Published online Aug 7, 2013. doi: 10.3748/wjg.v19.i29.4823
Revised: April 18, 2013
Accepted: May 9, 2013
Published online: August 7, 2013
Processing time: 211 Days and 8.4 Hours
Dieulafoy’s-like lesions (DLs-like) represent a cause of obscure gastrointestinal bleeding, enteroscopy being the main diagnostic and therapeutic procedure. Frequently, more than one enteroscopy is needed to identify the bleeding vessel. In our practice, video capsule endoscopy (VCE) identified and guided therapy in four cases of DLs-like; three of them were localized on the small bowel. We report, for the first time, a diagnosis of colonic DL-like performed by colon capsule endoscopy. Two patients presented with severe cardiovascular disorders, being hemodynamically unstable during VCE examination. Based on the VCE findings, only one invasive therapeutic procedure per patient was necessary to achieve hemostasis. VCE and enteroscopy may be regarded as complementary procedures in patients with gut DLs-like.
Core tip: This case series emphasizes the role of capsule endoscopy in active obscure gastrointestinal bleeding, even in hemodynamically unstable patients, because it is able to identify the site of bleeding and to guide therapeutic procedures. Emergency capsule endoscopy reduces the number of diagnostic enteroscopies in Dieulafoy’s-like lesions of the small bowel and colon.
- Citation: Ciobanu L, Pascu O, Diaconu B, Matei D, Pojoga C, Tanţău M. Bleeding Dieulafoy’s-like lesions of the gut identified by capsule endoscopy. World J Gastroenterol 2013; 19(29): 4823-4826
- URL: https://www.wjgnet.com/1007-9327/full/v19/i29/4823.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i29.4823
Dieulafoy’s lesion (DL) is characterized by a small mucosal erosion involving an unusually large submucosal artery in an otherwise normal mucosa[1]. Even a predilection for proximal stomach was considered previously; no region of the gut is immune[1-3]. Characteristic histological lesions consist of a normal artery with an abnormally large diameter, maintaining a constant width of 1-3 mm, that runs a tortuous course within the submucosa and protrudes through a small mucosal defect, varying from 2 to 5 mm, which fibrinoid necrosis at its base[4]. The term DL-like is used to describe bleeding when angiographic, endoscopic ultrasound or pathological data are unavailable, the diagnosis being based on clinical and endoscopic features[4]. DLs are responsible for 3.5% of mid gastrointestinal bleeding[2]. The diagnosis is challenging, not only because of the small size of the lesion and the normal surrounding mucosa, but also because of the intermittent nature of bleeding; frequently more than one enteroscopic procedure being required for small bowel DLs-like.
In recent years, the extensive use of video capsule endoscopy (VCE) proved to be a useful procedure with high diagnostic yield in obscure gastrointestinal bleeding (OGIB)[5]. Recent reports also document the utility of this procedure in active, severe OGIB[5-8]. Some case reports describe DLs-like diagnosis on capsule endoscopy[9-11], but none of the larger series gives specific details on this topic. Colon capsule endoscopy, initially designed as a non-invasive procedure for colorectal cancer screening[12], with many technical improvements, can assess the entire length of the gut to identify sources of bleeding.
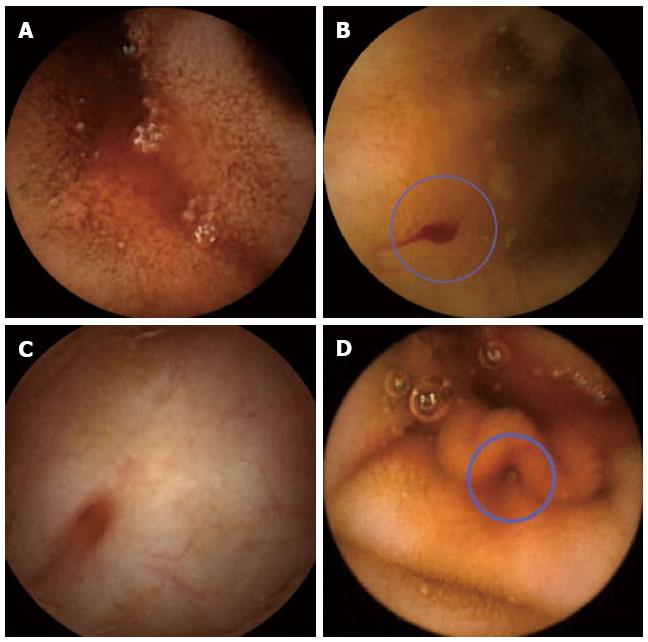
During 2006 to 2012, in our capsule endoscopy unit, 227 VCE procedures were performed, 70 patients being investigated for overt OGIB. Four DLs-like were diagnosed by capsule endoscopy (three localized on the small bowel and one in the colon) in active gastrointestinal bleeding and successful guided therapeutic procedures were performed. Capsule endoscopy findings suggestive of DLs-like were: active blood streaming from a minute mucosa defect or through surrounding mucosa, visualization of a protruding vessel or the appearance of a fresh, densely adherent clot with a narrow point of attachment to a minute mucosal defect or to normal appearing mucosa, as described in conventional endoscopy[1].
