones in the same patients have been reported to be pulled out simultaneously through the CBD[6]. In this patient, CBD stones were removed successfully by the first ERCP and no signs of either living or dead biliary ascaris were found. The living ascaris found by the second ERCP was thought to have resulted from the entry of the worm into the common bile duct through the open papilla; therefore, anthelmintics were used to prevent reentry of any other ascaris residing in the small bowel. Six months of follow-up were uneventful.
Previously, Zargar et al[7] described the endoscopic management of postoperative biliary ascariasis in 19 consecutive patients who underwent cholecystectomy and choledocholithotomy. ERCP was performed 4 to 16 d after biliary tract surgery and roundworms in the CBD were extracted from 10 patients, from the hepatic ducts of patients, or from both ducts in seven patients. Taken together, we suggest that endoscopic management is an effective and safe approach for extracting ascarids from the biliary tree of postoperative patients.
P- Reviewer Erpecum KJ S- Editor Gou SX L- Editor Stewart GJ E- Editor Zhang DN
| 1. | Baba AA, Shera AH, Bhat MA, Hakim S, Sheikh KA, Shah OJ. Management of biliary ascariasis in children living in an endemic area. Eur J Pediatr Surg. 2010;20:187-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Anderson MA, Fisher L, Jain R, Evans JA, Appalaneni V, Ben-Menachem T, Cash BD, Decker GA, Early DS, Fanelli RD. Complications of ERCP. Gastrointest Endosc. 2012;75:467-473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 299] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 3. | Gupta R, Agarwal DK, Choudhuri GD, Saraswat VA, Baijal SS. Biliary ascariasis complicating endoscopic sphincterotomy for choledocholithiasis in India. J Gastroenterol Hepatol. 1998;13:1072-1073. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Sharma M. Echogenic shadow in the common bile duct. Diagnosis: Biliary ascariasis. Gastroenterology. 2011;141:e14-e15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Sandouk F, Haffar S, Zada MM, Graham DY, Anand BS. Pancreatic-biliary ascariasis: experience of 300 cases. Am J Gastroenterol. 1997;92:2264-2267. [PubMed] |
| 6. | Alam S, Mustafa G, Rahman S, Kabir SA, Rashid HO, Khan M. Comparative study on presentation of biliary ascariasis with dead and living worms. Saudi J Gastroenterol. 2010;16:203-206. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Zargar SA, Khan BA, Javid G, Yattoo GN, Shah AH, Gulzar GM, Singh J, Khan MA, Shah NA. Endoscopic management of early postoperative biliary ascariasis in patients with biliary tract surgery. World J Surg. 2004;28:712-715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |