Published online Jul 7, 2013. doi: 10.3748/wjg.v19.i25.3990
Revised: April 20, 2013
Accepted: May 8, 2013
Published online: July 7, 2013
Processing time: 161 Days and 10.7 Hours
AIM: To investigate the prevalence of psychiatric illness in association with functional gastrointestinal disorders using defecating proctography (DP) and validated questionnaires.
METHODS: We prospectively evaluated 45 subjects referred for DP using hospital anxiety and depression scale (HADS), state trait anxiety inventory (STAI), patient health questionnaire 15-item somatic symptom severity scale (PHQ-15), validated questionnaires for sexual or physical abuse; post-traumatic stress disorder questionnaire (PTSD) and ROME-III questionnaires for gastrointestinal complaints. DP results were considered negative if levator ani function was normal, rectoceles (if any) were < 4 cm and there was no evidence of intussusception, rectal prolapse, or other anatomic abnormality demonstrated. Subjects were subsequently divided into those with structural defects seen on DP (DP positive group) and those with a normal defecography study (DP negative group).
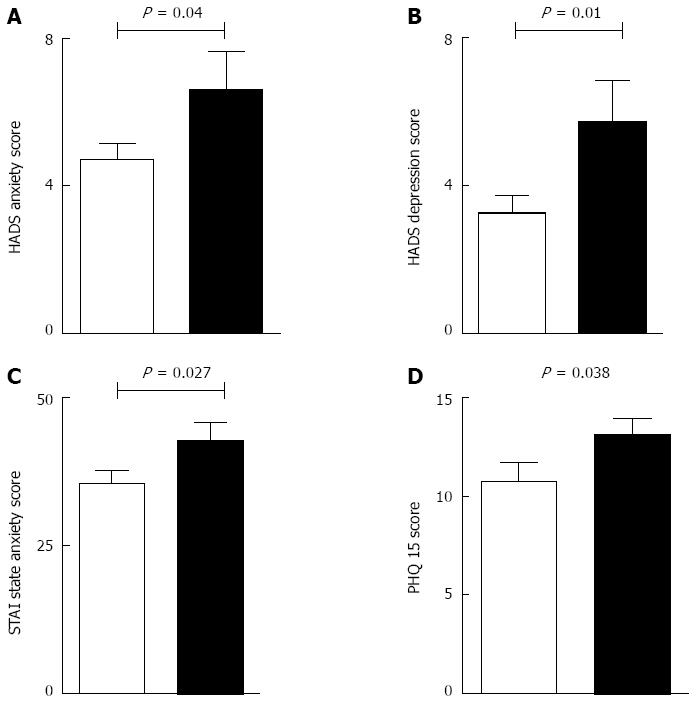
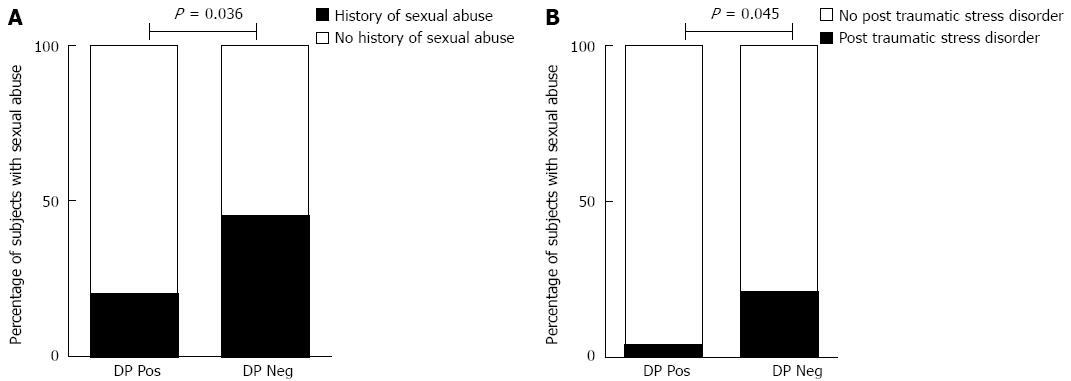
RESULTS: Forty five subjects were included in the study of which 20 subjects were classified as DP negative (44.4%). There was a striking prevalence of a history of sexual abuse in DP negative group compared to the DP positive group (n = 9, 5 respectively; P = 0.036). Further, subjects in the DP negative group scored significantly higher on the HADS anxiety (6.60 ± 1.00 vs 4.72 ± 0.40, P = 0.04) and depression scales (5.72 ± 1.00 vs 3.25 ± 0.46, P = 0.01). This correlated well with significantly higher scores on the STAI state anxiety scale (42.75 ± 3.16 vs 35.6 ± 2.00, P = 0.027), PHQ-15 questionnaire (13.15 ± 0.82 vs 10.76 ± 0.97, P = 0.038) and prevalence of PTSD (20% vs 4%, P = 0.045) among DP negative subjects. There was no difference between the groups in terms of STAI trait anxiety.
CONCLUSION: The findings of this prospective study demonstrate a significantly high degree of psychiatric ailments in patients with negative findings on DP who should be appropriately screened for a history of sexual abuse and symptoms of psychosocial distress.
Core tip: In this study, we used validated questionnaires in consort with defecating proctography and demonstrated that subjects undergoing defecating proctography who met ROME III criteria for functional constipation have a high prevalence of psychiatric disorders and a significant history of sexual abuse. We also found an association between post-traumatic stress disorder questionnaire, anxiety, history of sexual abuse and functional constipation. Taken together, these findings suggest that a very detailed history about psychiatric co-morbidities and traumatic experiences must be taken in selected patients complaining of constipation.
- Citation: Kashyap AS, Kohli DR, Raizon A, Olden KW. A prospective study evaluating emotional disturbance in subjects undergoing defecating proctography. World J Gastroenterol 2013; 19(25): 3990-3995
- URL: https://www.wjgnet.com/1007-9327/full/v19/i25/3990.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i25.3990
Patients with chronic gastrointestinal symptoms such as abdominal pain and constipation often display features suggestive of concomitant emotional disturbance[1]. Conversely, patients with a history of sexual or physical abuse have a high prevalence of gastrointestinal and genitourinary complaints[2].
There is evidence suggesting that patients with history of abuse and functional gastrointestinal disorders have a higher incidence of surgeries, lower quality of life and greater disability[3]. Given the lack of a surgically correctable etiology, surgical intervention may be inappropriate in these patients. In this context, we decided to evaluate patients with constipation, studying both anatomic and psychosocial variables using a variety of instruments.
We sought to assess the prevalence of abuse and psychiatric diagnoses in patients referred for defecating proctography (DP). Specifically, we sought to ascertain the prevalence of sexual abuse, physical abuse, anxiety, depression, somatization and post-traumatic stress disorder (PTSD) in subjects meeting criteria for functional constipation and without radiographic evidence of structural explanation for symptoms. We hypothesized that patients with no anatomic disorder of the pelvic floor evidenced by radiological parameters are likely to have a history of abuse and/or psychiatric diagnosis.
The purpose of the study was to use DP and a variety of validated questionnaires to assess the prevalence of psychiatric ailments in subjects with chronic constipation.
This prospective cohort study was undertaken at the Washington Hospital Center, a 926 bed tertiary care hospital in Washington DC. All subjects undergoing DP for the evaluation of lower gastrointestinal complaints were prospectively enrolled over 18 mo starting October 2010. Patients with obvious anatomical anomalies such as rectal prolapse, solitary rectal ulcers, fissures and fistulae were excluded.
At the time of enrollment, demographic information was recorded and each subject was assigned a unique identifying number. All other subject identifiers were removed. The study was approved by the institutional review board of Washington Hospital Center and all subjects gave written informed consent.
Immediately prior to undergoing the DP, all subjects were asked to complete a set of self-administered questionnaires.
All subjects answered a total of 7 self-administered validated questionnaires that assessed a history of sexual or physical abuse, generalized anxiety disorder (state and trait anxiety), PTSD, depression and somatoform disorders. Gastrointestinal symptoms were assessed using the ROME III criteria questionnaires that included the constipation module and irritable bowel syndrome module. All questionnaires were self-administered and met appropriate reliability and validity criteria. Further, each questionnaire was easily readable and understandable.
State-trait anxiety inventory: The state-trait anxiety inventory (STAI) is a self-administered test for evaluation of state and trait anxiety and has been used extensively in research and clinical practice. It has been translated into 30 languages and has since been extensively used and validated in the research literature[4]. For the purpose of our study the revised version of the test; ‘‘Form-Y’’ was used[5]. The STAI-Y is a self-administered test and takes 6-15 min to complete, depending on the subject’s level of education. The S-anxiety scale (STAI Form Y-1) consists of 20 statements that evaluate how the respondent feels ‘‘right now, at this moment’’ using a 4 point Likert scale. The T-anxiety scale (STAI Form Y-2) consists of 20 statements that evaluate how individuals ‘‘generally feel’’. A score of over 40 on the STAI Form Y-1 and STAI Form Y-2 was considered diagnostic of state of anxiety and trait anxiety respectively.
Screening questionnaire for sexual and physical abuse history: This is a self-report questionnaire developed by Drossman et al[6] and has been validated against a detailed psychological interview[7]. The questionnaire has two sections to identify sexual abuse and physical abuse as a child or adult respectively. For the purpose of our study, no distinction was made between abuse as an adult or child.
Hospital anxiety and depression scale: The hospital anxiety and depression scale (HADS) is a self-administered questionnaire to assess generalized anxiety or depression[8] and takes approximately 2-5 min to complete. It has been extensively validated in patients with gastrointestinal disorders[9] in the in-patient[5] as well as the out-patient setting[10]. Each item is answered by the patient on a four point scale (0-3) with possible scores ranging from 0-21 for anxiety and 0-21 for depression. Any score above 11 is indicative of abnormal levels of anxiety or depression, thus a positive screen for the appropriate disorder.
Screening for somatoform disorders: We used the patient health questionnaire (PHQ-15) to screen for somatoform disorders in our subjects. The PHQ-15 is a 15 item scale addressing somatic symptoms during a 2 wk period on a scale of 0-2 with a maximum score of 30[11] and has been validated among patients with gastrointestinal complaints[12]. We compared the scores of the subjects based on the findings of the DP.
PTSD: We used the 4 item screen for PTSD in primary care developed by Prins et al[13]. This validated screening questionnaire[14] uses a binary yes/no response to a specific experience and a score of 3 or greater on the scale was defined as a positive case of PTSD.
ROME III constipation module and ROME III irritable bowel syndrome module: The ROME III criteria were used to screen for irritable bowel syndrome (IBS) and constipation[15]. The ROME III criteria are a system used to classify functional gastrointestinal disorders and we used validated self-administered questionnaires that are freely available for download[16]. The ROME III criteria were used to rule out constipation predominant IBS as a cause of the patients symptoms and also to diagnose patients with true functional constipation.
Notably, all the questionnaires inquired about information which may have been potentially distressing to the subjects. Hence, one of the authors (Olden KW) who is a board-certified psychiatrist was available to the subjects in case emotional and mental distress was caused or detected by the protocol related questions. After completing the questionnaires, subjects underwent DP.
Defecating proctography was used to evaluate for anatomical defects that could explain the gastrointestinal symptoms in the subjects. Briefly, the study involved rectal administration of a radio-opaque semi-solid paste with the consistency of soft stool. The subject was then seated on a commode and made to excrete the material in a manner similar to defecation[17]. The radiological images taken during the evacuation process were interpreted by a radiologist who specialized in DP. The radiologist was blinded to the results of the psychosocial evaluation and did not interact with the subjects.
DP has been used extensively in patients with defecatory dysfunction, pelvic prolapse or puborectalis dysfunction[18-20] to visualize anatomic defects like internal or complete rectal prolapse, enterocele or rectocele. The quantification of the rectal evacuation is especially helpful in patients with pelvic floor dysfunction or dyssynergia and is recommended as a physiological means of assessing rectal dysfunction[21]. DP was considered “negative” for anatomical abnormalities if levator ani function was normal, rectoceles (if any) were < 4 cm[22] and there was no evidence of intussusception, rectal prolapse, or other anatomic abnormality demonstrated. Subjects were subsequently divided into those with structural defects seen on DP (DP positive group) and those with a normal defecography study (DP negative group). Responses to the questions were subsequently compared between the DP positive and the DP negative group.
Unpaired Student’s t test was used for analyzing demographic differences in demographic variables with continuous distribution while χ2 test was used for analyzing categorical variables using GraphPad Prism software (v 5.0a, GraphPad Prism Inc., San Diego, CA, United States). A P value of < 0.05 was considered significant. All data are presented as mean ± SE.
A total of 45 patients were included in the study and completed the psychosocial evaluation prior to undergoing the DP. Thirty seven (82%) of the total subjects were females (Table 1). Forty four subjects (97.7%) were referred for DP for evaluation of constipation. One subject was referred for possible anismus (pelvic floor dyssynergia).
| Variables | DP positive group (n = 25) | DP negative group (n = 20) | P value |
| Demographics | |||
| Males | 3 | 5 | > 0.050 |
| Age (yr) | 61.8 ± 2.8 | 58.1 ± 2.9 | > 0.050 |
| Assessment of psycho-social factors | |||
| Sexual abuse | 5 | 9 | 0.036 |
| Physical abuse | 1 | 2 | > 0.050 |
| Post traumatic stress disorder | 1 | 4 | 0.045 |
| STAI state anxiety | 35.60 ± 2.00 | 42.75 ± 3.16 | 0.027 |
| STAI trait anxiety | 35.08 ± 1.76 | 38.06 ± 2.42 | > 0.050 |
| HADS anxiety | 4.72 ± 0.40 | 6.60 ± 1.00 | 0.040 |
| HADS depression | 3.25 ± 0.46 | 5.72 ± 1.00 | 0.014 |
| PHQ-15 | 10.76 ± 0.97 | 13.15 ± 0.82 | 0.038 |
In 20 (44.4%) of the 45 subjects, the DP did not show any anatomical anomaly and these subjects were classified as DP negative (i.e., negative for anatomical abnormalities on DP). The remaining 25 patients were classified as DP positive (i.e., DP demonstrated anatomical abnormalities that could contribute to symptoms).
Subjects in the DP negative group had strikingly high scores on the HADS anxiety and depression questionnaires (P = 0.04 and P = 0.01) compared to subjects in the DP positive group (Figure 1A and B). This correlated well with the significantly higher score on the STAI state anxiety questionnaire among subjects in the DP negative (P = 0.027) compared to the DP positive group (Figure 1C). Further, subjects in the DP negative group reported significantly worse PHQ-15 scores compared to the DP positive group (P = 0.038, Figure 1D).
Notably, we found that a fair proportion of the subjects reported a history of sexual abuse. Nine of the 20 (45%) subjects in the DP negative group and 5 of the 25 (20%) subjects in the DP positive group reported a history of sexual abuse (P = 0.036, Figure 2A). This correlated well with a higher prevalence of PTSD among subjects in DP negative group (4 of 20 subjects, 20%) than the DP positive group (1 of 25 subjects, 4%; P = 0.04, Figure 2B).
There was no significant difference among the DP positive and DP negative groups in terms of STAI trait anxiety and prevalence of physical abuse. Further, there was no significant difference in the 2 groups in terms of prevalence of IBS or constipation assessed using the ROME III questionnaires. Of note, all subjects included in the study had complaints of constipation and the results of the prevalence confirm the presenting complaints.
In this study, we demonstrated that subjects undergoing DP who met ROME III criteria for functional constipation have a high prevalence of psychiatric disorders. Greater levels of state anxiety as well depression were found in the above mentioned population. We also found an association between PTSD, history of sexual abuse and functional constipation. Taken together, these findings suggest that a very detailed history about psychiatric co-morbidities and traumatic experiences must be taken in selected patients complaining of constipation.
We included subjects who were referred for DP as part of further work-up of constipation that was refractory to conservative management. It is pertinent to note that a majority of the referrals were from colo-rectal surgeons for pre-operative assessment. As the results of the study show, 44% of the patients (DP negative) did not have any surgically correctable cause and hence would not be appropriate candidates for surgical interventions.
Sexual abuse is very common among patients with functional disorders of the lower gastrointestinal tract[1] with one study showing prevalence of 40%. Further, abused patients were found to have constipation as the most common gastrointestinal complaint[23]. In our study, 14 subjects had a history of sexual abuse of which a majority had constipation without any anatomical explanation. The difference in the prevalence of sexual abuse between the 2 groups was statistically significant. Notably, patients in the DP negative group had a significantly higher prevalence of PTSD, a condition closely associated with sexual abuse. Since a history of sexual abuse is a strong predictor of multiple surgeries and poor surgical outcomes for slow-transit constipation[24], a careful history is essential in this patient population.
There is a strong association between psychological dysfunction and gastro-intestinal disorders for which various therapeutic paradigms have been found to be effective. Cognitive behavior therapy, psychodynamic psychotherapy and pharmacological agents including anti-depressants been shown to be efficacious in managing the gastrointestinal symptoms in selected patients[1]. However, there needs to be a greater emphasis on the detection of psychological disturbance and eliciting a detailed history in these patients.
A novel aspect of our study was the use of DP for the evaluation of constipation and classifying subjects with organic (DP positive) vs functional (DP negative) gastrointestinal disorders. DP has been used extensively for evaluation of patients with evacuatory dysfunction[25] and is often considered the gold standard for imaging in patients with defecation disorders, most notably rectocele, enterocele, anismus and perineal descent[26]. Patients in the DP negative group would likely not benefit from surgical interventions given the functional nature of the symptoms detected by DP.
The findings of this prospective study demonstrate a significantly high degree of anxiety, depression, somatization, PTSD and sexual abuse in subjects with negative findings on DP. Our study confirms that psychological ailments can impact the lower gastrointestinal tract and is especially associated with constipation. We recommend that patients with refractory constipation and features suggestive of psychological ailment/abuse[3] should be appropriately screened for the aforementioned disorders.
Functional constipation is a common gastrointestinal ailment and is often associated with emotional disturbance. Defecating proctography (DP) is a radiological tool to visualize anatomical causes leading to gastrointestinal symptoms. This study assessed the prevalence of psychiatric ailments in patients with gastrointestinal symptoms who had been referred for defecating proctography.
This study uses a novel approach of combining a radiological tool (DP) and multiple validated psychiatric instruments to assess the prevalence of psychiatric ailments causing gastrointestinal manifestations.
The study demonstrates that a significant proportion of subjects undergoing DP and met ROME III criteria for functional constipation have psychiatric ailments. Further, there is an association between functional constipation and a history of sexual abuse.
It is suggested that a very detailed history about psychiatric co-morbidities and traumatic experiences must be taken in selected patients complaining of constipation. Further large scale studies are warranted to explore these associations.
Defecating proctography is a radiological study that requires a subject to excrete a rectally administered contrast to visualize anatomical defects pertinent to rectal evacuation.
The authors demonstrated a prospective study evaluating emotional disturbance in subjects undergoing defecating proctography. In my opinion, such a prospective study will give us more important information in this field.
P- Reviewers Naito Y, Tang W S- Editor Gou SX L- Editor A E- Editor Zhang DN
| 1. | Olden KW, Drossman DA. Psychologic and psychiatric aspects of gastrointestinal disease. Med Clin North Am. 2000;84:1313-1327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 2. | Hartono JL, Mahadeva S, Goh KL. Anxiety and depression in various functional gastrointestinal disorders: do differences exist? J Dig Dis. 2012;13:252-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 3. | Drossman DA, Leserman J, Nachman G, Li ZM, Gluck H, Toomey TC, Mitchell CM. Sexual and physical abuse in women with functional or organic gastrointestinal disorders. Ann Intern Med. 1990;113:828-833. [PubMed] |
| 4. | Spielberger CD. The State Trait anxiety inventory: A Comprehensive Bibliography. CA: Consulting Psychologists Press 1983; . |
| 5. | Bal BS, Crowell MD, Kohli DR, Menendez J, Rashti F, Kumar AS, Olden KW. What factors are associated with the difficult-to-sedate endoscopy patient? Dig Dis Sci. 2012;57:2527-2534. [PubMed] |
| 6. | Drossman DA, Talley NJ, Leserman J, Olden KW, Barreiro MA. Sexual and physical abuse and gastrointestinal illness. Review and recommendations. Ann Intern Med. 1995;123:782-794. [PubMed] |
| 7. | Leserman J, Drossman DA, Li Z. The reliability and validity of a sexual and physical abuse history questionnaire in female patients with gastrointestinal disorders. Behav Med. 1995;21:141-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 112] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361-370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28548] [Cited by in RCA: 31826] [Article Influence: 757.8] [Reference Citation Analysis (0)] |
| 9. | Bryant RV, van Langenberg DR, Holtmann GJ, Andrews JM. Functional gastrointestinal disorders in inflammatory bowel disease: impact on quality of life and psychological status. J Gastroenterol Hepatol. 2011;26:916-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (1)] |
| 10. | Higashi A, Yashiro H, Kiyota K, Inokuchi H, Hatta H, Fujita K, Watanabe Y, Kawai K. Validation of the hospital anxiety and depression scale in a gastro-intestinal clinic. Nihon Shokakibyo Gakkai Zasshi. 1996;93:884-892. [PubMed] |
| 11. | Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64:258-266. [PubMed] |
| 12. | Mussell M, Kroenke K, Spitzer RL, Williams JB, Herzog W, Löwe B. Gastrointestinal symptoms in primary care: prevalence and association with depression and anxiety. J Psychosom Res. 2008;64:605-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 110] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 13. | Prins A, Ouimette P, Kimerling R, Camerond RP, Hugelshofer DS, Shaw-Hegwer J, Thrailkill A, Gusman FD, Sheikh JI. The primary care PTSD screen (PC-PTSD): development and operating characteristics. Inter J Psychiatry Clin Pract. 2004;9:9-14. [RCA] [DOI] [Full Text] [Cited by in Crossref: 777] [Cited by in RCA: 783] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 14. | Ouimette P, Wade M, Prins A, Schohn M. Identifying PTSD in primary care: comparison of the Primary Care-PTSD screen (PC-PTSD) and the General Health Questionnaire-12 (GHQ). J Anxiety Disord. 2008;22:337-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 101] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 15. | Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006;130:1377-1390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1467] [Cited by in RCA: 1479] [Article Influence: 77.8] [Reference Citation Analysis (0)] |
| 16. | Available from: http: //www.romecriteria.org/assets/pdf/19_RomeIII_apA_885-898.pdf. |
| 17. | Mahieu P, Pringot J, Bodart P. Defecography: II. Contribution to the diagnosis of defecation disorders. Gastrointest Radiol. 1984;9:253-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 218] [Cited by in RCA: 158] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 18. | Thompson JR, Chen AH, Pettit PD, Bridges MD. Incidence of occult rectal prolapse in patients with clinical rectoceles and defecatory dysfunction. Am J Obstet Gynecol. 2002;187:1494-1499; discussion 1499-1500. [PubMed] |
| 19. | Kelvin FM, Maglinte DD, Hornback JA, Benson JT. Pelvic prolapse: assessment with evacuation proctography (defecography). Radiology. 1992;184:547-551. [PubMed] |
| 20. | Eltringham MT, Khan U, Bain IM, Wooff DA, Mackie A, Jefferson E, Yiannakou Y. Functional defecation disorder as a clinical subgroup of chronic constipation: analysis of symptoms and physiological parameters. Scand J Gastroenterol. 2008;43:262-269. [PubMed] |
| 22. | Diamant NE, Kamm MA, Wald A, Whitehead WE. AGA technical review on anorectal testing techniques. Gastroenterology. 1999;116:735-760. [PubMed] |
| 23. | Leroi AM, Bernier C, Watier A, Hémond M, Goupil G, Black R, Denis P, Devroede G. Prevalence of sexual abuse among patients with functional disorders of the lower gastrointestinal tract. Int J Colorectal Dis. 1995;10:200-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 73] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 24. | O’Brien S, Hyman N, Osler T, Rabinowitz T. Sexual abuse: a strong predictor of outcomes after colectomy for slow-transit constipation. Dis Colon Rectum. 2009;52:1844-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 25. | Beer-Gabel M, Teshler M, Schechtman E, Zbar AP. Dynamic transperineal ultrasound vs. defecography in patients with evacuatory difficulty: a pilot study. Int J Colorectal Dis. 2004;19:60-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 81] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Perniola G, Shek C, Chong CC, Chew S, Cartmill J, Dietz HP. Defecation proctography and translabial ultrasound in the investigation of defecatory disorders. Ultrasound Obstet Gynecol. 2008;31:567-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 86] [Article Influence: 5.1] [Reference Citation Analysis (0)] |