A 69-year-old female, receiving long-term warfarin therapy for a prosthetic mitral valve was referred to our department for intermittent melena in the last four weeks. No bleeding source was identified after two upper and lower gastrointestinal endoscopies. She did not use nonsteroidal anti-inflammatory drugs (NSAIDs). At the time of VCE, her blood pressure was 90/60 mmHg, her heart rate was 110 beats/min and her hemoglobin level was 6.8 g/dL. Capsule endoscopy revealed significant amounts of fresh blood in the first jejunal loop (Figure 1A), without an identifiable lesion, highly suggestive of DL-like. On the same day, an emergency push enteroscopy was performed, with therapeutic hemoclipping of jejunal bleeding mucosal break. Her clinical status significantly improved, and she was discharged a few days later, with a hemoglobin level of 10 g/dL. She did not experience any gastrointestinal bleeding during a 5-year follow-up period.
A 58-year-old female who experienced four episodes of melena in the last five years, without an identifiable source of bleeding at multiple upper and lower endoscopies. At the time of VCE she had melena and a hemoglobin level of 5.8 g/dL. Capsule endoscopy revealed a very small mucosal break suggestive of DL-like (Figure 1B), with a significant amount of fresh blood in the jejunum. Based on these findings, 12 h later, an emergency enteroscopy was performed that was able to stop the bleeding by hemoclipping. She remained in excellent clinical condition 1 year later.
A 68-year-old female presented two severe episodes of melena and hematochezia with hemorrhagic shock in the last five months. She was not using NSAIDs and no other symptoms were present. She was investigated with upper and lower gastrointestinal endoscopies on the first episode without an identifiable source of bleeding. On the second episode of bleeding, another gastroscopy did not find any bleeding source, and she was referred for capsule endoscopy. After a standard preparation we used a colon capsule endoscopy to examine the entire gut mucosa. Capsule endoscopy found fresh blood only in the colon with a mucosal break (Figure 1C). Colonoscopy was performed the same night: a bleeding vessel was found on the transverse colon and hemoclips were placed. The patient was released from hospital five days later in good clinical condition. She did not experience other episodes of gastrointestinal bleeding during a 2 years follow up period.
Case 4 was an 80-year-old female patient with known cardiovascular disorders that required both antiagregants (low doses of aspirin) and anticoagulants (warfarin). She was admitted for a severe episode of hematochezia, with hemorrhagic shock, with a 5.8 g/dL hemoglobin level. Upper and lower endoscopies did not find the source of the bleeding; therefore, a capsule endoscopy was performed. The patient being closely monitored because she was hemodynamically unstable. VCE detected active bleeding in the proximal jejunum and a small mucosal break (Figure 1D). An emergency push enteroscopy was performed the next morning, which was able to place metal clips on the bleeding jejunum mucosal vessel. Her clinical condition improved and she left the hospital five days later. During a 6-mo follow up period she did not experience another episode of gastrointestinal bleeding.
DLs account for 1%-2% of all gastrointestinal bleeding episodes[4]. From 1884, when it was first described by Gallard[13], until today, the management of DLs-like has represented a challenge. The patients present with acute onset of bleeding, frequently without identifiable risk factors, sometimes life-threatening. Identifying the site of bleeding by endoscopy procedures may be difficult, as the dimension of the mucosal break is minute and is not easy to visualize, in the context of large amounts of blood or if the bleeding stops[4]. These aspects are even more relevant for small bowel localization, as the bleeding lesions are more difficult to reach. Small bowel DLs-like account for 3.5% of OGIB, as assessed recently by Dulic-Lakovic et al[2] in a large retrospective study based on enteroscopy findings in patients with OGIB. Enteroscopy, even if it is invasive, requires sedation and sometimes may be technically difficult, has proved to be a very efficient diagnostic and therapeutic procedure for these lesions. Patients with small bowel DLs-like frequently require more than one enteroscopy until the source is identified and treated; a mean of 1.5 enteroscopy per case being reported[2].
Previous case reports document a correct diagnosis of DLs-like achieved by VCE, with subsequently successful guided therapeutic procedures[9-11]. All our cases also argue for the good performance of VCE in identifying and guiding therapy, even in hemodynamically unstable patients (cases 1 and 4). An important issue to consider in these patients is the timing of both VCE and enteroscopy. In active bleeding patients, with hemodynamically instability, VCE is not routinely used, as it may be considered time consuming; however, recent studies report a good diagnostic yield in identifying the site of acute bleeding in 75% of patients and the source of bleeding in 67% of cases[6-8]. Based on these findings, successful guided therapy was performed in 73%-76% of patients[7,8]. In these studies, no specific results or discussion are presented for DLs-like. Our patients presented clinical signs of active bleeding at the time of VCE, which substantially increased the chance for detecting blood or lesions. Capsule endoscopy images were interpreted immediately after the procedure and were followed by emergency endoscopy in the next few hours.
To the best of our knowledge, no previous report describes colon DL-like diagnosed with colon VCE. Previous studies reported missing bleeding lesions localized in the stomach or cecum, by conventional endoscopies and identified on capsule endoscopy[14,15]. In case 3, previous colonoscopy did not find fresh blood in the colon, meaning that DL was inactive. A second colonoscopy guided by findings on VCE enabled the correct identification of the lesion and treatment.
In our patients, after correct localization of the bleeding active site by VCE, only one interventional endoscopy per patient was needed for treatment (3 push enteroscopies and 1 colonoscopy), hemostasis being achieved by hemoclipping. VCE findings provided a very good selection for subsequent therapeutic procedures, reducing the number of interventional diagnostic maneuvers. Hemoclipping is a highly effective therapy, very well documented for gastric DLs-like[16]. Angiography can identify and treat DLs by embolization, being used in difficult to treat cases[3]. Surgery could be regarded as an alternative treatment only if the bleeding is not stopped by endoscopic or angiographic procedures[3].
No pathogenetic association between NSAIDs and DLs-like has been identified in the literature[17,18]. However, as DLs-like seem to be more frequent in older patients with significant comorbidities[4] that may require NSAIDs and/or anticoagulants, it is assumed that concomitant administration of these agents prolongs and increases the severity of bleeding, as was observed in cases 1 and 4. In addition, differential diagnosis may be challenging, as NSAIDs enteropathy can display a wide spectrum of features from mucosal breaks to large bleeding ulcers[19]. In actively bleeding NSAIDs enteropathy, multiple erosions or ulcers could be documented as necro-inflammation, representing the background pathology induced by these drugs[20].
The limitations of this report are related to the retrospective analyses of cases and inclusions of patients with active OGIB, highly suspicious of DLs-like. Despite these limitations, this case series emphasizes the role of capsule endoscopy in reducing the number of diagnostic enteroscopies in DLs-like.
In conclusion, VCE should be considered in active OGIB, even in hemodynamically unstable patients, because it is able to identify the site of bleeding and to guide therapeutic procedures.
