Published online Mar 21, 2012. doi: 10.3748/wjg.v18.i11.1262
Revised: July 28, 2011
Accepted: August 15, 2011
Published online: March 21, 2012
AIM: To investigate the incidence and mortality of gastric cancer (GC) in Zhuanghe region, northeast China and the influencing factors for their changing trends.
METHODS: All new cancer cases and deaths registered from 2005 to 2010 in Zhuanghe County were reviewed. The annual GC cases, constituent ratio, crude rates, age-standardized rates, their sex and age distribution and temporal trends were assessed. The method of annual percentage change (APC) was used to estimate the trends of GC.
RESULTS: Altogether 2634 new cases of GC and 1722 related deaths were registered, which accounted for 21.04% and 19.13% of all cancer-related incidence and deaths, respectively. The age-standardized incidence rate steadily decreased from 57.48 in 2005 to 44.53 in 2010 per 105 males, and from 18.13 to 14.70 per 105 females, resulting in a APC of -5.81% for males and -2.89% for females over the entire period. The magnitude of APC in GC mortality amounted to -11.09% and -15.23%, respectively, as the age-standardized mortality rate steadily decreased from 42.08 in 2005 to 23.71 in 2010 per 105 males, and from 23.86 to 10.78 per 105 females. Females had a significantly lower incidence (a male/female ratio 2.80, P < 0.001) and mortality (a male/female ratio 2.30, P < 0.001). In both genders, the peak incidence and mortality occurred in the 80-84 years age group. The age-standardized mortality/incidence ratio also decreased from the peak of 0.73 in 2005 to 0.53 in 2010 for males, and from 1.32 to 0.73 for females.
CONCLUSION: Encouraging declines of incidence and mortality of GC were observed in Zhuanghe region between 2005 and 2010, possibly due to the economic development and efficient GC control strategies.
- Citation: Jing JJ, Liu HY, Hao JK, Wang LN, Wang YP, Sun LH, Yuan Y. Gastric cancer incidence and mortality in Zhuanghe, China, between 2005 and 2010. World J Gastroenterol 2012; 18(11): 1262-1269
- URL: https://www.wjgnet.com/1007-9327/full/v18/i11/1262.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i11.1262
Gastric cancer (GC) is one of the most frequently occurring cancers globally; a total of 989 600 new GC cases and 738 000 deaths are estimated to have occurred in 2008, accounting for 8% of the total cases and 10% of total cancer-related deaths, respectively[1]. The geographical distribution of GC exhibits wide international variation and over 70% of new cases and deaths occur in developing countries[1,2]. Although a notable decreasing trend has been recently observed in the developed countries, the incidence of GC is still high[3] and it remains an important public health burden in China. Moreover, there is a significant regional disparity in the distribution of GC in China. People in rural areas are supposed to have a higher risk of GC than those in cities[4], thus, strategy of GC control in China should be implemented specifically based on the different distribution patterns.
Zhuanghe is a county of northern China with a total population of approximate 900 000, of whom approximately 87.2% are agricultural residents. It is located along the coast of the Huanghai Sea and occupies an area of approximately 4034 km2[5]. Zhuanghe has been recognized for its high GC mortality since 1984, the mortality rate being 49.55/105 in males and 22.23/105 in females[6]. The high risk of GC in this region aroused the interest of researchers, and a series of investigations regarding the potential risk factors and corresponding etiological intervention methods and screening measures were conducted in representative villages[7]. To date, the population in Zhuanghe County has been surveyed through census for 28 years. Various risk factors, such as salted pork, Helicobacter pylori (H. pylori) infection with a specific strain, and genetic polymorphisms in the etiology of GC in local residents have been found to play a role[8-12]. In addition, several pilot surveys regarding incidence and mortality were also conducted. The GC mortality rates fluctuated between 63.29/105 and 38.98/105 during the period of 1996-2003 and the incidence rate was 35.42-41.03/105 from 1998 to 2004[7,13,14].
Despite some epidemiological surveys in pilot areas, a population-based investigation concerning the incidence and mortality of GC in Zhuanghe has not been previously reported. Monitoring and studying the incidence as well as mortality provides important information, enabling effective assessment of potential cancer prevention and control. Therefore, the aim of the present study is to examine the GC patterns and temporal trends of incidence and mortality at the population level in Zhuanghe region and to elucidate the factors that influence the changing trends, in an attempt to establish future general and specific strategies for the prevention and control of cancers.
The preliminary cancer surveillance was conducted in Zhuanghe as a high-risk GC research base in 1984. However, previous cancer data were obtained from limited populations and sample surveys. Over the past two decades, a cancer registry was developed along with an expanding research scope, with coverage of only several villages initially in the 1980s which increased to 70 villages in the 1990s. Since 2001, a population-based cancer registry has been gradually established, in collaboration with the Cancer Registration Office of Liaoning Province, China that has collected information on all deaths and all cancer cases in Zhuanghe County and has functioned well since 2005.
The framework of this registry consisted of three parts: village clinics that served as basic units, rural administration units, and Center of Disease Prevention and Control (CDC) of Zhuanghe County. Village clinic doctors were required to report each new case of cancer using a standard card to the rural administration unit. The cards were then submitted to the CDC of Zhuanghe, registered and processed on a regular basis. These cards were checked, analyzed, coded and stored at the CDC. All data were coded according to the manual “National Criteria of Cancer Registry in China”, which describes the cancer inclusion and exclusion criteria, and provides definitions and coding for cancer cases. The accuracy of the data was assured through the comprehensive training of doctors and registrars by the Cancer Registration Office of Liaoning Province, and by computerized consistency checks. At the end of each year, a sample survey was conducted to check the quality of the registration. The cancer occurrence data were compared one by one with the death registry database data to supplement cases of cancer death which were not registered for cancer occurrence.
Annual GC cases data were provided by the CDC of Zhuanghe County. All data were coded and checked for eligibility and validity prior to analysis. Data collected on each patient included demographics and native origins, primary cancer site/type, morphology, and pathological diagnosis confirmation, stage of the disease, and active patient follow-up. The 10th revision of International Classification of Diseases (ICD-10) was used for cancer classification. Data concerning age and sex in the Zhuanghe population were provided by the local police station.
All of the data were checked and analyzed by SPSS 13.0 software (SPSS, Chicago, Illinois, United States). Incidence and mortality rates were calculated as the mean annual number per 100 000 residents. Age-standardized incidence rates (ASRs) and age-standardized mortality rates (ASMRs) were calculated using a direct method[15] by weighting age-specific incidence and mortality rates in accordance with the World Standard Population (World Health Organization, published in 2000) and the China Standard Population (2000). The Chi-squared test was used to determine whether the differences between sexes were statistically significant, and the test was also used to examine trends of annual change in crude rates.
The average annual percent change (APC)[16,17] was estimated by fitting a regression line to the natural logarithm of the rates using the calendar year as the regression variable, i.e., y = mx + b in which y = ln (rate) and x = calendar year. The estimated APC = 100 (em-1) and 95% CI of APC = 100 (em ± SEm-1), where the standard error of m (SEm) was obtained according to the fit of the regression line. To test the hypothesis that the APC equals zero is equivalent to the hypothesis that the slope of the regression line is zero, the t-distribution of m/SEm was used. The number of degrees of freedom is equivalent to the number of calendar years minus two. This calculation assumes that the rate increased/decreased at a constant rate over the entire period. Statistical significance was assessed by the two-sided Student’s t test, and P < 0.05 was considered statistically significant.
Ethical approval for this study was obtained from the Human Ethics Review Committee of China Medical University (Shenyang, China). Written informed consents were obtained from the participants in accordance with the Declaration of Helsinki and its later revisions.
From 2005 to 2010, a total of 2634 new cases of GC were registered in Zhuanghe, including 1950 males and 684 females. We analyzed the constituent ratios for incidence according to various types of cancer (Table 1). GC ranked first among all types of cancers in males, whereas it ranked the second among females and both sexes combined. The ten most common types of cancer in the Zhuanghe population were lung, stomach, liver, colon/rectum, breast, esophageal, thyroid, bladder, pancreatic cancers, and cancer of brain and nervous system. These cancers comprised 80.74% of all cases of cancer. The five predominant primary cancer sites in males were stomach, lung, liver, and esophagus; whereas in females, the leading sites were lung, stomach, breast, colon/rectum, and thyroid.
