Published online Sep 28, 2012. doi: 10.3748/wjg.v18.i36.5142
Revised: May 16, 2012
Accepted: May 26, 2012
Published online: September 28, 2012
Air in the main pancreatic duct has been reported only rarely and might be associated with either a spontaneous or a surgically induced alteration of the anatomy of the biliary tract. We report a case of “innocent” air found incidentally in the main pancreatic duct. To our knowledge, this is only the third such case reported. A 54-year-old woman presented with hemoptysis that had lasted for 3 d. She underwent a chest computed tomography scan, which revealed not only focal bronchiectasis in the left lower lobe, but also air in the main pancreatic duct and dilatation of the common bile duct. She was managed conservatively for the hemoptysis and no further problems developed. She had no specific gastrointestinal symptoms and had no history of surgery or medication. Her laboratory parameters were normal. Magnetic resonance cholangiopancreatography also demonstrated air in the main pancreatic duct and a dilated common bile duct (CBD). Duodenoscopy revealed separate biliary and pancreatic orifices with patulous openings and some air bubbles appearing in the pancreatic orifice. Endoscopic retrograde cholangiopancreatography (ERCP) showed the dilated CBD and pancreatic duct with some air bubbles, but no other abnormal lesions. She was discharged with no further problems. Most patients with air in the main pancreatic duct have had a pancreatobiliary disease, or a history of pancreatobiliary disease, pancreatobiliary surgery or sphincterotomy. If the air is innocent, as in our case, ERCP should be performed to evaluate any altered sphincteric function or anatomy such as patulous openings.
- Citation: Kim YJ, Kim HK, Cho YS, Kim SS, Chae HS, Kim SK, Kim ES, Lee SY. Air in the main pancreatic duct: A case of innocent air. World J Gastroenterol 2012; 18(36): 5142-5144
- URL: https://www.wjgnet.com/1007-9327/full/v18/i36/5142.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i36.5142
Air in the pancreas is unusual and is usually related to an abscess, emphysematous pancreatitis or a pancreatic fistula[1,2]. There have been several cases reported, including one case series of air in the main pancreatic duct rather than in the pancreas itself[3-9].
This phenomenon has been reported in a child with biliary and pancreatic ascariasis with liver abscesses and a pancreatic pseudocyst[3], in an adult patient with cystic dilatation of the main pancreatic duct limited to the head of the organ[4], in a patient after transampullary septectomy[5], in 11 patients with various acute or chronic pancreatic and/or biliary diseases[6], in three infants with a congenital duodenal obstruction[7], in a middle-aged man with a history of acute pancreatitis[8], and in a young woman with acute pancreatitis and a pseudocyst[9]. Among these patients, most had a pancreatobiliary disease, or a history of pancreatobiliary disease, pancreatobiliary surgery or sphincterotomy, whereas only two patients had no such background.
We report a case of “innocent” air in the main pancreatic duct found incidentally. The patient had no history of a pancreatobiliary disease and had no pancreatic or biliary symptoms.
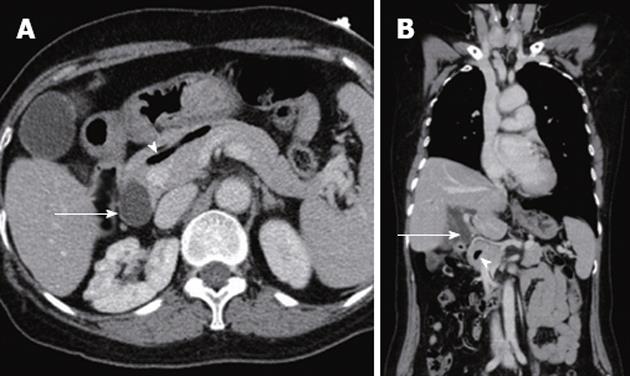
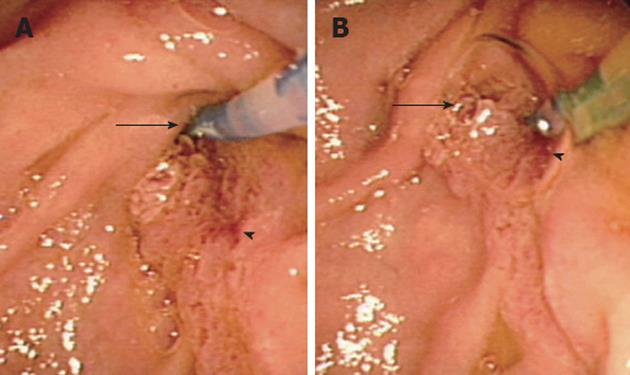
A 54-year-old woman presented at our hospital’s division of pulmonology with hemoptysis that had lasted for 3 d. She underwent a chest computed tomography (CT) scan, which revealed not only focal bronchiectasis in the left lower lobe, but also air in the main pancreatic duct (arrowhead in Figure 1) and dilatation of the common bile duct (CBD; arrow in Figure 1). She was managed conservatively for the hemoptysis and no further problems developed. She was referred to the gastrointestinal (GI) division for an evaluation. She had no specific GI symptoms such as abdominal pain and had no history of surgery or medication. Her laboratory parameters were normal (hemoglobin, 14.8 g/dL; white blood cell, 6400/mm3; aspartate aminotransferase/alanine aminotransferase, 17/16 IU/L; total bilirubin, 1.14 mg/dL; alkaline phosphatase, 182 IU/L; γ-glutamyl transpeptidase, 31 IU/L; amylase, 94 IU/L). To better evaluate the pancreatic ductal system, magnetic resonance cholangiopancreatography (MRCP) was carried out. This also demonstrated air in the main pancreatic duct and the dilated CBD. To further evaluate the ampulla of Vater and the pancreatobiliary ductal system, endoscopic retrograde cholangiopancreatography (ERCP) was carried out. A duodenoscopic examination revealed separate biliary (arrow in Figure 2) and pancreatic orifices with patulous openings and some air bubbles appearing in the pancreatic orifice (arrowhead in Figure 2). The ERCP showed the dilated CBD and pancreatic duct with some air bubbles (Figure 3), but no other abnormal lesions. She was discharged with no further problems.
Here, we report a case of “innocent” air found incidentally in the main pancreatic duct. The patient had no pancreatobiliary disease or history of it. She had separate biliary and pancreatic orifices with patulous openings but displayed no pancreatic or biliary symptoms. To our knowledge, this is only the third case reported of innocent air in the main pancreatic duct[4,6].
This phenomenon has been reported only rarely and might be associated with either a spontaneous or surgically induced alteration of the anatomy of the biliary tract. The origin of such air is not known, but there have been two possible explanations given[6,10]. First, it is likely that air in the pancreatic duct is the result of biliary-pancreatic reflux in patients who have received biliary-enteric anastomoses or have undergone sphincterotomy. Second, in patients who have not undergone such operations, the likely cause of pancreatic duct air is a duodenal-pancreatic duct reflux. This possibility arose from the observation that six of 11 patients with air in the pancreatic duct had undergone previous biliary or pancreatic surgery or had undergone sphincterotomy; these patients all had pneumobilia[6]. However, these patients comprised only 5% of all who had received biliary anastomoses or had undergone sphincterotomy, so this mechanism seemed to operate only in a minority of such patients. Duodenal-pancreatic duct reflux occurring in patients who have not undergone pancreatobiliary surgery or sphincterotomy could be explained by the animal experiment of DiMagno et al[10]. That is, during duodenal phase III motor activity of the interdigestive period, the mean duodenal pressure at times exceeds the mean pancreatic pressure, and reflux of duodenal contents into the pancreatic duct can occur. Generally, the sphincter of Oddi plays a major role in regulating secretory flow and preventing such reflux, but patients who have undergone a sphincterotomy or have had papillitis might have altered sphincter function so that reflux could occur more commonly. However, in three patients with a common channel, air was present only in the pancreatic duct and not in the biliary system[6]. This could be explained neither by a biliary-pancreatic reflux nor by a duodenal-pancreatic duct reflux. Further investigations on the presence of air in the pancreatic duct are needed.
In all previous reports, air in the pancreatic duct was demonstrated by CT scans[3,4,8,9] or ultrasonography[5-7]. CT is known to be sensitive for detecting small amounts of gas. Generally, air in the pancreatic duct is never demonstrated on plain radiographs. In our case, air in the pancreatic duct was found first by a CT scan and then found in MRCP and ERCP studies. In a previous case series, nine of 11 patients underwent a second ultrasound examination and air in the pancreatic duct was only confirmed in five[6]. In another case, air in the pancreatic duct found first on CT scans was not shown in the second MRCP[8]. This spontaneous disappearance of air seemed to be related to the cyclically variable diameter of the pancreatic duct associated with air expulsion or the phasic motor activity of the sphincter of Oddi[6]. As in our case, why air in the pancreatic duct persisted was not understood fully. However, in our case, the major duodenal papilla had separate biliary and pancreatic orifices with patulous openings. This anatomy could have been one cause of air in the pancreatic duct that also affected the persistence of air. Why there was no pneumobilia and the CBD was dilated is also not understood fully; possibly the degree of altered sphincteric function differed between the separate biliary and pancreatic orifices.
In most cases reported in the literature, the patients had a history of biliary and/or pancreatic disease, such as pancreatitis or cholangitis, or a history of pancreatobiliary surgery or sphincterotomy[3,5-9]. Two patients had no history of pancreatobiliary disease or surgery and no pancreatobiliary symptoms[4,6]. Our patient also had no history of pancreatobiliary disease or surgery and no related symptoms. Therefore, this appears to be the third reported case of innocent air in the pancreatic duct. Separate duct orifices with patulous openings might be related to the presence of air in the pancreatic duct and the dilated CBD, but how such patulous openings formed is not known.
In summary, when air in the pancreatic duct is discovered, the physician should investigate a history of pancreatobiliary disease, a history of pancreatobiliary surgery and sphincterotomy and any related symptoms. If the air is innocent, as in our case, ERCP should be performed to evaluate any altered sphincteric function or anatomy such as patulous openings.
Peer reviewer: Dr. Xiaoyun Liao, Department of Medical Oncology, Dana-Farber Cancer Institute, 450 Brookline Avenue, Room JF-208E, Boston, MA 02215, United States
S- Editor Gou SX L- Editor A E- Editor Li JY
| 1. | Warshaw AL. Pancreatic abscesses. N Engl J Med. 1972;287:1234-1236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 76] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Alexander ES, Clark RA, Federle MP. Pancreatic gas: indication of pancreatic fistula. AJR Am J Roentgenol. 1982;139:1089-1093. [PubMed] |
| 3. | Radin DR, Vachon LA. CT findings in biliary and pancreatic ascariasis. J Comput Assist Tomogr. 1986;10:508-509. [PubMed] |
| 4. | Itai Y, Ohtomo K, Kokubo T, Nagai H, Atomi Y, Kuroda A. CT demonstration of gas in dilated pancreatic duct. J Comput Assist Tomogr. 1986;10:1052-1053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Braver JM, Jones TB, Brooks JR. The sonographic appearance of the pancreatic duct following transampullary septectomy. J Ultrasound Med. 1986;5:459-460. [PubMed] |
| 6. | Costa PL, Righetti G. Air in the main pancreatic duct: demonstration with US. Radiology. 1991;181:801-803. [PubMed] |
| 7. | Peer S, Kiechl-Kohlendorfer U, Gassner I. Air in the main pancreatic duct revealed by abdominal ultrasound: an additional diagnostic sign in paediatric patients with duodenal obstruction. Clin Radiol. 2002;57:945-948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 8. | Brindisi C, Calculli L, Casadei R, Pezzilli R. Air in the Wirsung duct. An unusual finding. JOP. 2008;9:534-537. [PubMed] |
| 9. | Tyagi P, Puri AS, Sachdeva S. Spontaneous air in the main pancreatic duct. Indian J Gastroenterol. 2009;28:87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | DiMagno EP, Hendricks JC, Go VL, Dozois RR. Relationships among canine fasting pancreatic and biliary secretions, pancreatic duct pressure, and duodenal phase III motor activity--Boldyreff revisited. Dig Dis Sci. 1979;24:689-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 76] [Article Influence: 1.7] [Reference Citation Analysis (0)] |