P- Reviewer Szilagyi A S- Editor Huang XZ L- Editor Stewart GJ E- Editor Zhang DN
| 1. | Dy NM, Gostout CJ, Balm RK. Bleeding from the endoscopically-identified Dieulafoy lesion of the proximal small intestine and colon. Am J Gastroenterol. 1995;90:108-111. [PubMed] |
| 2. | Dulic-Lakovic E, Dulic M, Hubner D, Fuchssteiner H, Pachofszky T, Stadler B, Maieron A, Schwaighofer H, Püspök A, Haas T. Bleeding Dieulafoy lesions of the small bowel: a systematic study on the epidemiology and efficacy of enteroscopic treatment. Gastrointest Endosc. 2011;74:573-580. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (2)] |
| 3. | Patel P, Tobi M. Dieulafoy-like lesion bleeding: in the loop. Gastroenterol Hepatol (N Y). 2011;7:271-274. [PubMed] |
| 4. | Baxter M, Aly EH. Dieulafoy’s lesion: current trends in diagnosis and management. Ann R Coll Surg Engl. 2010;92:548-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 183] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 5. | Liao Z, Gao R, Xu C, Li ZS. Indications and detection, completion, and retention rates of small-bowel capsule endoscopy: a systematic review. Gastrointest Endosc. 2010;71:280-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 561] [Cited by in RCA: 476] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 6. | Hogan RB, Pareek N, Phillips P, Haick A, Hogan RB. Video capsule endoscopy in life-threatening GI hemorrhage after negative primary endoscopy (with video). Gastrointest Endosc. 2009;69:366-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Almeida N, Figueiredo P, Lopes S, Freire P, Lérias C, Gouveia H, Leitão MC. Urgent capsule endoscopy is useful in severe obscure-overt gastrointestinal bleeding. Dig Endosc. 2009;21:87-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Lecleire S, Iwanicki-Caron I, Di-Fiore A, Elie C, Alhameedi R, Ramirez S, Hervé S, Ben-Soussan E, Ducrotté P, Antonietti M. Yield and impact of emergency capsule enteroscopy in severe obscure-overt gastrointestinal bleeding. Endoscopy. 2012;44:337-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 74] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 9. | de Franchis R, Rondonotti E, Abbiati C, Beccari G, Gullotta R, Primignani M, Vecchi M. Successful identification of a jejunal Dieulafoy lesion by wireless capsule enteroscopy: a case report. Dig Liver Dis. 2002;34 Suppl 1:A118. [DOI] [Full Text] |
| 10. | Sai Prasad TR, Lim KH, Lim KH, Yap TL. Bleeding jejunal Dieulafoy pseudopolyp: capsule endoscopic detection and laparoscopic-assisted resection. J Laparoendosc Adv Surg Tech A. 2007;17:509-512. [PubMed] |
| 11. | De Palma GD, Patrone F, Rega M, Simeoli I, Masone S, Persico G. Actively bleeding Dieulafoy’s lesion of the small bowel identified by capsule endoscopy and treated by push enteroscopy. World J Gastroenterol. 2006;12:3936-3937. [PubMed] |
| 12. | Eliakim R, Fireman Z, Gralnek IM, Yassin K, Waterman M, Kopelman Y, Lachter J, Koslowsky B, Adler SN. Evaluation of the PillCam Colon capsule in the detection of colonic pathology: results of the first multicenter, prospective, comparative study. Endoscopy. 2006;38:963-970. [PubMed] |
| 13. | Gallard T. Aneurysmes miliaires de l’estomac, donnant lieu a des hematemeses mortelle. Bull Soc Med Hop Paris. 1884;1:84-91. |
| 14. | Rana SS, Bhasin DK, Singh K. Colonic lesions in patients undergoing small bowel capsule endoscopy. Int J Colorectal Dis. 2011;26:699-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Riccioni ME, Shah S, Urgesi R, Costamagna G. Case report: a lesson in capsule endoscopy. Hepatogastroenterology. 2008;55:1006-1007. [PubMed] |
| 16. | Park CH, Sohn YH, Lee WS, Joo YE, Choi SK, Rew JS, Kim SJ. The usefulness of endoscopic hemoclipping for bleeding Dieulafoy lesions. Endoscopy. 2003;35:388-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 62] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Juler GL, Labitzke HG, Lamb R, Allen R. The pathogenesis of Dieulafoy’s gastric erosion. Am J Gastroenterol. 1984;79:195-200. [PubMed] |
| 18. | Lee YT, Walmsley RS, Leong RW, Sung JJ. Dieulafoy’s lesion. Gastrointest Endosc. 2003;58:236-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 133] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 19. | Maiden L. Capsule endoscopic diagnosis of nonsteroidal antiinflammatory drug-induced enteropathy. J Gastroenterol. 2009;44 Suppl 19:64-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 77] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 20. | Konaka A, Nishijima M, Tanaka A, Kunikata T, Kato S, Takeuchi K. Nitric oxide, superoxide radicals and mast cells in pathogenesis of indomethacin-induced small intestinal lesions in rats. J Physiol Pharmacol. 1999;50:25-38. [PubMed] |