Published online Jan 7, 2013. doi: 10.3748/wjg.v19.i1.133
Revised: September 20, 2012
Accepted: September 28, 2012
Published online: January 7, 2013
Processing time: 143 Days and 14 Hours
Phytobezoar is the most common type of bezoar. It is composed of indigestible vegetable matter and is usually found in the stomach. Biliary phytobezoar is extremely rare and difficult to diagnose preoperatively. The pathogenesis is not clear, and there have been only a few reports of biliary bezoars associated with sphincteric impairmentat the ampulla of Vater. Here, we present a report of biliary bezoar that resulted in jejunal obstruction. We were unable to identifythe bezoar in the extrahepatic bile duct until it obstructed the small bowel lumen. To our knowledge, this is the first report of small bowel obstruction resulting frommigration of a biliary bezoar.
- Citation: Kim Y, Park BJ, Kim MJ, Sung DJ, Kim DS, Yu YD, Lee JH. Biliary phytobezoar resulting in intestinal obstruction. World J Gastroenterol 2013; 19(1): 133-136
- URL: https://www.wjgnet.com/1007-9327/full/v19/i1/133.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i1.133
A bezoar is an intragastric mass consisting of accumulated ingested material. Phytobezoars, the most common type of bezoar, are masses of indigested vegetable matter including skin, seeds, and fruit and vegetable fiber, and are most commonly reported in patients who have had previous gastric surgery[1]. Although normally found in the stomach, a phytobezoar may pass into the small bowel. Primary small bowel bezoarsare very rare, but can form in patients with underlying small bowel disease such as diverticulum, stricture, or tumor[2]. Phytobezoars can also develop secondarily if there are areas of sufficient stagnation within a dilated small bowel loop, as may occur in patients with strictures caused by previous surgery, Crohn’s disease, or tuberculosis[3].
We encountered a case of small bowel obstruction by a ‘biliary’ phytobezoar, which was formed in the extrahepatic bile duct and migrated into the small bowel resulting complete obstruction. Intestinal obstruction due to bezoars is rare, reportedly constituting only 0.44% of all small intestinal obstructions[4,5], and there is an even greater paucity of reports regarding small bowel obstructions caused by the migration of biliary bezoar. The first case report of bezoar-induced obstructive jaundice caused by an intradiverticular bezoar was published by Seryrig et al[6] in 1989, and to date, fewer than 5 cases of biliary bezoar have been reported in the English language literature[6-9].
This report concerns a rare case of biliary bezoar resulting intestinal obstruction, including imaging and clinicopathologic details.
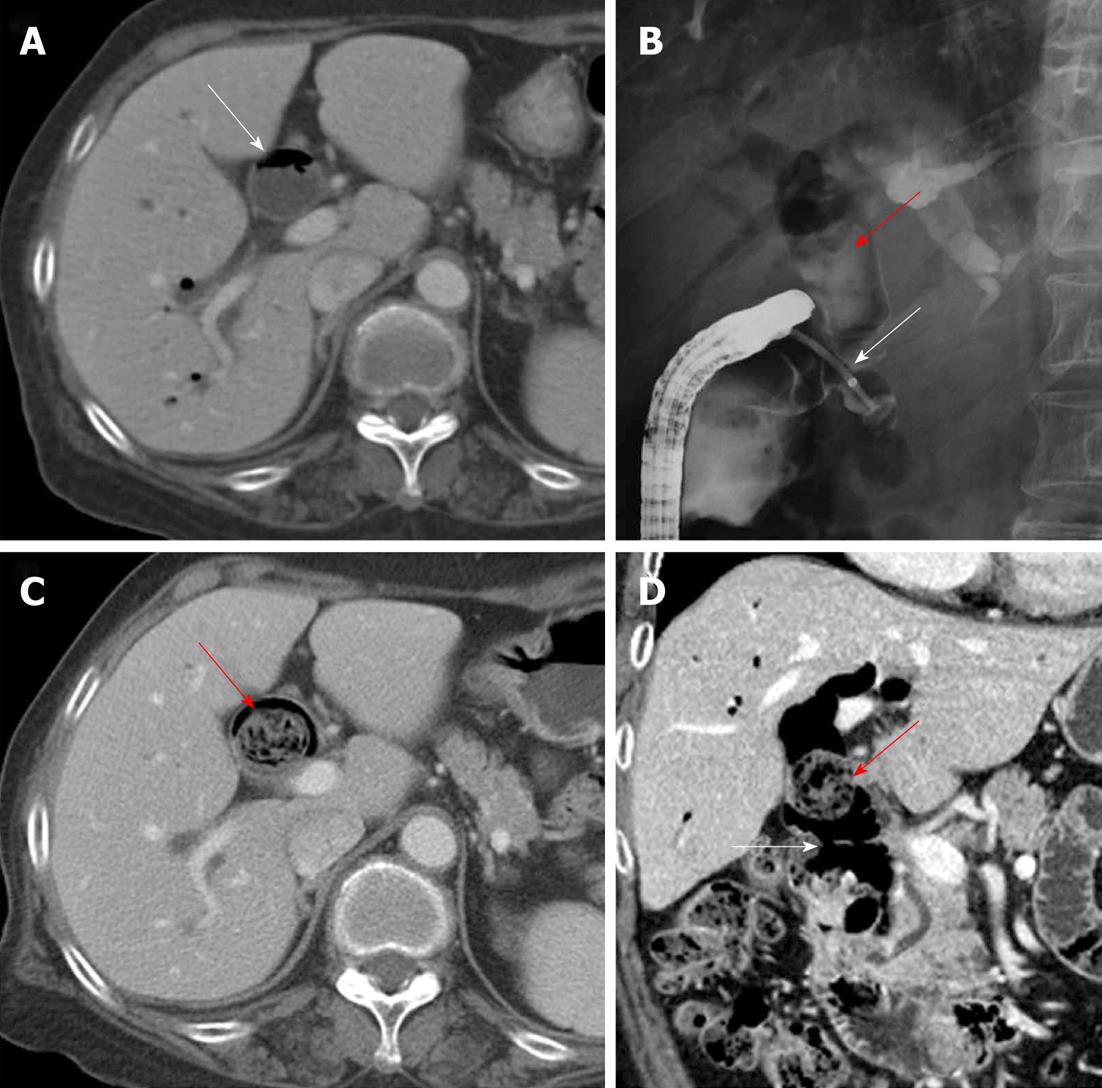
A 72-year-old woman visited the emergency department with a 3-d history of abdominal pain. She had undergone open cholecystectomy with common bile duct (CBD) exploration for acute calculus cholecystitis 12 years previously. Since then, she had experienced recurrent episodes of obstructive jaundice and been hospitalized 3 years ago for recurrent pyogenic cholangitis. Multi-detector computed tomography (MDCT) at that time had shown diffuse and marked bile duct dilatation with pneumobilia (Figure 1A). Although the extent of dilatation was remarkable, there was no evidence of an obstructive mass within the bile ducts. The patient underwent endoscopic retrograde cholangio-pancreatography (ERCP), which revealed a choledochoduodenal fistula (Figure 1B). She was treated with endoscopic nasobiliary drainage and antibiotics and subsequently discharged after a few days of hospital stay.
A routine MDCT checkup 6 mo after discharge showed neither interval changes of the extensive biliary dilatation nor pneumobilia. The choledochoduodenal fistula was seen, along with a newly visible large mass at the extrahepatic bile duct with multiple internal air densities and low attenuation areas resembling impacted food material that was associated with luminal dilatation (Figure 1C). These MDCT features were suggestive of CBD stone or refluxed food material from the second portion of the duodenum (Figure 1D).
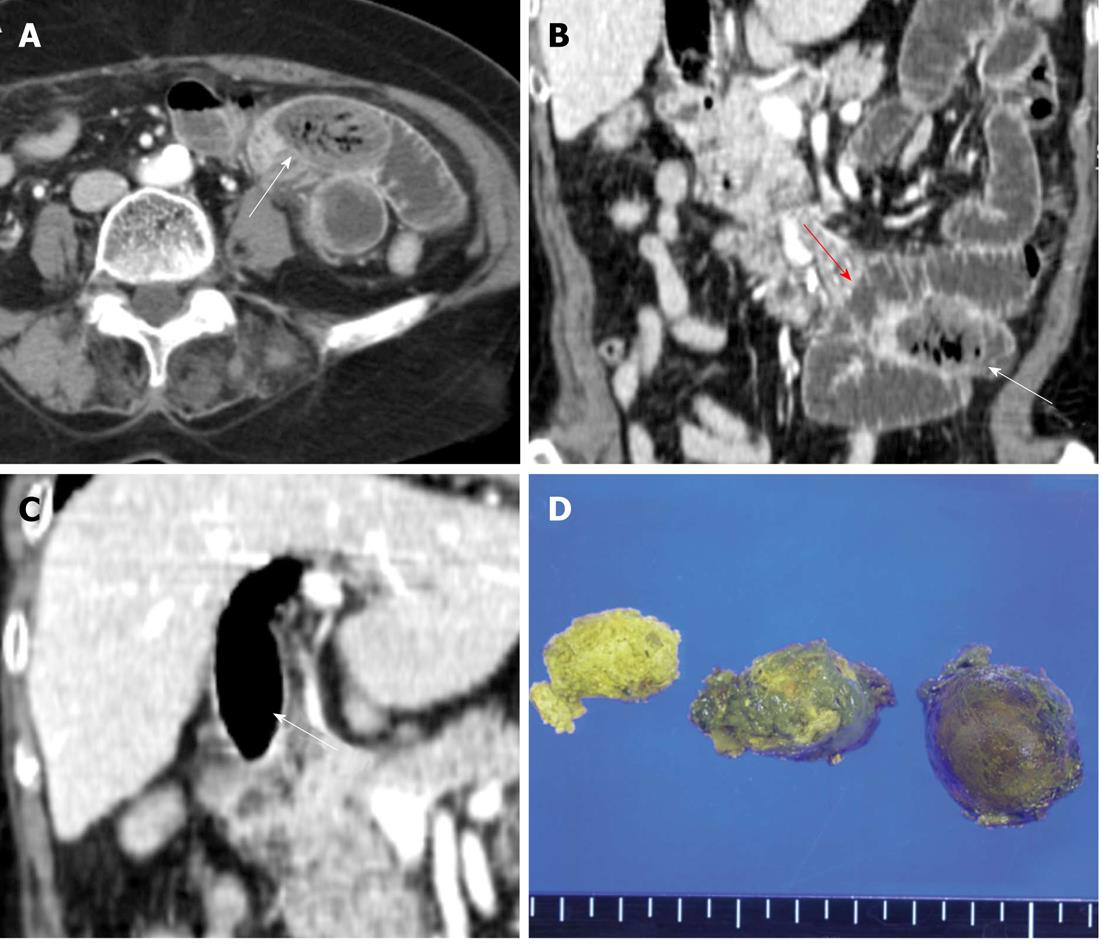
When the patient presented to the emergency room, MDCT confirmed small-bowel obstruction and showed proximal luminal dilatation of the jejunum with focal wall thickening of the transition zone of the mid-jejunum. In the transition zone, well-defined, thin-walled, ovoid food remnants were observed, consistent with bezoars, and these were assumed to be the cause of the obstruction (Figure 2A and B).
The patient underwent exploratory laparotomy with enterotomy, and the obstructing mass at the proximal jejunum was removed. Inflammation-induced segmental wall thickening was observed in the involved small bowel however, there was no sign of bowel perforation or ischemia. The resected mass was pathologically confirmed as a biliary bezoar (Figure 2D), and the histological evaluation indicated that theremoved objects were revealed as fibrinoid materials with some cellular debris.
When we retrospectively reviewed the preoperative computed tomography (CT) images, we concluded that the previously noted CBD mass, which was thought to be refluxed food or a stone, had disappeared. This mass had apparently migrated along the gastrointestinal tract until it reached the jejunal loop of the small bowel, where it resulted in obstruction (Figure 2C). The patient was discharged 1 wk after surgery without any postoperative complications.
Phytobezoar is a type of bezoar that consists of remnants of poorly digested food materials. Phytobezoars are usually reported in patients who have poor mastication, a vegetarian diet, have ingested persimmons, or have undergone previous gastric surgery and vagotomy resulting in diminished motility[10-12].
Biliary phytobezoar is extremely rare, and is reported to develop in patients who have had previous cholecystectomy. In 1995, Lamotte et al[6] were the first to describe a biliary bezoar, which developed in a patient 15 years after cholecystogastrostomy[13]. In other reports, including the present case, biliary bezoar shave developed in patients who have undergone cholecystectomy and had subsequent formation of choledochoduodenal fistulas[9]. Thus, development of biliary bezoar seems to be related to loss of the sphincteric mechanism due to previous biliary-enteric anastomosis or sphincterotomy, which allows reflux of undigested vegetable fibers or food particles from the alimentary tract into the bile ducts[7]. However, biliary bezoarhas also developed in the patients without any sphincteric disruption or impairment. Thus, it is conceivable that some vegetable matter can enter the bile duct through an intact sphincter[7,8].
It is reported that MDCT is the most useful method for diagnosing of small-bowel bezoars because it is able to reveal precise details including location, degree, and features of bezoars[14]. When a patient has a well-defined round or ovoid mass in the intraluminal space with mottled gas pattern causing small-bowel obstruction, bezoar should be considered as the cause of obstruction[14]. A study from France on CT findings that could differentiate small-bowel bezoars from small-bowel feces suggested‘floating fat density debris’, as a CT feature of bezoars, which can be defined in images showing fat-density debris in a region proximal to the obstruction site with dilated bowel loops[15]. The definition proposes that this unusual density arises from the sum of the tissue density of the debris and the negative density of trapped air. However, in our case, no such low-density feature was noted.
MDCT findings for biliary bezoars causing intestinal obstruction have not been previously reported. A biliary bezoar entrapped in the small bowel can be confused with an intraluminal gallstone associated with gallstone ileus or with other types of bezoars formed within gastrointestinal tract. The Rigler’s radiologic criteria (evidence of an ectopic stone in the intestine, air in the biliary tree and gall bladder, and small-bowel obstruction) and direct visualization of choledochoduodenal fistula by MDCT are well known pathognomonic factors for the diagnosis of the gall stone ileus[16,17]. Although the present case fulfilled most criteria for the diagnosis of the gall stone ileus, mottled air densities of intraluminal mass in transition zone of intestinal obstruction was different from Rigler’s criteria and this finding provided diagnostic clue for the final diagnosis as the bezoar rather than gall stone.
It is not possible to classify biliary foreign bodies, including biliary bezoars, in patients who have not had previous surgery or who do not have a biliary enteric fistula, because the radiologic and macroscopic characteristics of biliary bezoarson MDCT and ERCP resemble those of bile duct stones[18]. Therefore, it is important to carefully check for the presence of biloenteric communication and predisposing factors related to bezoar formation ahead of a preoperative diagnosis of a biliary bezoar, because, as noted, most biliary bezoarsare associated with a previous history of biliary abnormality such as choledocho or cholecystoduodenal fistula or diverticula in the walls of the bile ducts and duodenum.
Surgical or laparoscopic excision is the treatment of choice for small bowel bezoars. The entire gastrointestinal tract must be explored to exclude synchronous bezoars and prevent recurrent bowel obstruction caused by residual bezoar[3]. Other non-surgical treatment options include sodium bicarbonate powder, a liquid diet, enzymatic digestion with various agents, endoscopic fragmentation, and oral intake (or endoscopic injection) of ‘Coca-Cola’[19]. A study using combinations of the cola and the endoscopic treatment showed a relatively good response in terms of ability to dissolveor decrease the size of phytobezoars[20].
In conclusion, we have presented a case of small bowel obstruction caused by biliary phytobezoar. Although it is considered extremely rare, biliary bezoar can be one of the possible causes of the mechanical small bowel obstruction in patients with the previously mentioned predisposing factors. We have presented this case to promote further awareness of the interesting phenomenon of biliary bezoar formation associated with abilo digestive fistula, as well as the possibility of subsequent small bowel obstruction due tomigration of the biliary bezoar.
P- Reviewers Papavramidis T, Vikram K, Manta R, Tsujikawa T, Cho YS S- Editor Gou SX L- Editor A E- Editor Xiong L
| 1. | Angelelli G, Magliocca M, Zaccheo N, Vinci R, Rotondo A. [Intestinal obstruction caused by phytobezoar: computerized tomography findings. Report of 3 cases]. Radiol Med. 1997;93:789-791. [PubMed] |
| 2. | Teng H, Nawawi O, Ng K, Yik Y. Phytobezoar: an unusual cause of intestinal obstruction. Biomed Imaging Interv J. 2005;1:e4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Ezzat RF, Rashid SA, Rashid AT, Abdullah KM, Ahmed SM. Small intestinal obstruction due to phytobezoar: a case report. J Med Case Rep. 2009;3:9312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Quiroga S, Alvarez-Castells A, Sebastià MC, Pallisa E, Barluenga E. Small bowel obstruction secondary to bezoar: CT diagnosis. Abdom Imaging. 1997;22:315-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Goldstein SS, Lewis JH, Rothstein R. Intestinal obstruction due to bezoars. Am J Gastroenterol. 1984;79:313-318. [PubMed] |
| 6. | Lamotte M, Kockx M, Hautekeete M, Holvoet J, Hubens H. Biliary phytobezoar: a medical curiosity. Am J Gastroenterol. 1995;90:1346-1348. [PubMed] |
| 7. | Cetta F, Lombardo F, Rossi S. Large foreign body as a nidus for a common duct stone in a patient without spontaneous biliary enteric fistula or previous abdominal surgery. HPB Surg. 1993;6:235-242. [PubMed] |
| 8. | Procházka V, Krausová D, Kod’ousek R, Zámecníková P. Foreign material as a cause of choledocholithiasis. Endoscopy. 1999;31:383-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Moghaddam JA, Amini M, Adibnejad S. Development of bile duct bezoars following cholecystectomy caused by choledochoduodenal fistula formation: a case report. BMC Gastroenterol. 2006;6:1. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Chisholm EM, Leong HT, Chung SC, Li AK. Phytobezoar: an uncommon cause of small bowel obstruction. Ann R Coll Surg Engl. 1992;74:342-344. [PubMed] |
| 11. | Rubin M, Shimonov M, Grief F, Rotestein Z, Lelcuk S. Phytobezoar: a rare cause of intestinal obstruction. Dig Surg. 1998;15:52-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 12. | Kement M, Ozlem N, Colak E, Kesmer S, Gezen C, Vural S. Synergistic effect of multiple predisposing risk factors on the development of bezoars. World J Gastroenterol. 2012;18:960-964. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 46] [Cited by in RCA: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 13. | Seyrig JA, Chambon J, Fritsch J, Berger M, Liguory C, Chousterman M. [Cholestasis caused by an intradiverticular bezoar. Endoscopic treatment]. Gastroenterol Clin Biol. 1989;13:741-743. [PubMed] |
| 14. | Delabrousse E, Brunelle S, Saguet O, Destrumelle N, Landecy G, Kastler B. Small bowel obstruction secondary to phytobezoar CT findings. Clin Imaging. 2001;25:44-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Delabrousse E, Lubrano J, Sailley N, Aubry S, Mantion GA, Kastler BA. Small-bowel bezoar versus small-bowel feces: CT evaluation. AJR Am J Roentgenol. 2008;191:1465-1468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Papavramidis TS, Potsi S, Paramythiotis D, Michalopoulos A, Papadopoulos VN, Douros V, Pantoleon A, Foutzila-Kalogera A, Ekonomou I, Harlaftis N. Gallstone obstructive ileus 3 years post-cholecystectomy to a patient with an old ileoileal anastomosis. J Korean Med Sci. 2009;24:1216-1219. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Lassandro F, Romano S, Ragozzino A, Rossi G, Valente T, Ferrara I, Romano L, Grassi R. Role of helical CT in diagnosis of gallstone ileus and related conditions. AJR Am J Roentgenol. 2005;185:1159-1165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 83] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 18. | Kim TO, Lee SH, Kim GH, Heo J, Kang DH, Song GA, Lee JW, Cho M. Common bile duct stone caused by a phytobezoar. Gastrointest Endosc. 2006;63:324; discussion 324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Ha SS, Lee HS, Jung MK, Jeon SW, Cho CM, Kim SK, Choi YH. Acute intestinal obstruction caused by a persimmon phytobezoar after dissolution therapy with Coca-Cola. Korean J Intern Med. 2007;22:300-303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Lee BJ, Park JJ, Chun HJ, Kim JH, Yeon JE, Jeen YT, Kim JS, Byun KS, Lee SW, Choi JH. How good is cola for dissolution of gastric phytobezoars? World J Gastroenterol. 2009;15:2265-2269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 38] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |