Published online Jun 28, 2013. doi: 10.3748/wjg.v19.i24.3866
Revised: December 20, 2012
Accepted: February 7, 2013
Published online: June 28, 2013
Processing time: 209 Days and 0.7 Hours
AIM: To identify demographic and clinical factors associated with disabling Crohn’s disease (CD).
METHODS: A systematic review and meta-analysis of observational studies, focusing on the factors that can predict the prognosis of different outcomes of CD was undertaken. PubMed, ISI Web of Knowledge and Scopus were searched to identify studies investigating the above mentioned factors in adult patients with CD. Studies were eligible for inclusion if they describe prognostic factors in CD, with inclusion and exclusion criteria defined as follows. Studies with adult patients and CD, written in English and studying association between clinical factors and at least one prognosis outcome were included. Meta-analysis of effects was undertaken for the disabling disease outcome, using odds ratio (OR) to assess the effect of the different factors in the outcome. The statistical method used was Mantel-Haenszel for fixed effects. The 16-item quality assessment tool (QATSDD) was used to assess the quality of the studies (range: 0-42).
RESULTS: Of the 913 papers initially selected, sixty studies were reviewed and three were included in the systematic review and meta-analysis. The global QATSDD scores of papers were 18, 21 and 22. Of a total of 1961 patients enrolled, 1332 (78%) were classified with disabling disease five years after diagnosis. In two studies, age at diagnosis was a factor associated with disabling disease five years after diagnosis. Individuals under 40 years old had a higher risk of developing disabling disease. In two studies, patients who were treated with corticosteroids on the first flare developed disabling disease five years after diagnosis. Further, perianal disease was found to be relevant in all of the studies at two and five years after diagnosis. Finally, one study showed localization as a factor associated with disabling disease five years after diagnosis, with L3 being a higher risk factor. This meta-analysis showed a significantly higher risk of developing disabling disease at five years after initial diagnosis among patients younger than 40 years of age (OR = 2.47, 95%CI: 1.74-3.51), with initial steroid treatment for first flare (OR = 2.42, 95%CI: 1.87-3.11) and with perianal disease (OR = 2.00, 95%CI: 1.41-2.85).
CONCLUSION: Age at diagnosis, perianal disease, initial use of steroids and localization seem to be independent prognostic factors of disabling disease.
- Citation: Dias CC, Rodrigues PP, Costa-Pereira AD, Magro F. Clinical prognostic factors for disabling Crohn's disease: A systematic review and meta-analysis. World J Gastroenterol 2013; 19(24): 3866-3871
- URL: https://www.wjgnet.com/1007-9327/full/v19/i24/3866.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i24.3866
Crohn’s disease (CD) occurs in equal proportion in both genders and its incidence has been growing worldwide in the last decades[1]. CD is a disabling disease affecting psychological, familial, and social dimensions of life[2]. Therefore, the need to develop a specific instrument able to evaluate disabilities and identify specific factors as predictors is paramount. This is particularly true since in the last decades the medical treatment options have been dramatically changed. Other strategies are now approaching, namely accelerate step-up and top-down treatment[3]. The top-down strategy is based on the very early use of intensive therapy (immunosuppressants and/or biologics) to maintain a good quality of life from the first flare-up of the disease and prevent any irreversible consequences[3]. Therefore, it is now crucial to identify simple clinical criteria at diagnosis to predict CD outcome. This work aims to systematically review the evidence with respect to predictive clinical prognostic factors for CD.
A systematic review and meta-analysis of observational studies focusing on the factors that can predict the prognosis of different outcomes of CD was undertaken. The methodology included the definition of eligibility criteria, search strategies, study selection and characteristics, outcome measures, quantitative data synthesis and sensitivity analysis, methodological quality of studies, and statistical data analysis.
Studies that described prognostic factors in CD were eligible for inclusion. The criteria for inclusion were studies with adult patients and CD written in English and studying association between clinical factors and disabling disease. Studies not in English, without available abstract, with genetic or serologic factors, biomarker studies, or those addressing diagnosis or quality of life were excluded.
The main method to search for the eligible articles was a broad literature search using PubMed with the following keywords and MeSH terms: “crohn disease”[MeSH Terms] OR “crohn”[All Fields] AND predictor [All Fields] OR predictors [All Fields] OR predict [All Fields] OR “prognostic factor” [All Fields] OR “prognostic factors” [All Fields]. Literature searches were also undertaken in Scopus database and ISI Web of Knowledge using the same search keywords: crohn disease AND (predictors OR predict OR prognostic factors).
The studies were screened and selected by two reviewers. First, all titles and abstracts were read and the inclusion and exclusion criteria were applied. Second, the reviewers read the full text of all papers considered for inclusion after abstract selection, again applying the inclusion and exclusion criteria.
The following properties of each study were recorded: total number of patients, prognostic variables, and percentage of patients with disabling disease.
The aim of the study is to assess prognostic factors to predict disabling CD.
The 16-item quality assessment tool (QATSDD), developed by Higgins et al[4], was used to assess the quality of the included studies. This tool includes 16 items, scored between 0 and 3, and can be applied to different types of studies using different approaches. However, two of the items were not evaluated as they only address qualitative studies, hence we only considered a maximum score of 42.
Statistical evidence of effects is presented as described in the original studies. Meta-analysis of effects was undertaken for the disabling disease outcome using odds ratio (OR) to assess the effect of the different factors in the outcome. The statistical method used was Mantel-Haenszel for fixed effects. All included estimates are recomputed from original articles descriptions, potentially resulting in slightly different values. All reported P-values are 2-sided with a significance level of 5%. Statistical heterogeneity was assessed with the I2 statistic; values higher than 50% indicate a substantial level of heterogeneity[5]. RevMan v5.1 (The Nordic Cochrane Center, The Cochrane Collaboration, 2011) was used to calculate OR and 95%CI for disabling disease and to derived forest plots showing the results of individual studies and pooled analysis.
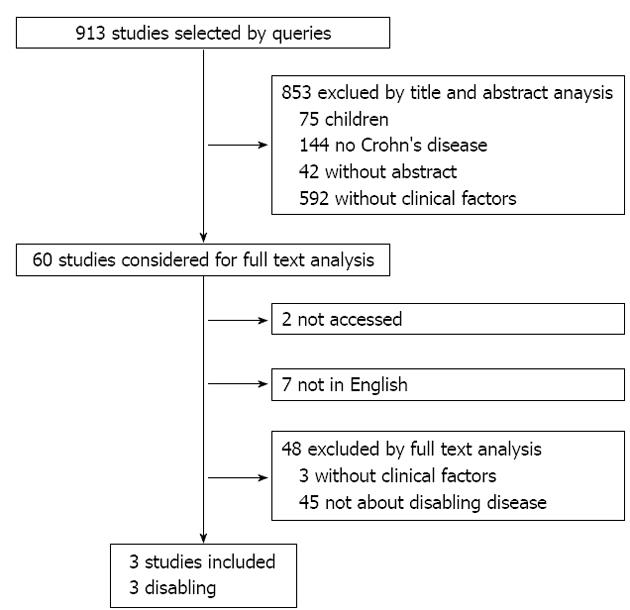
A total of 913 articles were identified using the search strategy. After reading all titles and abstracts, 853 articles were excluded (Figure 1). Sixty studies were reviewed in detail and three articles were included in the study. A new search of the literature focused on the outcome was made in order to find other papers that could have been missed by the generic search. The global QATSDD scores ranged between 18 and 22. The main characteristics of the studies are summarized in Table 1.
| Ref. | Country | Sample size (n) | Type of study | Disabling | Follow-up (yr) | Factor | QATSDD |
| Beaugerie et al[6] | France | 1123 | Retrospective | 85.2% | 5 | Age (under 40 yr) | 22 |
| Steroids for 1st flare | |||||||
| Perianal disease | |||||||
| Loly et al[7] | Belgium | 361 | Retrospective | 57.9% | 5 | Steroids for 1st flare | 18 |
| Perianal disease | |||||||
| L3 | |||||||
| Yang et al[8] | China | 207 | Retrospective | 71.0% | 2 | Steroids for 1st flare | 21 |
| Perianal disease | |||||||
| 80.2% | 5 | Age (under 40 yr) |
Beaugerie et al[6] and Loly et al[7] define disabling disease by the presence of at least one of the following criteria: two steroid courses required and/or steroid dependency; further hospitalization after diagnosis for flare up or complications of the disease; chronic symptoms (diarrhea with nocturnal and/or urgent stools, intensive abdominal pain due to intestinal obstruction, fever, fatigue attributable to the disease); joint pain; painful uveitis or pyoderma gangrenous for 12 mo within the five year study; immunosuppressive therapy and intestinal resection or surgical operation for perianal disease. Yang et al[8] defined CD as disabling if patients satisfy at least one of the following criteria: require two or more steroids courses and/or steroid dependency; need immunosuppressive therapy; intestinal resection or surgical operation for perianal disease and hospitalization after diagnosis for the treatment of acute exacerbation, or complication of the disease.
According to Beaugerie et al[6], 957 of 1123 patients (85.2%) were classified with disabling disease. With a sample of 361 patients, Loly et al[7] found 209 patients (57.9%) with disabling disease, while Yang et al[8] found 80.2% of 207 patients with disabling disease five years after diagnosis, and 71% of patients already had disabling disease two years after diagnosis.
Different factors were found that could predict disabling disease, namely age at diagnosis, use of steroids, perianal disease, and localization.
Beaugerie et al[6] found age at diagnosis as a factor associated with disabling disease. Patients less than 40 years old had a higher risk of developing disabling disease than older patients (OR = 2.1, 95%CI: 1.3-3.6) five years after the diagnosis. Yang et al[8] also showed that patients under 40 had a higher risk of developing disabling disease (OR = 3.56, 95%CI: 1.74-7.30).
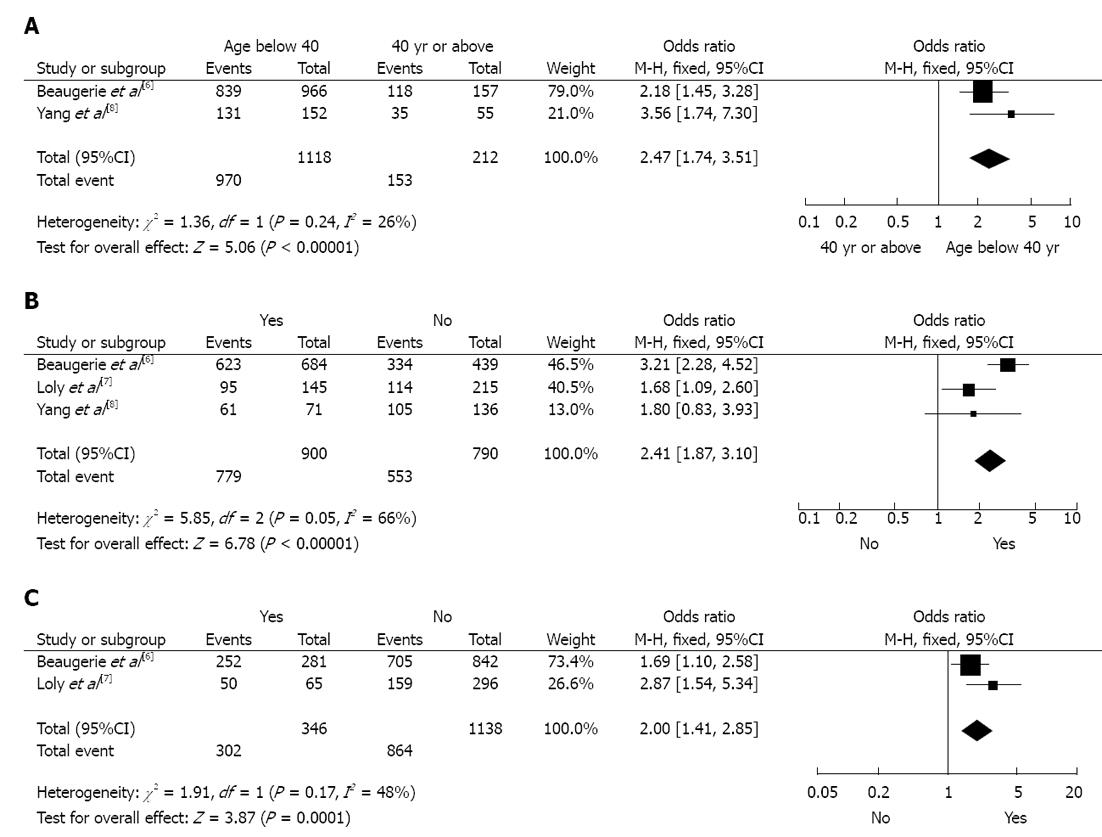
Results of studies comparing younger patients (under 40) with older patients (over 40) are shown in Figure 2A. A fixed effects model shows that younger patients had a higher risk of disabling disease five years after diagnosis (OR = 2.47, 95%CI: 1.74-3.51). There was no evidence of statistical heterogeneity among the studies (I2 = 26%).
Both Beaugerie et al[6] and Loly et al[7] show patients who had initial requirement of steroids for treating the first flare had a higher risk of developing disabling disease five years after diagnosis when compared to those who did not require treatment (OR = 3.1, 95%CI: 2.2-4.4 and OR = 1.7, 95%CI: 1.02-2.7, respectively). Yang et al[8] found similar results two years after diagnosis (OR = 2.142, 95%CI: 1.068-4.298).
Results of these different studies comparing patients with and without steroid requirement treatment are presented in Figure 2B. A fixed effects model shows that patients with steroid treatment had a higher risk of disabling disease five years after diagnosis (OR = 2.41, 95%CI: 1.87-3.10). Significant heterogeneity was found among the studies (I2 = 66%). Nevertheless, all studies found a higher risk of disabling disease for patients on steroids.
In all three studies, patients with perianal disease had a higher risk of developing disabling disease five years after diagnosis when compared to patients without perianal disease: Beaugerie et al[6] (OR = 1.8, 95%CI: 1.2-2.8), Loly et al[7] (OR = 2.6, 95%CI: 1.4-5.1), Yang et al[8] (two years after diagnosis) (OR = 5.433, 95%CI: 1.585-18.620).
The comparison between patients with and without perianal disease is shown in Figure 2C. A fixed effects model shows the presence of perianal disease as a high risk of disabling disease five years after diagnosis (OR = 2.00, 95%CI: 1.41-3.85). There was no evidence of statistical heterogeneity among the studies (I2 = 48%).
One study associated disabling disease to the localization of the disease. In this study, patients with L3 localization had a higher risk of developing disabling disease five years after the diagnosis (OR = 1.74, 95%CI: 1.06-2.8)[7].
CD is a chronic disease with no known medical or surgical cure, requiring several appointments and hospitalizations for those afflicted. There are several reasons stressing the importance of prognostic factors: (1) Recent available drugs, namely anti-tumour necrosis factor (TNF), having the potential of inducting mucosal healing and prolonged clinical remission; (2) Mucosal healing has been considered a therapeutic goal; and (3) Early therapeutic interventions are followed by a better outcome. Therefore, it is imperative that therapeutic options are optimized.
The present systematic review and meta-analysis presented some of the factors that could help clinicians identify risk groups for disabling CD. Age, perianal disease, the use of steroids and localization were all associated with disabling disease. Although other markers can help clinicians to predict disease course of CD, namely genetic, serologic and endoscopic findings, we limited this meta-analysis to demographic and clinical characteristics due to feasibility to apply at diagnosis at the bedside.
Three studies address disabling disease and used similar definitions, although in Yang et al[8] the presence of chronic symptoms like diarrhea, fever, fatigue, was not considered. All studies were retrospective and the number of patients in each study ranged from 207 to 1123[6,8]. It was clear that a large number of patients had disabling disease (range: 59%-81%), which gives an indication of the severity of the disease. Moreover, the study with the highest percentage of disabling disease included the least amount of defining characteristics[8]. Our meta-analysis showed that patients under 40 years old and patients with an initial requirement of steroids, or patients with perianal disease had a higher risk of having disabling disease five years following initial diagnosis. These results are in line with the three studies used in the meta-analysis[6-8]. Although the definition of disabling disease in Yang et al[8] is slightly different, this study had a lower weight in the final result of the meta-analysis, hence limiting the possible bias. Even though the effect of age at diagnosis was clear in the meta-analysis; further studies are necessary to better assess relative CD risk, including an evaluation of more patients diagnosed after the age threshold. We call into question some of the recent points included in disability definition, namely steroids following the first flare, the need for immunosuppressants, and surgery. The percentage of patients treated with steroids in the first flare (65%) in Beaugerie et al[6] was very similar to the percentage of patients who received steroids within in the first year of disease in the North-European population-based study, however this only reflects the step-up strategy, and the population on immunosuppressants was very low[9]. Markowitz et al[10] showed children requiring steroids for the treatment of the first flare-up that a very early use of 6-Mercaptopurine was associated with steroid sparing and a more favorable clinical outcome in the 18-mo period following diagnosis. Similar results were observed in those treated with anti-TNF in the first two years of disease[11]. Finally, the role of early surgery in limiting ileal disease with regard to CD prognosis is also debatable. In conclusion, the risk factors analyzed in this meta-analysis should be considered when new scores or approaches are taken concerning risk factors in CD outcome, particularly when more early therapeutic approaches are imminent.
The QATSDD scale, developed by Sirriyeh et al[5], allows the comparison of the quality of the included papers even when their designs are different. The included papers consistently presented low quality scores, especially considering the representativeness of the sample and the absence of a critical discussion of strengths and limitations.
The results of this study may need further confirmation due to the small number of reviewed studies and their low quality (maximum QATSDD score of 22 out of 42). Nevertheless, this work presents a step-forward in the definition of clinical predictors for disabling CD, exposing their relevance and impact in disease prognosis.
In summary, this review and meta-analysis showed that age, perianal disease and the use of steroids are associated with disabling disease. The use of these factors in building predictive models for CD prognosis could enhance the initial clinical approach, and therefore improve the clinical outcome of patients with severe disease. However, more elaborate and precise definitions of disabling and severe disease are needed.
Crohn’s disease (CD) occurs in equal proportion in both genders and its incidence has been growing worldwide in the last decades. CD is a disabling disease affecting psychological, familial, and social dimensions of life. Therefore, the need to develop a specific instrument able to evaluate disabilities and identify specific factors as predictors is paramount.
The top-down strategy is based on the very early use of intensive therapy (immunosuppressants and/or biologics) to maintain a good quality of life from the first flare-up of the disease and prevent any irreversible consequences. Therefore, it is now crucial to identify simple clinical criteria at diagnosis to predict CD outcome.
This work aims to systematically review the evidence with respect to predictive clinical prognostic factors for CD.
This review and meta-analysis showed that age, perianal disease and the use of steroids are associated with disabling disease. The use of these factors in building predictive models for CD prognosis could enhance the initial clinical approach, and therefore improve the clinical outcome of patients with severe disease. However, more elaborate and precise definitions of disabling and severe disease are needed.
It is one of the first work searching the role of CD in disability of the patient. The authors performed an extensive review of multiple manuscript related with the topic. The manuscript is very well prepared and written and can be accepted for publication.
P- Reviewers Perakath B, Rodriguez DC S- Editor Gou SX L- Editor A E- Editor Xiong L
| 1. | Peyrin-Biroulet L, Loftus EV, Colombel JF, Sandborn WJ. The natural history of adult Crohn’s disease in population-based cohorts. Am J Gastroenterol. 2010;105:289-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 654] [Cited by in RCA: 755] [Article Influence: 50.3] [Reference Citation Analysis (0)] |
| 2. | Casellas F, López-Vivancos J, Vergara M, Malagelada J. Impact of inflammatory bowel disease on health-related quality of life. Dig Dis. 1999;17:208-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 75] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Devlin SM, Panaccione R. Evolving inflammatory bowel disease treatment paradigms: top-down versus step-up. Med Clin North Am. 2010;94:1-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-560. [PubMed] |
| 5. | Sirriyeh R, Lawton R, Gardner P, Armitage G. Reviewing studies with diverse designs: the development and evaluation of a new tool. J Eval Clin Pract. 2012;18:746-752. [PubMed] |
| 6. | Beaugerie L, Seksik P, Nion-Larmurier I, Gendre JP, Cosnes J. Predictors of Crohn’s disease. Gastroenterology. 2006;130:650-656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 630] [Cited by in RCA: 639] [Article Influence: 33.6] [Reference Citation Analysis (0)] |
| 7. | Loly C, Belaiche J, Louis E. Predictors of severe Crohn’s disease. Scand J Gastroenterol. 2008;43:948-954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 212] [Cited by in RCA: 220] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 8. | Yang CH, Ding J, Gao Y, Chen X, Yang ZB, Xiao SD. Risk factors that predict the requirement of aggressive therapy among Chinese patients with Crohn’s disease. J Dig Dis. 2011;12:99-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Munkholm P, Langholz E, Davidsen M, Binder V. Frequency of glucocorticoid resistance and dependency in Crohn’s disease. Gut. 1994;35:360-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 487] [Cited by in RCA: 431] [Article Influence: 13.9] [Reference Citation Analysis (0)] |
| 10. | Markowitz J, Grancher K, Kohn N, Lesser M, Daum F. A multicenter trial of 6-mercaptopurine and prednisone in children with newly diagnosed Crohn’s disease. Gastroenterology. 2000;119:895-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 562] [Cited by in RCA: 524] [Article Influence: 21.0] [Reference Citation Analysis (0)] |
| 11. | Feagan BG, Panaccione R, Sandborn WJ, D’Haens GR, Schreiber S, Rutgeerts PJ, Loftus EV, Lomax KG, Yu AP, Wu EQ. Effects of adalimumab therapy on incidence of hospitalization and surgery in Crohn’s disease: results from the CHARM study. Gastroenterology. 2008;135:1493-1499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 280] [Cited by in RCA: 288] [Article Influence: 16.9] [Reference Citation Analysis (0)] |