Published online Apr 7, 2013. doi: 10.3748/wjg.v19.i13.2126
Revised: March 2, 2013
Accepted: March 7, 2013
Published online: April 7, 2013
Processing time: 69 Days and 4.2 Hours
A hemocholecyst (HC) is a clot-filled gallbladder caused by bleeding into its lumen. Obstructive jaundice caused by the compression of HC to the hilar biliary tract is likely to be misdiagnosed as cholangiocarcinoma and is extremely rare. We herein report a case of obstructive jaundice and melena caused by HC. A 57-year-old male patient presented with right upper quadrant pain associated with icteric sclera and melena was suspiciously diagnosed as having malignant cholangiocarcinmoa by abdominal ultrasonography, computed tomography and magnetic resonance imaging. Laparotomy found a hematoma in the gallbladder. The hematoma spread to the left hepatic lobe forming an exogenous mass which compressed the hilar biliary tract. Radical cholecystectomy and bile duct exploration with T-tube drainage were performed. Histopathological examination revealed massive necrosis of the gallbladder mucosa with inflammatory cells infiltration as well as intraluminal hematoma formation. One month after operation, a T-tube cholangiography revealed a normal biliary tree. We suggest that HC should be considered in patients with obstructive jaundice and melena after common causes are ruled out.
- Citation: Fan Y, Wu SD, Kong J. Obstructive jaundice and melena caused by hemocholecyst: A case report. World J Gastroenterol 2013; 19(13): 2126-2128
- URL: https://www.wjgnet.com/1007-9327/full/v19/i13/2126.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i13.2126
A hemocholecyst (HC) is a clot-filled gallbladder caused by bleeding into its lumen. As a cause of hemobilia, HC is rarely reported with a variety of etiology including trauma[1], iatrogenic manipulation[2,3], gallbladder tumor[4,5], cholecystitis[6] and ruptured cystic artery aneurysm[7]. Hematological disorders such as hemophilia are also implicated in some cases[8,9]. Here, we report a rare case of obstructive jaundice and melena caused by HC. Though abdominal ultrasonography (US), computed tomography (CT) and magnetic resonance imaging (MRI) have proved to be highly accurate methods for evaluating gallbladder disorders, a definitive diagnosis cannot be established preoperatively. In addition, our patient had not experienced abdominal trauma, and had no history of obvious bleeding disorders.
A 57-year-old man presented at our emergency department with the right upper quadrant pain with icteric sclera for seven days, and melena for two days. The pain was dull in character, sudden in onset, and did not radiate to the back. It was not aggravated by food intake or related to movement. The patient had no history of abdominal trauma or peptic ulcer with bleeding. On admission, the patient was febrile with right upper quadrant tenderness, rebound tenderness, slight muscular rigidity and a positive Murphy’s sign. Laboratory examinations revealed abnormal hepatic enzyme levels: aspartate aminotransferase 145 U/L (normal, 5-34 U/L), alanine aminotransferase 95 U/L (normal, 0-40 U/L), increased total bilirubin 135.5 μmol/L (normal, 3.4-20.5 μmol/L) and increased alkaline phosphatase 240 U/L (normal, 40-150 U/L). The patient had leukocytosis (14 200/μL), with decreased hemogram (hemoglobin, 8.9 g/dL; hematocrit, 32.7%), but normal platelet count (242 × 103/μL). However, prothrombin time and partial thromboplastin time were both normal. Serum amylase and lipase levels were also within normal limits. Tumor markers including alpha foetoprotein, carcinoembryonic antigen and carbohydrate antigen were also negative.
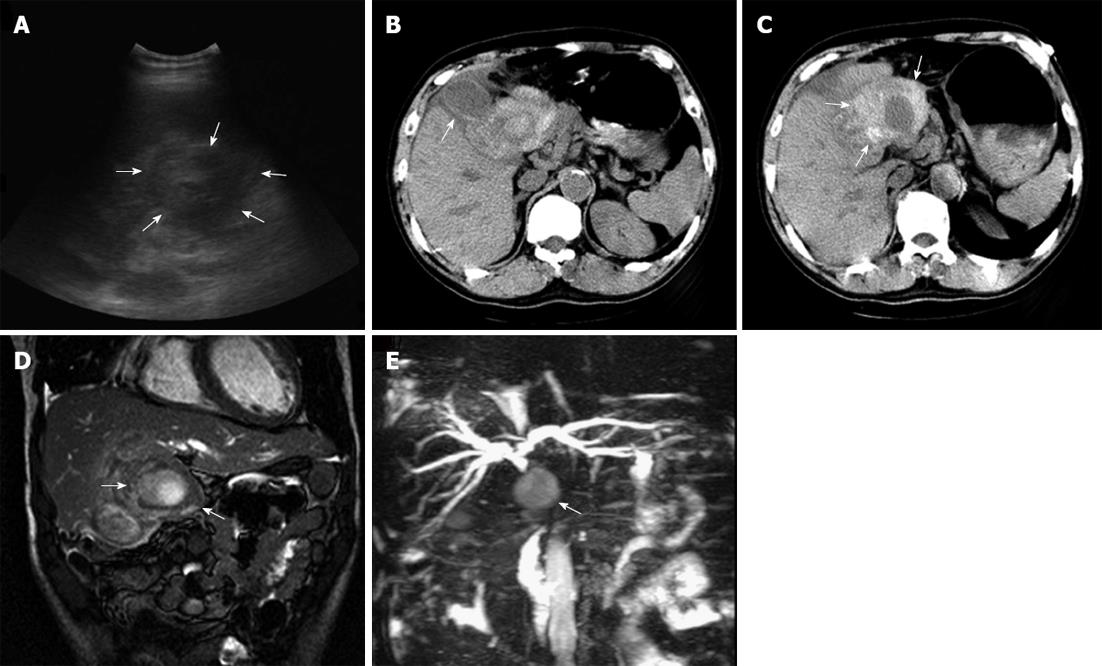
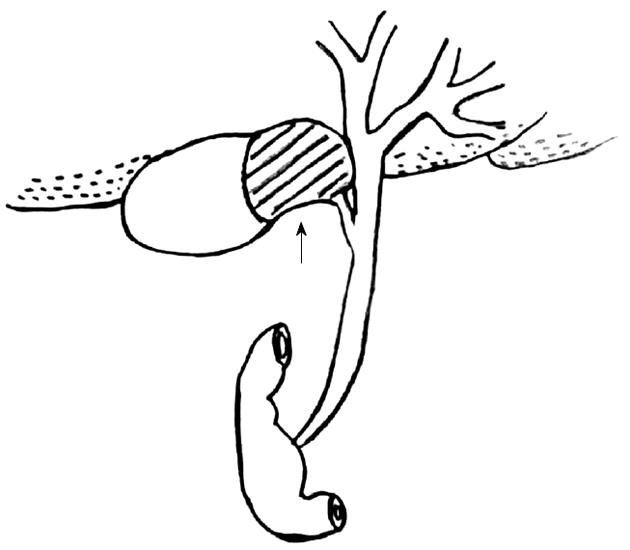
Ultrasound of the abdomen revealed a mass with heterogenous echo at the gallbladder region (Figure 1A). CT showed thickening of the gallbladder fundus and body wall (Figure 1B) and a mass with high-density shadow located at the gallbladder neck without clear demarcation from the left hepatic lobe (Figure 1C). MRI showed a mass located at the gallbladder neck and left hepatic lobe (Figure 1D) with slight dilation of intrahepatic ducts and an obscure image of hilar biliary tract (Figure 1E). Gastrointestinal tract endoscopic study found no common causes of melena such as malignancy, ischemic colitis, etc. Initial diagnosis of malignant cholangiocarcinoma was made. He was treated with antibiotics, hemostatics and fluid supplement before transferred to the operating room for exploratory laparotomy. On exploration, a hematoma was found in the neck-side lumen of the gallbladder. The hematoma spread to the left hepatic lobe forming an exogenous mass which compressed the hilar biliary tract (Figure 2). Cholecystectomy and bile duct exploration with T tube drainage were performed. Histopathology revealed massive necrosis of the gallbladder mucosa with inflammatory cell infiltration as well as intraluminal hematoma formation. The patient was discharged on the 7th postoperative day in a stable condition. One month after operation, a T-tube cholangiography revealed a normal biliary tree (Figure 3).
Hemorrhagic cholecystitis is an extremely rare cause of hemobilia. Up to now, only three cases of hemobilia which was clearly attributable to acalculous cholecystitis, have been reported by Shah et al[10] and Ellington et al[11]. Our patient is the 4th reported case. We think that acalculous cholecystitis may cause hemorrhage through mucosal necrosis and ulceration with erosion into one or more vessels in this patient.
Hemobilia classically presents as biliary colic pain, jaundice and gastrointestinal tract bleeding. However, the clinical presentation varies. Depending on the amount and rate of bleeding, blood may clot in various locations. If the blood does not clot in the biliary tract, hematemesis or melena may occur. If blood clots within the bile duct, it may cause obstructive jaundice or pancreatitis. It was unusual in this patient that jaundice was not caused by blood clots within the bile duct, but resulted from the compression of the HC to the hilar biliary tract.
Our patient did not present with melena as a primary symptom. He had symptoms, signs, and laboratory studies that suggested choledocholithiasis and cholangitis. He developed melena only on the 5th day. The preoperative diagnosis of gallbladder hematoma is very difficult, or even impossible, to make in the absence of a history of trauma or bleeding diatheses. Preoperative US, CT and MRI are main techniques for diagnosing gallbladder diseases. Although the US and CT findings of gallbladder hematoma might not be exactly the same as those of gallbladder carcinoma or invasive hilar cholangiocarcinoma, a definitive diagnosis often cannot be made confidently. MRI is useful for differential diagnosis. It was reported that hematomas are similar in signal intensity to skeletal muscle on T1-weighted imaging, with conversion to marked hypointensity on T2-weighted imaging[8]. The hematoma in our patient was not confined to the gallbladder but spread to the left hepatic lobe forming an exogenous mass which compressed the hilar biliary tract, thus making the diagnosis even more difficult. All preoperative imaging studies gave an impression of a highly suspected cholangiocarcinoma with invasion to the gallbladder neck and left hepatic lobe. In our case, cholangiocarcinoma could not be ruled out. Therefore, the correct diagnosis could only be made through dynamic image observation, aggregate analysis and resolute operation exploration.
In conclusion, we suggest that HC should be considered in patients with obstructive jaundice and melena after common causes are ruled out.
P- Reviewer Kai K S- Editor Gou SX L- Editor A E- Editor Xiong L
| 1. | Shin KY, Heo J, Kim JY, Lee SJ, Jang SY, Park SY, Jung MK, Cho CM, Tak WY, Kweon YO. A case of hemocholecyst associated with hemobilia following radiofrequency ablation therapy for hepatocellular carcinoma. Korean J Hepatol. 2011;17:148-151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Kwon TK, Jeon SH, Park HW, Jung WJ, Hwang JY, Park KS, Cho KB, Hwang JS, Ahn SH, Park SK. [A case of intraluminal gallbladder hematoma after percutaneous liver biopsy]. Taehan Kan Hakhoe Chi. 2002;8:486-489. [PubMed] |
| 3. | Yamamoto T, Kubo S, Hirohashi K, Tanaka S, Uenishi T, Ogawa M, Sakabe K, Hai S, Yamamoto S, Shuto T. Secondary hemocholecyst after radiofrequency ablation therapy for hepatocellular carcinoma. J Gastroenterol. 2003;38:399-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Heise CP, Giswold M, Eckhoff D, Reichelderfer M. Cholecystitis caused by hemocholecyst from underlying malignancy. Am J Gastroenterol. 2000;95:805-808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Ku J, DeLaRosa J, Kang J, Hoyt D, Coimbra R. Acute cholecystitis with a hemocholecyst as an unusual presentation of gallbladder cancer: report of a case. Surg Today. 2004;34:973-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Tan SW, Lai SK, Ng KW, Chen P, Chen KH, Jiang CF. Intramural gallbladder hematoma mimicking gallbladder neoplasm in a 33-year-old male. J Chin Med Assoc. 2005;68:146-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Akatsu T, Tanabe M, Shimizu T, Handa K, Kawachi S, Aiura K, Ueda M, Shimazu M, Kitajima M. Pseudoaneurysm of the cystic artery secondary to cholecystitis as a cause of hemobilia: report of a case. Surg Today. 2007;37:412-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 33] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Shimura T, Kojima T, Tsutsumi S, Yoshida T, Uchiumi H, Kuwano H. Gallbladder hematoma in a patient with hemophilia B, report of a case. Hepatogastroenterology. 2000;47:939-941. [PubMed] |
| 9. | Suaud O, Savoye-Collet C, Suaud L, Scotte M, Dacher JN. [Answer to February e-quid. Spontaneous hemocholecyst in a hemophiliac patient]. J Radiol. 2010;91:314-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Shah VR, Clegg JF. Haemorrhagic cholecystitis. Br J Surg. 1979;66:404-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 24] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Ellington RT, Seidel RH, Burdick JS, Peterson WL, Harford WV. Acalculous cholecystitis presenting as hemobilia and jaundice. Gastrointest Endosc. 2000;51:218-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |