Published online Mar 21, 2012. doi: 10.3748/wjg.v18.i11.1270
Revised: November 17, 2011
Accepted: December 31, 2011
Published online: March 21, 2012
Esophageal duplication cysts are rare inherited lesions usually diagnosed in early childhood. Most of them are found in the mediastinum and manifest themselves as separate masses along or in continuity with the native esophagus. Their prevalence remains unknown and they are treated either surgically or endoscopically. In this report we describe a series of four adult patients in whom esophageal duplication cysts were localised intramurally as masses pressing on the esophageal lumen and who were diagnosed with endoscopic ultrasonography. All patients were initially referred to other centres for upper gastroduodenoscopy due to non-specific dyspeptic symptoms. After finding suspicious lesions in the esophagus their endoscopists referred them for endoscopic ultrasound examination at our centre. In two of the cases lesions mimicked esophageal varices and the other two submucosal tumours. In all four patients endoscopic ultrasonography has shown esophageal duplication cysts. Patients had no symptoms suggesting disease of the esophagus and required no treatment. As the true prevalence of esophageal cysts is unknown, it is very likely that in many patients, like in these four described by us, they may cause no symptoms, remain undetected and require no intervention. Increasing availability of new diagnostic modalities such as endoscopic ultrasonography may change the current view regarding the prevalence of esophageal duplication cysts and prove that they may, in fact, not be such rare findings.
- Citation: Wiechowska-Kozłowska A, Wunsch E, Majewski M, Milkiewicz P. Esophageal duplication cysts: Endosonographic findings in asymptomatic patients. World J Gastroenterol 2012; 18(11): 1270-1272
- URL: https://www.wjgnet.com/1007-9327/full/v18/i11/1270.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i11.1270
Esophageal duplication cysts are congenital anomalies of the foregut resulting from aberration of the posterior division of the embryonic foregut at 3-4 wk gestation[1]. They represent either simple epithelial-lined cysts, or true esophageal duplication, which is a duplication of the muscularis mucosa and externa without epithelial duplication.
Esophageal cysts are considered rare, usually described in single case reports, and their true prevalence remains unknown[2]. Up to 80% of cases are diagnosed during childhood[1-5]. Most of them are found in the mediastinum and manifest themselves as separate masses along or in continuity with the native esophagus. Intramural esophageal cysts are considered very uncommon in adults[6,7].
Symptoms are caused by compression or displacement of surrounding mediastinal structures and comprise dysphagia, respiratory distress, failure to thrive and retrosternal pain[7,8]. Malignant progression is considered extremely rare[9]. Diagnosis is usually made by computed tomography scan or endoscopic ultrasonography (EUS).
Treatment of symptomatic esophageal cysts can be either surgical or endoscopic. Surgical resection of the cyst is usually carried out in childhood or in adults, in cases of lesions impossible to treat endoscopically. Surgical treatment is currently moving from thoracotomy to less-invasive procedures, such as video-assisted thoracoscopic surgery[7] and to endoscopic treatments which, however, still remain challenging interventions[10].
We present a series of 4 patients with esophageal cysts which caused no symptoms and required no intervention.
All patients were initially referred to other centres for upper gastroduodenoscopy due to non-specific, dyspeptic symptoms. They gave no history of dysphagia. After finding suspicious lesions in the esophagus their endoscopists referred them for EUS examination. Written informed consent was obtained from each patient.
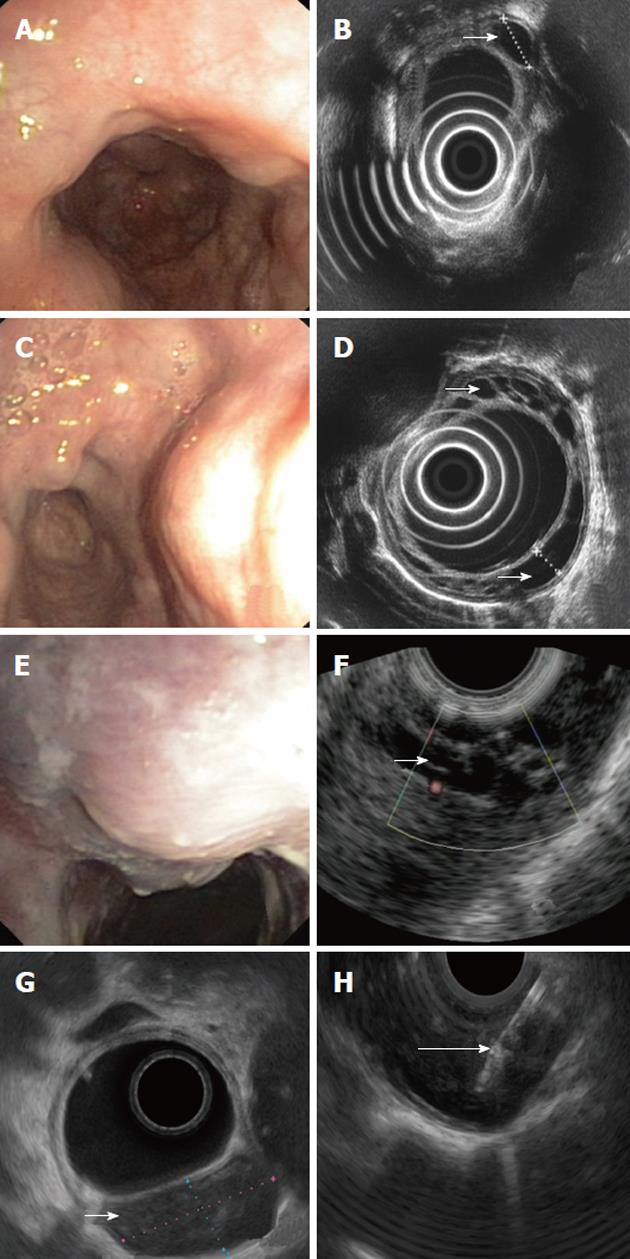
A 60-year old female: On endoscopy, multiple impressions, covered with normal mucosa and localized to the middle and lower third of the esophagus were seen (Figure 1A). They could be easily passed by the endoscope. No other abnormality was found on endoscopy. On EUS multiple cystic fluid-filled intramural lesions were detected (Figure 1B). They were avascular on Doppler study and their size varied from 3 mm × 5 mm to 11 mm × 25 mm.
A 51-year old male: Endoscopy revealed multiple impressions, covered with normal mucosa and localized in the lower third of the esophagus (Figure 1C). The prepyloric area showed features of atrophic gastritis subsequently confirmed with histology. On EUS, multiple cystic, fluid-filled, intramural lesions were detected (Figure 1D). Their size varied from 4 mm × 6 mm to 8 mm × 16 mm. They showed no vascular pattern on Doppler examination.
A 57-year old female: Endoscopy showed a solitary impression, localized 25 cm from the incisor teeth and covered with unchanged mucosa (Figure 1E). Examination was otherwise unremarkable. EUS revealed a cluster of unechoic fluid-filled intramural lesions showing no vascular pattern on Doppler examination (Figure 1F).
A 47-year old male: Endoscopy revealed a solitary lesion, size approximately 25 mm localized 30 cm from the incisor teeth and covered with unchanged mucosa (Figure 1G). No other abnormality was found on endoscopy. EUS demonstrated an unechoic fluid-filled intramural lesion 24 mm × 12 mm large. The lesion showed no vascular pattern on Doppler examination (Figure 1H). Aspiration with 18G needle revealed a clear fluid with no malignant or suspicious cells.
In this paper we describe a series of 4 patients who were referred to our centre for further investigation of esophageal lesions found on routine gastroduodenoscopy. In two cases, where there were multiple lesions, referring doctors suspected unusual looking varices or vascular lesions. In view of our interest in EUS of portal hypertension[11-13] a more detailed study of both the lesions and intrinsic para- and peri-esophageal circulation was performed. However, these patients had no clinical, laboratory or imaging features suggesting liver cirrhosis or portal hypertension. In the other two cases the initial diagnosis was submucosal tumours. These findings were expected to be confirmed using EUS. All these patients turned out to have esophageal duplication cysts.
Esophageal cysts do not usually communicate with the esophageal wall but occur as a separate malformation along or in continuity with the native esophagus. In the presented cases they were localized intramurally as a mass pressing on the esophageal lumen and this is why they resembled esophageal varices or submucosal tumours.
Treatment of esophageal duplication cysts in asymptomatic patients is controversial with no clear clinical guidelines. As all our patients remained asymptomatic we arbitrarily decided to schedule them for follow up EUS/gastroduodenoscopy in a period of 2 years. An earlier intervention will be performed if they become symptomatic.
As the true prevalence of esophageal cysts is unknown[2], it is very likely that in many patients, like in these four described by us, they cause no symptoms, remain undetected and require no intervention at all. Increasing availability of new diagnostic modalities such as EUS may change the current view regarding the prevalence of esophageal duplication cysts and prove that they are not rare findings.
Peer reviewers: Orhan Sezgin, Professor, Gastroenteroloji Bilim Dal, Mersin Üniversitesi Tp Fakültesi, Mersin 33190, Turkey; Michael Keese, Associate Professor, Clinic For Vascular and Endovascular Surgery, Johann Wolfgang Goethe Universität Frankfurt, Theodor-Stern-Kai 7, Frankfurt am Main 60590, Germany
S- Editor Gou SX L- Editor O’Neill M E- Editor Li JY
| 1. | Eichmann D, Engler S, Oldigs HD, Schroeder H, Partsch CJ. Radiological case of the month. Denouement and discussion: congenital esophageal duplication cyst as a rare cause of neonatal progressive stridor. Arch Pediatr Adolesc Med. 2001;155:1067-1068. [PubMed] [Cited in This Article: ] |
| 2. | Wootton-Gorges SL, Eckel GM, Poulos ND, Kappler S, Milstein JM. Duplication of the cervical esophagus: a case report and review of the literature. Pediatr Radiol. 2002;32:533-535. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Arbona JL, Fazzi JG, Mayoral J. Congenital esophageal cysts: case report and review of literature. Am J Gastroenterol. 1984;79:177-182. [PubMed] [Cited in This Article: ] |
| 4. | Danzer E, Paek BW, Farmer DL, Poulain FR, Farrell JA, Harrison MR, Albanese CT. Congenital diaphragmatic hernia associated with a gastroesophageal duplication cyst: a case report. J Pediatr Surg. 2001;36:626-628. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Markert DJ, Grumbach K, Haney PJ. Thoracoabdominal duplication cyst: prenatal and postnatal imaging. J Ultrasound Med. 1996;15:333-336. [PubMed] [Cited in This Article: ] |
| 6. | Diaz de Liaño A, Ciga MA, Trujillo R, Aizcorbe M, Cobo F, Oteiza F. Congenital esophageal cysts--two cases in adult patients. Hepatogastroenterology. 1999;46:2405-2408. [PubMed] [Cited in This Article: ] |
| 7. | Cioffi U, Bonavina L, De Simone M, Santambrogio L, Pavoni G, Testori A, Peracchia A. Presentation and surgical management of bronchogenic and esophageal duplication cysts in adults. Chest. 1998;113:1492-1496. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 108] [Cited by in F6Publishing: 115] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 8. | Harvell JD, Macho JR, Klein HZ. Isolated intra-abdominal esophageal cyst. Case report and review of the literature. Am J Surg Pathol. 1996;20:476-479. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 50] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Singh S, Lal P, Sikora SS, Datta NR. Squamous cell carcinoma arising from a congenital duplication cyst of the esophagus in a young adult. Dis Esophagus. 2001;14:258-261. [PubMed] [DOI] [Cited in This Article: ] |
| 10. | Will U, Meyer F, Bosseckert H. Successful endoscopic treatment of an esophageal duplication cyst. Scand J Gastroenterol. 2005;40:995-999. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Wiechowska-Kozłowska A, Białek A, Raszeja-Wyszomirska J, Starzyńska T, Milkiewicz P. Ligation of oesophageal varices may increase formation of "deep" gastric collaterals. Hepatogastroenterology. 2012;57:262-267. [PubMed] [Cited in This Article: ] |
| 12. | Wiechowska-Kozlowska A, Raszeja-Wyszomirska J, Wasilewicz MP, Bialek A, Wunsch E, Wójcicki M, Milkiewicz P. Upper gastrointestinal endosonography in patients evaluated for liver transplantation. Transplant Proc. 2009;41:3082-3084. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Wiechowska-Kozłowska A, Białek A, Milkiewicz P. Prevalence of 'deep' rectal varices in patients with cirrhosis: an EUS-based study. Liver Int. 2009;29:1202-1205. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |