Published online Jul 7, 2013. doi: 10.3748/wjg.v19.i25.4072
Revised: March 20, 2013
Accepted: May 7, 2013
Published online: July 7, 2013
Processing time: 149 Days and 4.7 Hours
AIM: To compare single incision laparoscopic surgery for an appendectomy (SILS-A) with conventional laparoscopic appendectomy (C-LA) when implemented by experienced surgeons.
METHODS: Studies and relevant literature regarding the performance of single-incision laparoscopic surgery vs conventional laparoscopic surgery for appendectomy were searched for in the Cochrane Central Register of Controlled Clinical Trials, MEDLINE, EMBASE and World Health Organization international trial register. The operation time (OR time), complications, wound infection and postoperative day using SILS-A or C-LA were pooled and compared using a meta-analysis. The risk ratios and mean differences were calculated with 95%CIs to evaluate the effect of SILS-A.
RESULTS: Sixteen recent studies including 1624 patients were included in this meta-analysis. These studies demonstrated that, compared with C-LA, SILS-A has a similar OR time in adults but needs a longer OR time in children. SILS-A has similar complications, wound infection and length of the postoperative day in adults and children, and required similar doses of narcotics in children, the pooled mean different of -0.14 [95%CI: -2.73-(-2.45), P > 0.05], the pooled mean different of 11.47 (95%CI: 10.84-12.09, P < 0.001), a pooled RR of 1.15 (95%CI: 0.72-1.83, P > 0.05), a pooled RR of 1.9 (95%CI: 0.92-3.91, P > 0.05), a pooled RR of 1.01 (95%CI: 0.51-2.0, P > 0.05) a pooled RR of 1.86 (95%CI: 0.77-4.48, P > 0.05), the pooled mean different of -0.25 (95%CI: -0.50-0, P = 0.05) the pooled mean different of -0.01 (95%CI: -0.05-0.04, P > 0.05) the pooled mean different of -0.13 (95%CI: -0.49-0.23, P > 0.05) respectively.
CONCLUSION: SILS-A is a technically feasible and reliable approach with short-term results similar to those obtained with the C-LA procedure.
Core tip: Single incision laparoscopic surgery for an appendectomy (SILS-A) is widely accepted and has become the best option for treatment of appendicitis. Compared with conventional laparoscopic appendectomy, the safety and efficacy of SILS-A is not known. This study clarified that SILS-A has a similar operation time in adults but needs more time in children, has similar complications, wound infection and length of the postoperative day in adults and children, and needs similar doses of narcotics in children.
- Citation: Li P, Chen ZH, Li QG, Qiao T, Tian YY, Wang DR. Safety and efficacy of single-incision laparoscopic surgery for appendectomies: A meta-analysis. World J Gastroenterol 2013; 19(25): 4072-4082
- URL: https://www.wjgnet.com/1007-9327/full/v19/i25/4072.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i25.4072
Today, approximately 8% of the population will undergo appendectomy for acute appendicitis over their lifetime in Europe. An appendectomy comprises the surgical resection of the appendix and is frequently performed as an emergency process in the management of a patient suffering from acute appendicitis, a condition in which the appendix becomes inflamed and putrescent. The operation can be performed with minimally invasive surgery or as an open procedure.
Laparoscopic surgery was first used about 100 years ago, and the concept of minimally invasive surgery has significantly affected the field of traditional surgery. The first laparoscopic appendectomy was performed by the gynecologist Semm[1]. In a classic laparoscopic appendectomy, three to four incisions are required for the placement of multiple trocars. Driven by a quest toward less abdominal trauma in surgery, improved cosmesis, the potential reduction in postoperative pain, and a shorter hospital stay, specialty cameras, ports, and instruments have been developed, and minimal access surgery has undergone an accelerated process of evolution. A recent development in appendectomy has been the introduction of less invasive methods.
Single incision laparoscopic surgery applies a single multi-luminal port, or multiple mono-luminal ports, through a single skin incision. With the appearance of natural orifice translumenal endoscopic surgery, single incision laparoscopic surgery for an appendectomy (SILS-A) can be used to perform advanced[2-10], as well as preliminary procedures[11-24]. While this technique has been embraced by surgeons worldwide, the procedures and instruments used are still in the basic stages of investigation. Currently, two different methods exist for single-incision access. One involves the application of traditional, low profile laparoscopic ports that are clustered within a single skin incision, but penetration the peritoneal cavity through separate fascial incisions. The other involves the adoption of specialized ports created to provide multiple channels through a single port for one larger fascial incision. Both of methods have a good cosmetic effect. Despite its ameliorating effects, conventional laparoscopic appendectomy (C-LA) still requires three to four abdominal incisions for completion of the procedure. Each incision adds to potential morbidity risks, including bleeding, hernia, or internal organ damage[25,26]. There is little published data on the feasibility, safety, and clinical advantage of the procedure. Therefore, this study will analyze and compare the short-term surgical results of SILS-A and C-LA. The primary aim of this meta-analysis was to evaluate SILS-A vs C-LA; the secondary aims were to determine the difficulties, limitations or advantages of SILS-A.
Four bibliographic databases (Cochrane Central Register of Controlled Clinical Trials, MEDLINE, EMBASE and the World Health Organization international trial register) were searched for all relevant literature, including articles referenced in the publications. The medical subject headings (MeSH) and keywords searched for individually and in combination were as follows: “single-incision laparoscopic surgery”“multiport laparoscopic surgery” or “conventional laparoscopic” and “appendectomies”. The last search was done on January 20, 2013.
The inclusion criteria were as follows: (1) patients should be at least 1 year of age; (2) suspected acute appendicitis on clinical and radiographic (computed tomography) grounds; (3) male or female (excluding pregnant females); (4) patients with American Society of Anesthesiology score < 3; (5) patients informed about the study, and will have read, understood and signed the patient informed; and (6) studies that provided information on at least one of the outcome measures. When a study reporting the same patient cohort was included in several publications, only the most recent or complete study was selected.
The exclusion criteria were as follows: (1) prior open laparotomy with incision through the umbilicus; (2) mental illness, dementia, or inability to provide informed consent; (3) chronic pain requiring daily medication (including opiates and NSAIDs); (4) pregnancy; (5) case reports; (6) articles that were not full text, or non-comparative studies; and (7) open operations.
For identified eligible studies, two reviewers using a standard form containing pre-specified outcomes would have undertaken data extraction independently. Clarification was sought where there was potential data collection but not reported. Any differences of opinion were resolved among the reviewers, and where necessary referred to a fourth party for arbitration.
Statistical analysis was performed using Review Manager (RevMan) software version 5.0.0 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark). A pooled RR and a pooled Mean Different with 95%CI were used to assess outcomes of the studies; statistical heterogeneity was tested by the χ2 test. According to the Forest plot, heterogeneity was limited, so we used the Mantel-Haenszel fixed effect model. The significance of the pooled RR was determined by the Z test and statistical significance was considered at P < 0.05. Publication bias was estimated using a funnel plot with an Egger’s linear regression test, and funnel plot asymmetry on the natural logarithm scale of the RR was measured by a linear regression approach.
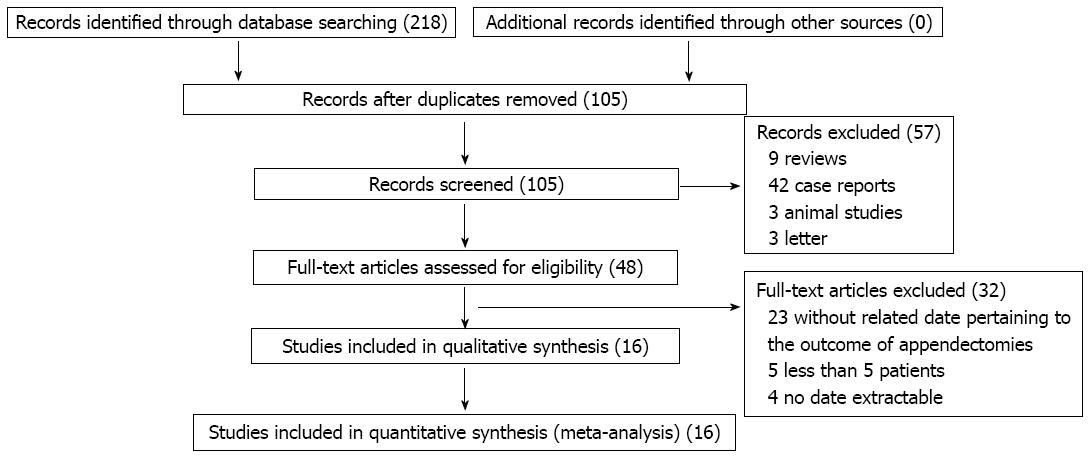
In total, 16 studies were included in the meta-analysis[27-42]. All of these studies were published after 2009 and comprised 751 adult patients, of whom 332 were operated on using SILS-A and 419 were operated on using C-LA. The sample size of the trials ranged from 15 to 108. Eight hundred and seventy three of the patients were children, of whom 428 were operated on using SILS-A and 445 were operated on using C-LA. The sample size of the trials ranged from 8 to 180. Moreover, some studies reported single-incision laparoscopic surgery for appendicitis, but did not report information regarding C-LA and were therefore not compared in this meta-analysis. Other studies did not provide any information about SILS-A vs C-LA, and were excluded in present meta-analysis (Figure 1). Tables 1-4 list the main characteristics of the 16 studies included in this analysis.
| Ref. | Year | SILS-A (n) | C-LA (n) | Age (yr) | M:F | ||
| SILS-A | C-LA | SILS-A | C-LA | ||||
| Lee et al[27] | 2009 | 72 | 108 | 30.3 ± 16.4 | 33.6 ± 18.6 | 24:46 | 56:52 |
| Cho et al[28] | 2011 | 23 | 20 | 44.7 | 39.2 | 14:9 | 11:9 |
| Teoh et al[29] | 2011 | 30 | 60 | 32.97 ± 13.31 | 34.88 ± 11.45 | 19:11 | 38:22 |
| Park et al[30] | 2012 | 42 | 62 | 23.9 ± 11.9 | 29.9 ± 12.2 | 14:28 | 42:21 |
| Kim et al[31] | 2011 | 17 | 33 | 21.0 | 28.0 | 1:10 | 21:12 |
| Vilallonga et al[32] | 2012 | 46 | 41 | 34.2 (13.3) | 37.7 (13.2) | 19:27 | 22:19 |
| Raakow et al[39] | 2011 | 20 | 20 | 27.75 ± 8.26 | 31.75 ± 9.30 | 8:12 | 10:10 |
| Amos et al[40] | 2011 | 27 | 17 | 37.74 ± 18.85 | 33.71 ± 12.50 | 6:21 | 6:11 |
| Chow et al[41] | 2010 | 40 | 33 | 31.65 ± 15.36 | 29.85 ± 14.93 | 18:22 | 15:18 |
| Kang et al[42] | 2010 | 15 | 25 | 35.5 ± 13.2 | 37.9 ± 14.5 | 8:07 | 14:11 |
| Ref. | Year | SILS-A (n) | C-LA (n) | Age | M:F | ||
| SILS-A | C-LA | SILS-A | C-LA | ||||
| Perez et al[33] | 2012 | 25 | 25 | 8.7 ± 0.6 | 8.9 ± 0.6 | 10:15 | 15:10 |
| Chandler et al[34] | 2010 | 50 | 45 | 11.1 ± 3.6 | 11.7 ± 3.8 | 26:24 | 34:11 |
| Mayer et al[35] | 2011 | 8 | 31 | 12.3 ± 2.4 | 12.3 ± 2.4 | ||
| St Peter et al[36] | 2011 | 180 | 180 | 11.1 ± 3.5 | 11.1 ± 3.3 | 99:81 | 92:88 |
| Knott et al[37] | 2012 | 135 | 139 | 11.0 ± 3.5 | 10.9 ± 3.4 | 72:63 | 70:69 |
| Kang et al[38] | 2011 | 30 | 25 | 9.3 ± 4.0 | 8.7 ± 3.5 | 17/13 | 14/11 |
| Ref. | Postoperative day (d) | Complications | OR time (min) | Wound infection | ||||
| SILS-A | C-LA | SILS-A | C-LA | SILS-A | C-LA | SILS-A | C-LA | |
| Lee et al[27] | 2.0 ± 1.4 | 2.0 ± 1.3 | 7 | 12 | 41.0 ± 13.6 | 37.1 ± 18.6 | 4 | 7 |
| Cho et al[28] | 1 | 0 | 61.8 ± 23.6 | 61.1 ± 13.7 | ||||
| Teoh et al[29] | 5 | 5 | 64.67 ± 26.09 | 71 ± 21.45 | 2 | 4 | ||
| Park et al[30] | 2.6 ± 1.0 | 2.9 ± 1.9 | 6 | 6 | 51.6 ± 16.8 | 55.8 ± 15.2 | 3 | 2 |
| Kim et al[31] | 0 | 2 | 0 | 2 | ||||
| Vilallonga et al[32] | 2 | 0 | 40.4 ± 17.5 | 35.0 ± 13.6 | ||||
| Raakow et al[39] | 4.12 ± 0.61 | 4.65 ± 0.98 | 1 | 2 | 48.0 ± 13.2 | 49.0 ± 19.9 | 1 | 1 |
| Amos et al[40] | 3.70 ± 2.52 | 3.82 ± 1.24 | 0 | 1 | 41.37 ±10.19 | 54.41 ± 21.93 | 5 | |
| Chow et al[41] | 1.36 ± 0.95 | 2.36 ± 2.62 | 2 | 3 | 60.0 ± 15.56 | 70.2 ± 21.23 | 2 | 2 |
| Kang et al[42] | 6.8 ± 1.8 | 6.4 ± 1.6 | 3 | 2 | 62.5 ± 18.7 | 53.7 ± 11.5 | 1 | 1 |
| Ref. | Postoperative day (d) | Complications | OR time (min) | Wound infection | Doses of narcotics | |||||
| SILS-A | C-LA | SILS-A | C-LA | SILS-A | C-LA | SILS-A | C-LA | SILS-A | C-LA | |
| Perez et al[33] | 1 | 0 | 46.8 ± 3.7 | 34.8 ± 2.5 | ||||||
| Chandler et al[34] | 1.1 ± 0.4 | 1.2 ± 0.5 | 5 | 0 | 33.8 ± 9 | 26.3 ± 7.5 | 4 | 0 | 0.9 ± 0.9 | 1.4 ± 1.3 |
| Mayer et al[35] | 3.63 ± 1.2 | 3.68 ± 1.3 | 2 | 3 | 68.5 ± 19.9 | 66.2 ± 19.5 | 4.75 ± 3.3 | 7.33 ± 3.0 | ||
| St Peter et al[36] | 0.95 ± 0.3 | 0.93 ± 0.3 | 6 | 3 | 35.2 ± 14.5 | 29.8 ± 11.6 | 6 | 3 | 9.6 ± 4.9 | 8.5 ± 4.3 |
| Knott et al[37] | 0.92 ± 0.2 | 0.94 ± 0.3 | 2 | 3 | 34.0 ± 13.6 | 29.6 ± 13.6 | 2 | 3 | 5.7 ± 3.5 | 5.3 ± 3.2 |
| Kang et al[38] | 4.0 ± 1.5 | 3.8 ± 2.0 | 2 | 2 | 46.2 ± 18.5 | 40.5 ± 15.2 | 2 | 1 | ||
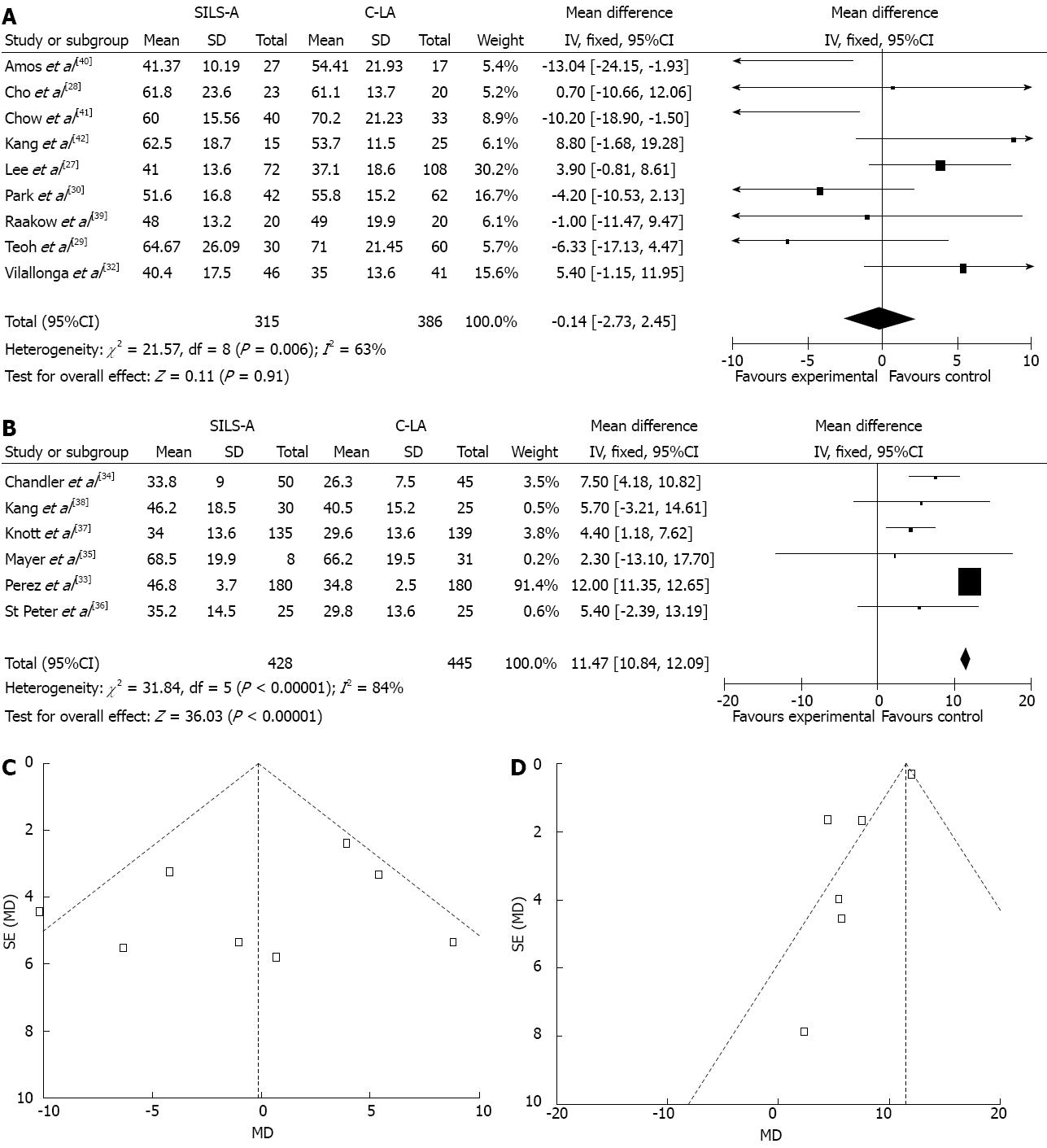
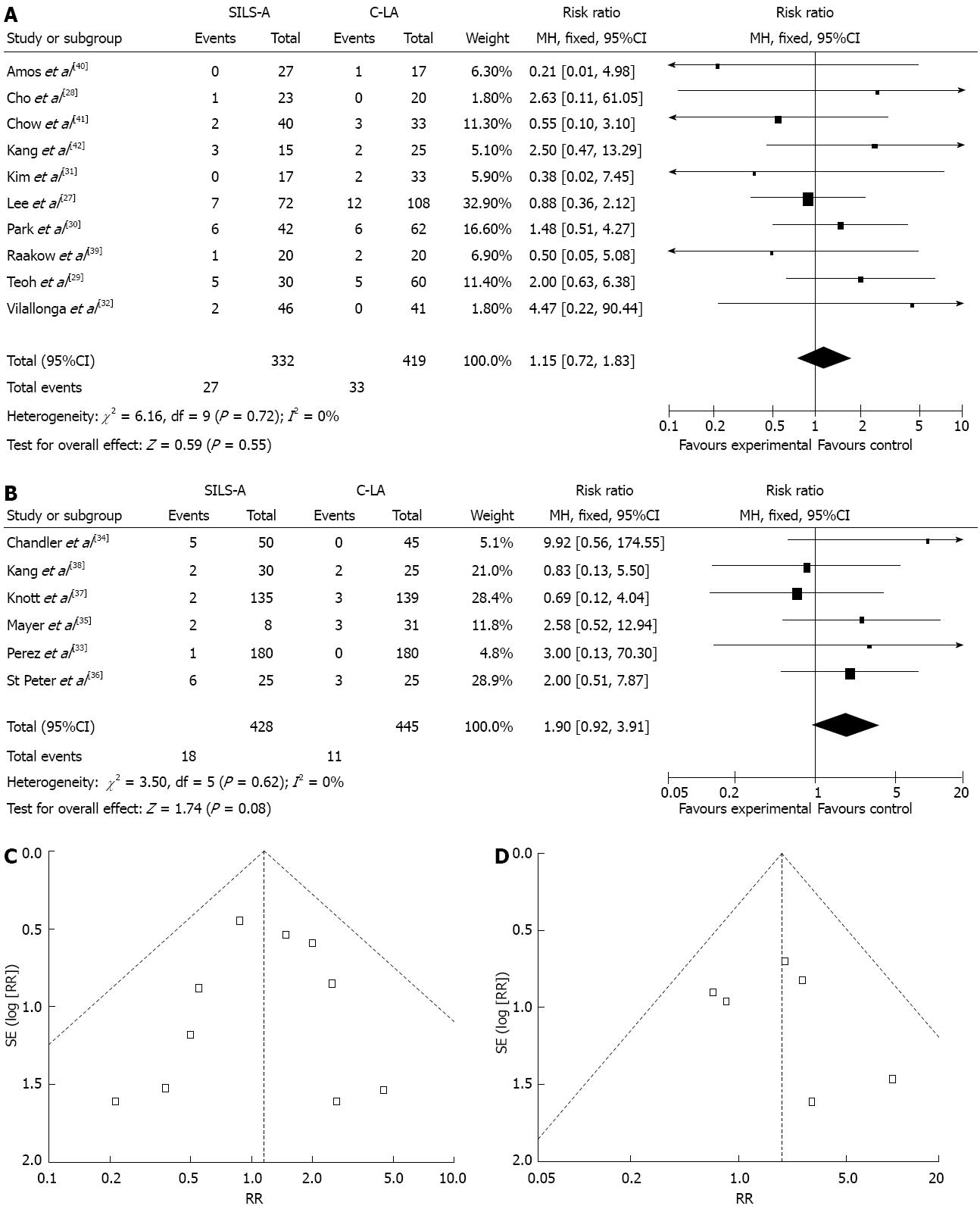
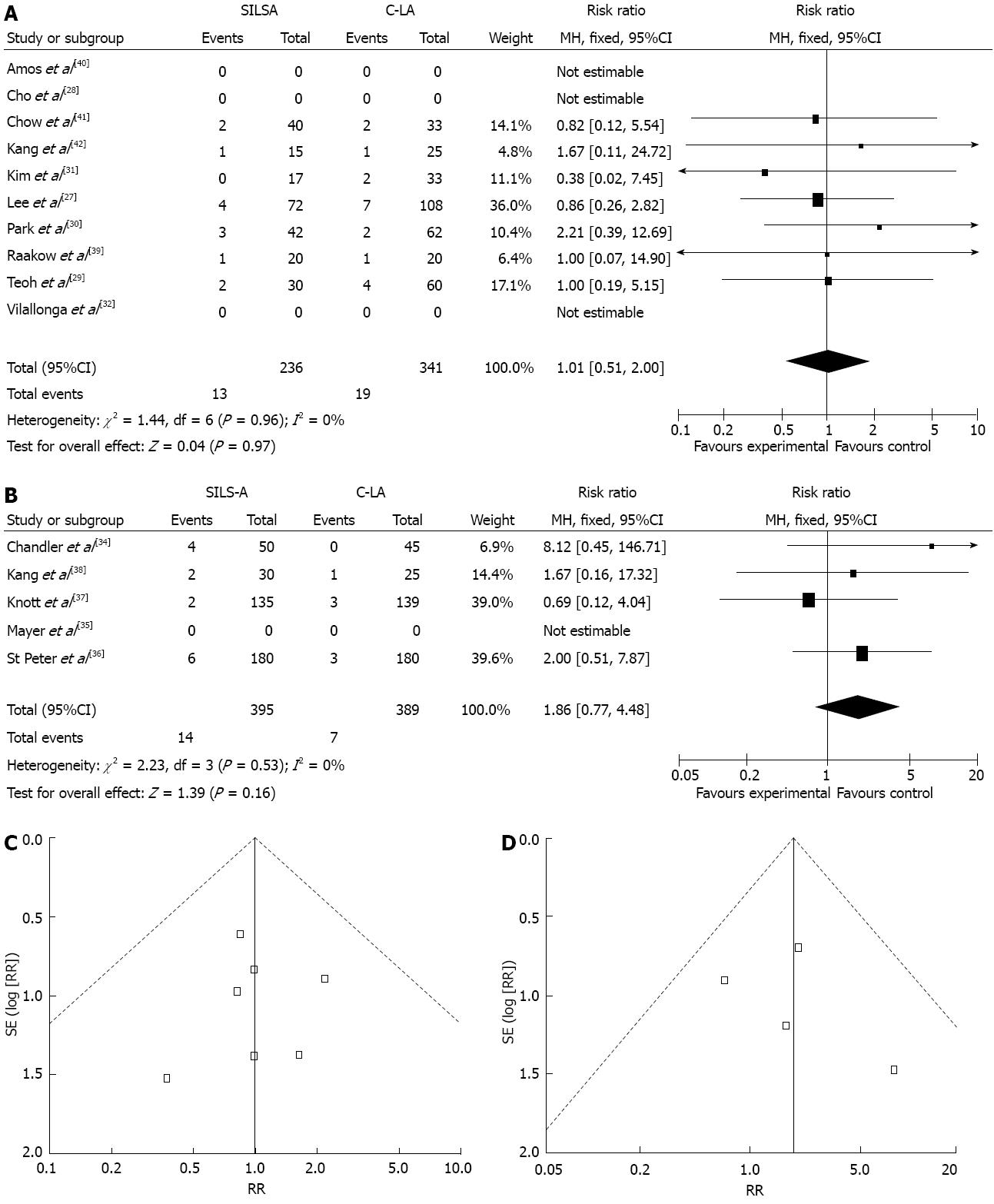
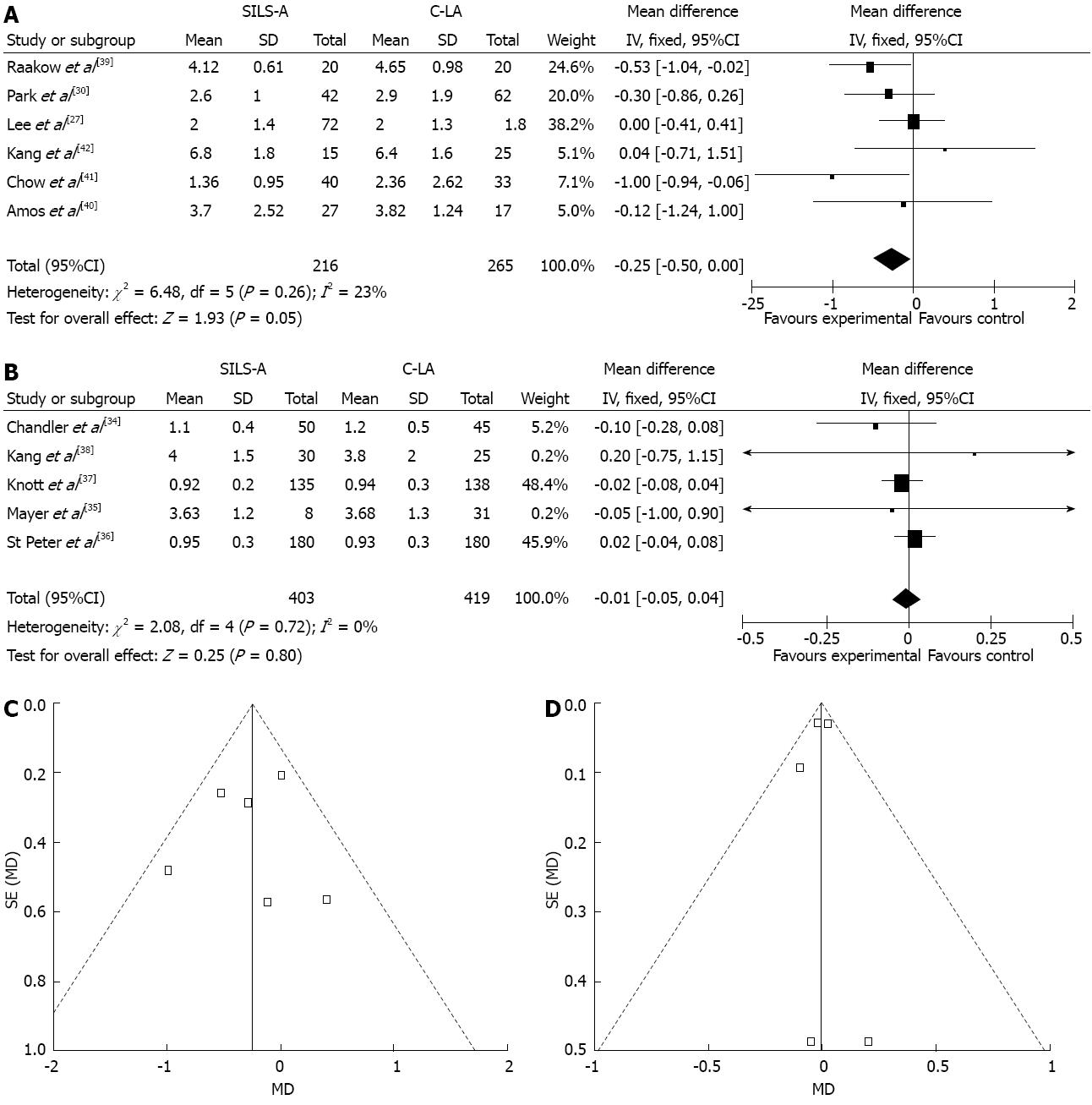
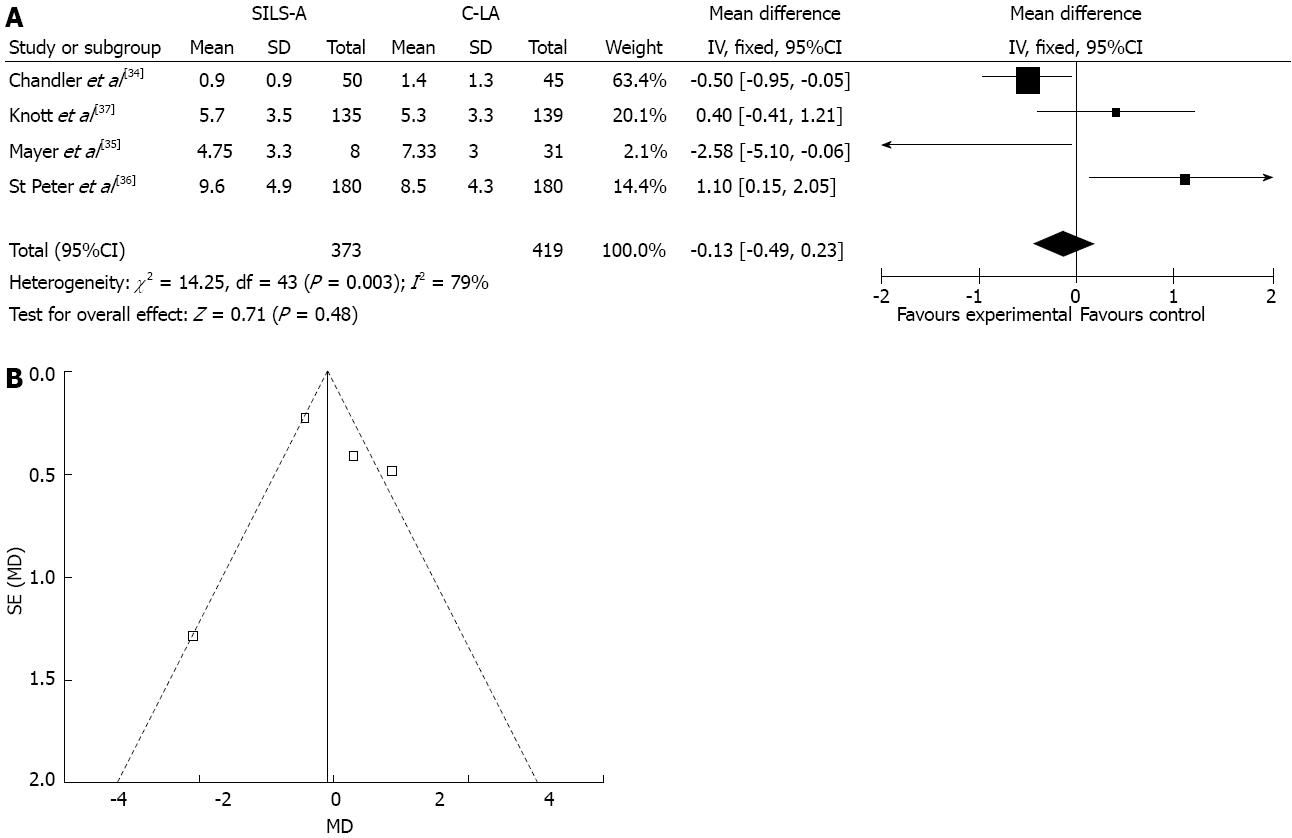
The present meta-analysis demonstrated the pooled mean different of [-0.14, 95%CI: -2.73-(-2.45), P > 0.05, Figure 2A], the pooled RR of 1.15 (95%CI: 0.72-1.83), P > 0.05, Figure 3A) a pooled RR of 1.01 (95%CI: 0.51-2.0), P > 0.05, Figure 4A, a pooled mean different of -0.25 (95%CI: -0.5-0.0), P = 0.05, Figure 5A, a pooled mean different of 11.47 (95%CI: 10.84-12.09), P < 0.001, Figure 2B, a pooled RR of 1.9 (95%CI: 0.92-3.91), P > 0.05, Figure 3B, the pooled RR of 1.86 (95%CI: 0.77-4.48), P > 0.05, Figure 4B, the pooled mean different of -0.01 (95%CI: -0.05-0.04), P > 0.05, Figure 5B, the pooled mean different of -0.13 (95%CI: -0.49-0.23), P > 0.05, Figure 6, respectively. It revealed that SILS-A is feasible, and appears to have results similar to C-LA in our comparisons. But, in children, SILS-A needs more operative time than C-LA.
Operation time (min): Nine studies (701 patients) provided data on operation time for adults. The pooled results indicated that SILS-A has similar results to C-LA [weighted mean differences (WMD), -0.14 (95%CI: -2.73-2.45), P > 0.05]. The χ2and I2 were 21.57 (P = 0.0006) and 63%, respectively, indicating heterogeneity among the studies (Figure 2A). Six studies (873 patients) provided data on operation time for children. The pooled the indicated that SILS-A requires more time than C-LA [WMD, 11.47 (95%CI: 10.84-12.09), P < 0.001]. The χ2 and I2 were 31.84 (P < 0.001) and 84%, respectively, indicating heterogeneity among the studies (Figure 2B).
Complications: Ten studies (751 patients) provided data on complications in adults. Complications occurred in 27 of 332 (8.1%) patients after SILS-A and in 33 of 419 (7.8%) after C-LA. Pooling the results indicated that SILS-A had slightly, but not significantly, more complications than C-LA [WMD 1.15 (95%CI: 0.72-1.83), P > 0.05]. The χ2 and I2 were 6.16 (P = 0.72) and 0%, which excluded heterogeneity in the studies (Figure 3A). Six studies (873 patients) provided data on complications in children. Complications occurred in 18 of 428 (4.2%) patients after SILS-A and in 11 of 445 (2.4%) patients after C-LA. Pooling the results indicated that SILS-A and C-LA have the similar levels of complications [WMD a pooled RR of 1.9 (95%CI: 0.92-3.91), P > 0.05]. The χ2 and I2 were 3.5 (P = 0.62) and 0%, which excluded heterogeneity in the studies (Figure 3B).
Wound infection: Seven studies (577 patients) provided data on wound infections in adults. Wound infections occurred in 13 of 236 (5.5%) patients after SILS-A and in 19 of 341 (5.6%) patients after C-LA. Pooling the results indicated that SILS-A and C-LA have the similar levels of wound infection [WMD 1.01 (95%CI: 0.51-2.0), P > 0.05]. The χ2 and I2 were 1.44 (P = 0.96) and 0%, which excludes heterogeneity in the studies (Figure 4A). Five studies (784 patients) provided data on wound infections in children. Wound infections occurred in 14 of 395 (3.5%) patients after SILS-A and in 7 of 398 (1.7%) patients after C-LA. The results indicated that SILS-A has more wound infections, but at an acceptable level. Pooling the results of wound infection [WMD 1.86 (95%CI: 0.77-4.48), P > 0.05]. The χ2 and I2 were 2.23 (P = 0.53) and 0%, which excluded heterogeneity in the studies (Figure 4B).
Postoperative days (d): Six studies (481 patients) provided data on postoperative days for adult. Pooling the results indicated that SILS-A has the slightly better results than C-LA [WMD -0.25 (95%CI: -0.50-0), P > 0.05]. The χ2 and I2 were 6.48 (P = 0.26) and 23%, respectively, indicating heterogeneity among the studies (Figure 5A). Five studies (822 patients) provided data on postoperative days for children. Pooling the results indicated that SILS-A has the same results as C-LA [WMD, -0.01 (95%CI: -0.05-0.04), P > 0.05]. The χ2 and I2 were 2.08 (P = 0.72) and 23%, respectively, which excluded heterogeneity in the studies (Figure 5B).
Doses of narcotics: Four studies (768 patients) provided data on doses of narcotics for children. Pooling the results indicated that SILS-A had similar results to C-LA, [WMD -0.25 (95%CI: -0.50-0), P > 0.05]. The χ2 and I2 were 14.25 (P = 0.0003) and 79%, respectively, indicating heterogeneity among the studies (Figure 6).
The straightforward conclusion from the 16 included studies is that compared with C-LA, SILS-A has acceptable complications, similar recovery, and the same OR times for patients.
Arguments against the use SILS-A cite the lack of evidence regarding patient benefit over open surgery or CL-A. The potential requirement for advanced instrumentation may also translate into increased costs. In addition, the lack of pneumoperitoneum leaks, triangulation, and instrument “clashing” are perceived as real disadvantages of this procedure, thereby increasing its difficulty. From our study, the umbilical incision permitted only one laparoscope and one instrument into the abdominal cavity concomitantly, which ensured less trauma than the C-LA. Coaxiality was not a significant problem, except for a few of patients in whom we adopted flexible and rotating instruments. Moreover, tilting the operating table enabled us to achieve adequate exposure and dissection for the majority of patients. However, ligation of the appendix was a restricted phase of the procedure. In children, the surgery space is smaller and the lack of ancillary equipment increasing the difficulty. This is why SILS-A requires a longer time than C-LA in children at present. However, future research could be oriented toward the development of a 5-mm-diameter clip applier or sealing of the appendiceal base using energy sources, which would resolve this difficulty.
With the emergence of natural orifice translumenal endoscopic surgery, the new transumbilical approach seems to reduce the trauma of surgical access, improving postoperative pain and patient cosmesis compared to the conventional laparoscopic approach. The cosmetic outcomes of SILS-A are expected to be better if the operation is performed through the umbilicus. This is because the surgical wound is hidden within the umbilicus, leaving no visible abdominal scars. From our study, SILS-A has the same of OR times, recovery and complications as C-LA; however, SILS-A has more advantages than C-LA.
The total complication rate of 8% after SILS-A in our series was close to the 9%-14% published in the current literature for C-LA[43,44]. Extraction of the appendix through the abdominal wall is generally performed with a protected method. In our series, the risk of surgical-site infection was similar to C-LA. Although more wound infections occurred in the SILS-A group, this difference did not reach statistical significance. To answer the question of whether the wound infection rate is indeed higher for single-incision compared to C-LA, a larger number of patients are needed.
There are conflicting results regarding doses of narcotics required comparing SILS-A with C-LA, with some studies reporting higher doses of narcotics required after SILS-A[34-37] and others showing no difference. Some scholars reported that in SILS-A, early pain was more severe than in a C-LA. This might be caused by the skin incision. Although the skin incision in the umbilical area is small, the actual length of the fascia incision is much longer, and through the small incision region, all the laparoscopic equipment is used together, which stimulates the incision. From our study, there is no different between SILS-A and C-LA in children.
Postsurgical complications in patients who underwent SILS-A were treated without special side effects or complications, except for wound problems. Thus, SILS-A appears to be safe. Implementation in the identified RCT’s showed a fairly low rate of complications in the SILS-A group. However, major complications were not reduced. More large studies, with more stringent quality criteria, may improve the statistical power and provide proof of reduced morbidities. There is a common perception that although patients are released earlier after SILS-A, there are more readmissions. With a a 90 d follow up period, this is unlikely, especially in children. Although not statistically significant, it seems that SILS-A does decrease morbidities. However, the available data does not provide proof that SILS-A is superior to the conventional technique and more evidence should be provided. In addition, the quality of future trials should be higher to adequately advocate using SILS-A as the gold standard.
There are limitations to this meta-analysis. First, the sample size of some of the studies was quite low, as was the number of studies included in our meta-analysis; this may have biased the results. Second, not all of the included trials were randomized, which caused a lack of the required details. Third, we did not compare improvements in other comorbidities following SILS-A and C-LA, and these factors may be important in assessing and recommending the procedure. SILS-A is a comparatively new procedure that has become popular in recent years; therefore, there is also concern about the long-term results. The follow-up periods in most reports were 3 or 6 mo, and the studies analyzed here provided relatively short-term findings. However, we believe that, with greater awareness and the increasing popularity of SILS-A, studies comparing the two approaches in large volumes with long-term follow-up will be published.
In conclusion, this meta-analysis demonstrated that the SILS-A procedure is associated with significantly less bleeding, while providing an improved cosmetic outcome despite a modest increase the ratio of conversion. SILS-A is a technically feasible and reliable approach with short-term results similar to those obtained with C-LA. Prospective randomized studies comparing the two approaches in large patient cohorts with long-term follow-up will be needed to confirm the results reported.
Single incision laparoscopic surgery for an appendectomy (SILS-A) is widely accepted and has become the best option for treatment of appendicitis. Compared with conventional laparoscopic appendectomy (C-LA), the safety and efficacy of SILS-A is not known.
Over the past three decades, many studies have assessed the performance of SILS-A. However, comparisons of SILS-A and C-LA for adults and children have not been published.
Based on this meta-analysis, single incision laparoscopic surgery does not increase the risk for an appendectomy. Similar associations were indicated in subgroup analyses of East Asian, Western, cohort, and high-quality studies. These findings were not presented clearly in previous systematic reviews.
Single incision laparoscopic surgery appears to be neither directly nor indirectly associated with the risk and pain of appendectomy. Further studies should seek to clarify this conclusion.
SILS-A is rapidly becoming the focal point of attraction for specialists worldwide. This article shows the advantages of the procedure for adults and children. This analysis has great practical value for clinicians.
P- Reviewer Wang DR S- Editor Wang JL L- Editor Stewart GJ E- Editor Ma S
| 1. | Semm K. Endoscopic intraabdominal surgery in gynecology. Wien Klin Wochenschr. 1983;95:353-367. [PubMed] |
| 2. | Saber AA, El-Ghazaly TH, Elian A. Single-incision transumbilical laparoscopic sleeve gastrectomy. J Laparoendosc Adv Surg Tech A. 2009;19:755-758, discussion 759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 3. | Nguyen NT, Reavis KM, Hinojosa MW, Smith BR, Wilson SE. Laparoscopic transumbilical sleeve gastrectomy without visible abdominal scars. Surg Obes Relat Dis. 2009;5:275-277. [PubMed] |
| 4. | Reavis KM, Hinojosa MW, Smith BR, Nguyen NT. Single-laparoscopic incision transabdominal surgery sleeve gastrectomy. Obes Surg. 2008;18:1492-1494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 136] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 5. | Saber AA, Elgamal MH, Itawi EA, Rao AJ. Single incision laparoscopic sleeve gastrectomy (SILS): a novel technique. Obes Surg. 2008;18:1338-1342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 167] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 6. | Saber AA, El-Ghazaly TH. Early experience with single incision transumbilical laparoscopic adjustable gastric banding using the SILS Port. Int J Surg. 2009;7:456-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Saber AA, El-Ghazaly TH. Early experience with single-access transumbilical adjustable laparoscopic gastric banding. Obes Surg. 2009;19:1442-1446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Teixeira J, McGill K, Binenbaum S, Forrester G. Laparoscopic single-site surgery for placement of an adjustable gastric band: initial experience. Surg Endosc. 2009;23:1409-1414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Teixeira J, McGill K, Koshy N, McGinty J, Todd G. Laparoscopic single-site surgery for placement of adjustable gastric band--a series of 22 cases. Surg Obes Relat Dis. 2010;6:41-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Tacchino RM, Greco F, Matera D. Laparoscopic gastric banding without visible scar: a short series with intraumbilical SILS. Obes Surg. 2010;20:236-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | D’Alessio A, Piro E, Tadini B, Beretta F. One-trocar transumbilical laparoscopic-assisted appendectomy in children: our experience. Eur J Pediatr Surg. 2002;12:24-27. [PubMed] |
| 12. | Rispoli G, Armellino MF, Esposito C. One-trocar appendectomy. Surg Endosc. 2002;16:833-835. [PubMed] |
| 13. | Ateş O, Hakgüder G, Olguner M, Akgür FM. Single-port laparoscopic appendectomy conducted intracorporeally with the aid of a transabdominal sling suture. J Pediatr Surg. 2007;42:1071-1074. [PubMed] |
| 14. | Varshney S, Sewkani A, Vyas S, Sharma S, Kapoor S, Naik S, Purohit D. Single-port transumbilical laparoscopic-assisted appendectomy. Indian J Gastroenterol. 2007;26:192. [PubMed] |
| 15. | Palanivelu C, Rajan PS, Rangarajan M, Parthasarathi R, Senthilnathan P, Praveenraj P. Transumbilical endoscopic appendectomy in humans: on the road to NOTES: a prospective study. J Laparoendosc Adv Surg Tech A. 2008;18:579-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Hodgett SE, Hernandez JM, Morton CA, Ross SB, Albrink M, Rosemurgy AS. Laparoendoscopic single site (LESS) cholecystectomy. J Gastrointest Surg. 2009;13:188-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 138] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 17. | Zhu JF, Hu H, Ma YZ, Xu MZ. Totally transumbilical endoscopic cholecystectomy without visible abdominal scar using improved instruments. Surg Endosc. 2009;23:1781-1784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Gumbs AA, Milone L, Sinha P, Bessler M. Totally transumbilical laparoscopic cholecystectomy. J Gastrointest Surg. 2009;13:533-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 127] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 19. | Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech A. 1999;9:361-364. [PubMed] |
| 20. | Bresadola F, Pasqualucci A, Donini A, Chiarandini P, Anania G, Terrosu G, Sistu MA, Pasetto A. Elective transumbilical compared with standard laparoscopic cholecystectomy. Eur J Surg. 1999;165:29-34. [PubMed] |
| 21. | Bucher P, Buchs N, Pugin F, Ostermann S, Morel P. Single port access laparoscopic cholecystectomy (with video): reply. World J Surg. 2011;35:1150-1151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 22. | Tacchino R, Greco F, Matera D. Single-incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc. 2009;23:896-899. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 242] [Cited by in RCA: 242] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 23. | Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy : scarless cholecystectomy. Surg Endosc. 2009;23:1393-1397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 177] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 24. | Romanelli JR, Mark L, Omotosho PA. Single port laparoscopic cholecystectomy with the TriPort system: a case report. Surg Innov. 2008;15:223-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 104] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 25. | Lowry PS, Moon TD, D’Alessandro A, Nakada SY. Symptomatic port-site hernia associated with a non-bladed trocar after laparoscopic live-donor nephrectomy. J Endourol. 2003;17:493-494. [PubMed] |
| 26. | Marcovici I. Significant abdominal wall hematoma from an umbilical port insertion. JSLS. 2001;5:293-295. [PubMed] |
| 27. | Lee YS, Kim JH, Moon EJ, Kim JJ, Lee KH, Oh SJ, Park SM, Hong TH. Comparative study on surgical outcomes and operative costs of transumbilical single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy in adult patients. Surg Laparosc Endosc Percutan Tech. 2009;19:493-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 28. | Cho MS, Min BS, Hong YK, Lee WJ. Single-site versus conventional laparoscopic appendectomy: comparison of short-term operative outcomes. Surg Endosc. 2011;25:36-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 29. | Teoh AY, Chiu PW, Wong TC, Wong SK, Lai PB, Ng EK. A case-controlled comparison of single-site access versus conventional three-port laparoscopic appendectomy. Surg Endosc. 2011;25:1415-1419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 30. | Park J, Kwak H, Kim SG, Lee S. Single-port laparoscopic appendectomy: comparison with conventional laparoscopic appendectomy. J Laparoendosc Adv Surg Tech A. 2012;22:142-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 31. | Kim HO, Yoo CH, Lee SR, Son BH, Park YL, Shin JH, Kim H, Han WK. Pain after laparoscopic appendectomy: a comparison of transumbilical single-port and conventional laparoscopic surgery. J Korean Surg Soc. 2012;82:172-178. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 32. | Vilallonga R, Barbaros U, Nada A, Sümer A, Demirel T, Fort JM, González O, Armengol M. Single-port transumbilical laparoscopic appendectomy: a preliminary multicentric comparative study in 87 patients with acute appendicitis. Minim Invasive Surg. 2012;2012:492409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 33. | Perez EA, Piper H, Burkhalter LS, Fischer AC. Single-incision laparoscopic surgery in children: a randomized control trial of acute appendicitis. Surg Endosc. 2013;27:1367-1371. [PubMed] |
| 34. | Chandler NM, Danielson PD. Single-incision laparoscopic appendectomy vs multiport laparoscopic appendectomy in children: a retrospective comparison. J Pediatr Surg. 2010;45:2186-2190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 35. | Mayer S, Werner A, Wachowiak R, Buehligen U, Boehm R, Geyer C, Till H. Single-incision multiport laparoscopy does not cause more pain than conventional laparoscopy: a prospective evaluation in children undergoing appendectomy. J Laparoendosc Adv Surg Tech A. 2011;21:753-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 36. | St Peter SD, Adibe OO, Juang D, Sharp SW, Garey CL, Laituri CA, Murphy JP, Andrews WS, Sharp RJ, Snyder CL. Single incision versus standard 3-port laparoscopic appendectomy: a prospective randomized trial. Ann Surg. 2011;254:586-590. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 166] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 37. | Knott EM, Gasior AC, Holcomb GW, Ostlie DJ, St Peter SD. Impact of body habitus on single-site laparoscopic appendectomy for nonperforated appendicitis: subset analysis from a prospective, randomized trial. J Laparoendosc Adv Surg Tech A. 2012;22:404-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 38. | Kang DB, Lee SH, Lee SY, Oh JT, Park DE, Lee C, Choi DH, Park WC, Lee JK. Application of single incision laparoscopic surgery for appendectomy in children. J Korean Surg Soc. 2012;82:110-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 39. | Raakow R, Jacob DA. Initial experience in laparoscopic single-port appendectomy: a pilot study. Dig Surg. 2011;28:74-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 40. | Amos SE, Shuo-Dong W, Fan Y, Tian Y, Chen CC. Single-incision versus conventional three-incision laparoscopic appendectomy: a single centre experience. Surg Today. 2012;42:542-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 41. | Chow A, Purkayastha S, Nehme J, Darzi LA, Paraskeva P. Single incision laparoscopic surgery for appendicectomy: a retrospective comparative analysis. Surg Endosc. 2010;24:2567-2574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 58] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 42. | Kang KC, Lee SY, Kang DB, Kim SH, Oh JT, Choi DH, Park WC, Lee JK. Application of single incision laparoscopic surgery for appendectomies in patients with complicated appendicitis. J Korean Soc Coloproctol. 2010;26:388-394. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 43. | Meguerditchian AN, Prasil P, Cloutier R, Leclerc S, Péloquin J, Roy G. Laparoscopic appendectomy in children: A favorable alternative in simple and complicated appendicitis. J Pediatr Surg. 2002;37:695-698. [PubMed] |
| 44. | Fishman SJ, Pelosi L, Klavon SL, O’Rourke EJ. Perforated appendicitis: prospective outcome analysis for 150 children. J Pediatr Surg. 2000;35:923-926. [PubMed] |