| Rank | Total | Males | Females | |||||||||
| Cancer | ICD-10 | Cases | CR % | Cancer | ICD-10 | Cases | CR% | Cancer | ICD-10 | Cases | CR % | |
| 1 | LC | C33-34 | 2673 | 21.35 | GC | C16 | 1950 | 26.41 | LC | C33-34 | 1068 | 20.80 |
| 2 | GC | C16 | 2634 | 21.04 | LC | C33-34 | 1605 | 21.74 | GC | C16 | 684 | 13.32 |
| 3 | HCC | C22 | 1488 | 11.89 | HCC | C22 | 1093 | 14.80 | BC | C50 | 617 | 12.02 |
| 4 | CRC | C18-21 | 1211 | 9.67 | CRC | C18-21 | 719 | 9.74 | CRC | C18-21 | 492 | 9.58 |
| 5 | BC | C50 | 636 | 5.08 | EC | C15 | 322 | 4.36 | TC | C73 | 234 | 4.56 |
| 6 | EC | C15 | 364 | 2.91 | BLC | C67 | 246 | 3.33 | CC | C53 | 212 | 4.13 |
| 7 | TC | C73 | 317 | 2.53 | PC | C25 | 151 | 2.05 | EMC | C54 | 135 | 2.63 |
| 8 | BLC | C67 | 286 | 2.28 | CNC | C70-72 | 135 | 1.83 | CNC | C70-72 | 111 | 2.16 |
| 9 | PC | C25 | 253 | 2.02 | PRC | C61 | 85 | 1.15 | OC | C56 | 105 | 2.05 |
| 10 | CNC | C70-72 | 246 | 1.97 | KC | C64 | 83 | 1.12 | PC | C25 | 102 | 1.99 |
| Total | 10108 | 80.74 | Total | 6389 | 86.53 | Total | 3760 | 73.24 | ||||
The incidence rate of GC occurring over different years was analyzed. We initially calculated the annual crude incidence rate according to sex. The average crude incidence rate of GC in males was 70.23/105, which was 2.80-fold higher than in females (25.12/105). The difference was statistically significant (χ2 = 584.31, P < 0.001). Over the past 6 years, no obvious increasing or decreasing trend was observed concerning crude incidence (P = 0.404 in males, 0.061 in females and 0.101 in both sexes) (Table 2).
| Year | Total | Males | Females | |||||||||
| Cases | Crude | ASR1 | ASR2 | Cases | Crude | ASR1 | ASR2 | Cases | Crude | ASR1 | ASR2 | |
| 2005 | 409 | 44.74 | 33.41 | 37.67 | 312 | 67.51 | 47.92 | 57.48 | 97 | 21.46 | 16.97 | 18.13 |
| 2006 | 437 | 47.62 | 34.89 | 40.12 | 323 | 69.63 | 48.01 | 60.06 | 114 | 25.12 | 19.30 | 20.66 |
| 2007 | 411 | 44.60 | 32.88 | 37.77 | 314 | 67.42 | 46.89 | 57.86 | 97 | 21.28 | 16.68 | 18.17 |
| 2008 | 474 | 51.36 | 31.65 | 35.30 | 346 | 74.26 | 42.69 | 51.05 | 128 | 28.01 | 18.53 | 19.60 |
| 2009 | 476 | 51.98 | 30.55 | 34.04 | 337 | 72.97 | 39.58 | 47.66 | 139 | 30.63 | 19.53 | 20.30 |
| 2010 | 427 | 47.03 | 26.84 | 29.83 | 318 | 69.55 | 38.46 | 44.53 | 109 | 24.18 | 13.67 | 14.70 |
| Total | 2634 | 47.89 | 31.25 | 35.10 | 1950 | 70.23 | 43.28 | 51.95 | 684 | 25.12 | 17.17 | 18.26 |
| χ2 trend test | χ2 = 2.693, P = 0.101 | χ2 = 0.696, P = 0.404 | χ2 = 3.519, P = 0.061 | |||||||||
| APC | APC = -4.82%, P = 0.019 | APC = -5.81%, P = 0.008 | APC = -2.89%, P = 0.383 | |||||||||
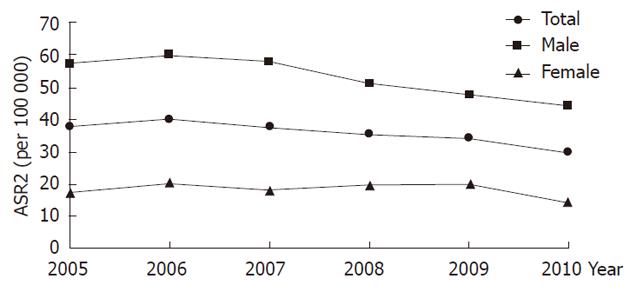
To adjust for the effect of age differences over different time periods, age-standardized incidence rates were calculated in accordance with the China Standard Population (ASR1) and World Standard Population (ASR2). As shown in Figure 1, over the past 6 years, the incidence rate of GC has gradually decreased. For both genders, the ASR2 decreased from 37.67 to 29.83 per 105 with an APC of -4.82% (95% CI: -3.58% to -6.04%; P = 0.019) and for males the rate decreased from 57.48 to 44.53 per 105 with an APC of -5.81% (95% CI: -4.67% to -6.94%; P = 0.008). The ASR2 decreased from 18.13 to 14.70 per 105 with an APC of -2.89% (95% CI: 0.06% to -5.75%) in females; however, the change had no statistical significance (P = 0.383) (Table 2).
In both genders, GC was very rare among populations younger than 20 years, but the rate rose sharply to a peak at approximately 80 years of age, and it declined afterwards. The median age of GC patients was 67 years and the average age was 65.78 years. The cases above 50 years old accounted for 88.65% of all GC cases.
There were a total of 1722 GC deaths between 2005 and 2010 in Zhuanghe, including 1207 males and 515 females. Table 3 shows the constituent ratio of malignant tumors leading to death, in which GC accounted for 19.13% (21.58% in males and 15.11% in females) of the total cancer deaths, making it the second leading cause of cancer death.
| Rank | Total | Males | Females | |||||||||
| Cancer | ICD-10 | Cases | CR % | Cancer | ICD-10 | Cases | CR % | Cancer | ICD-10 | Cases | CR% | |
| 1 | LC | C33-34 | 2683 | 29.81 | LC | C33-34 | 1560 | 27.89 | LC | C33-34 | 1123 | 32.95 |
| 2 | GC | C16 | 1722 | 19.13 | GC | C16 | 1207 | 21.58 | GC | C16 | 515 | 15.11 |
| 3 | HCC | C22 | 1623 | 18.03 | HCC | C22 | 1180 | 21.10 | HCC | C22 | 443 | 13.00 |
| 4 | CRC | C18-21 | 544 | 6.04 | CRC | C18-21 | 305 | 5.45 | CRC | C18-21 | 239 | 7.01 |
| 5 | EC | C15 | 290 | 3.22 | EC | C15 | 245 | 4.38 | BC | C50 | 179 | 5.25 |
| 6 | CNC | C70-72 | 289 | 3.21 | CNC | C70-72 | 158 | 2.82 | CNC | C70-72 | 131 | 3.84 |
| 7 | PC | C25 | 252 | 2.80 | PC | C25 | 143 | 2.56 | LK | C91-95 | 118 | 3.46 |
| 8 | LK | C91-95 | 251 | 2.79 | LK | C91-95 | 133 | 2.38 | PC | C25 | 109 | 3.20 |
| 9 | BC | C50 | 185 | 2.06 | BLC | C67 | 95 | 1.70 | EMC | C54 | 101 | 2.96 |
| 10 | LNC | C77 | 151 | 1.68 | LNC | C77 | 93 | 1.66 | LNC | C77 | 58 | 1.70 |
| Total | 7990 | 88.77 | Total | 5119 | 91.52 | Total | 3016 | 88.48 | ||||
The crude mortality rate during this period due to GC in Zhuanghe was 31.31 per 105; 43.47 per 105 in males and 18.91 per 105 in females. The difference in sex-specific incidence rates was statistically significant (χ2 = 264.82, P < 0.001); a higher rate was observed in males than in females with a ratio of 2.30. A decreasing trend in crude mortality rate was observed over the past 6 years (P < 0.001 in both sexes; P = 0.046 in males, P < 0.001 in females) (Table 4).
| Year | Total | Males | Females | |||||||||
| Cases | Crude | ASMR1 | ASMR2 | Cases | Crude | ASMR1 | ASMR2 | Cases | Crude | ASMR1 | ASMR2 | |
| 2005 | 352 | 38.51 | 27.94 | 32.74 | 224 | 48.47 | 33.31 | 42.08 | 128 | 28.32 | 21.75 | 23.86 |
| 2006 | 293 | 31.93 | 23.11 | 27.00 | 204 | 43.97 | 30.16 | 38.67 | 89 | 19.62 | 14.55 | 15.91 |
| 2007 | 276 | 29.95 | 21.79 | 25.78 | 202 | 43.37 | 29.26 | 38.55 | 74 | 16.24 | 12.50 | 13.54 |
| 2008 | 268 | 29.04 | 17.06 | 19.61 | 199 | 42.71 | 23.22 | 29.02 | 69 | 15.10 | 9.54 | 10.32 |
| 2009 | 272 | 29.71 | 16.20 | 18.74 | 202 | 43.74 | 21.82 | 28.07 | 70 | 15.42 | 8.99 | 9.52 |
| 2010 | 261 | 28.74 | 14.92 | 17.28 | 176 | 38.50 | 18.86 | 23.71 | 85 | 18.86 | 9.92 | 10.78 |
| Total | 1722 | 31.31 | 19.54 | 22.65 | 1207 | 43.47 | 25.42 | 32.18 | 515 | 18.91 | 12.35 | 13.32 |
| χ2 trend test | χ2 = 12.949, P < 0.001 | χ2 = 3.965, P = 0.046 | χ2 = 12.736, P < 0.001 | |||||||||
| APC | APC = -12.23%, P = 0.001 | APC = -11.09%, P = 0.002 | APC =-15.23%, P = 0.015 | |||||||||
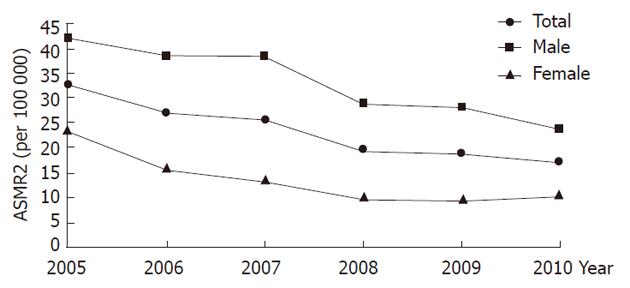
A progressive decrease in the world age-standardized mortality rate was noted in both genders (Figure 2 and Table 4): ASMR2 decreased steadily from 42.08/105 in 2005 to 23.71/105 in 2010 for males, and from 23.86/105 to 10.78/105 for females, with an average reduction of -11.09% for males (95% CI: -9.65% to -12.50%; P = 0.002) and -15.23% for females (95% CI: -11.71% to -18.62%; P = 0.015) per year. In general, ASMR2 decreased from 32.74 to 17.28 per 105 with an APC of -12.23% (95% CI: -10.94% to -13.90%; P = 0.001).
The minimum age group for GC death was 15-20 years. With increasing age, the mortality rate increased sharply, reaching a peak at approximately 80 years of age and declining thereafter. The median age was 71.00 years and the average age was 69.17 years. The cases in subjects over 50 years of age accounted for 91.70% of all deaths (Table 5).
| Age (yr) | Incidence | Mortality | ||||
| Males | Females | Total | Males | Females | Total | |
| 0-4 | ||||||
| 5-9 | ||||||
| 10-14 | ||||||
| 15-19 | 0.68 | 0 | 0.33 | |||
| 20-24 | 0.61 | 0.57 | 0.59 | 0 | 0 | 0 |
| 25-29 | 2.49 | 1.97 | 2.23 | 0.99 | 0.99 | 0.99 |
| 30-34 | 2.15 | 5.01 | 3.54 | 2.15 | 3.19 | 2.65 |
| 35-39 | 12.08 | 5.49 | 8.85 | 3.02 | 3.53 | 3.27 |
| 40-44 | 23.34 | 9.93 | 16.65 | 11.32 | 4.97 | 8.15 |
| 45-49 | 35.80 | 12.46 | 24.15 | 14.61 | 8.43 | 11.52 |
| 50-54 | 70.78 | 28.85 | 50.01 | 29.64 | 21.18 | 25.45 |
| 55-59 | 130.08 | 50.15 | 91.74 | 57.05 | 29.10 | 43.65 |
| 60-64 | 169.90 | 62.55 | 119.25 | 85.33 | 35.50 | 61.82 |
| 65-69 | 280.88 | 87.94 | 186.18 | 169.55 | 56.15 | 113.89 |
| 70-74 | 369.88 | 123.30 | 245.56 | 245.76 | 80.57 | 162.48 |
| 75-79 | 474.45 | 128.06 | 296.01 | 373.28 | 116.57 | 241.04 |
| 80-84 | 573.56 | 183.05 | 367.92 | 453.11 | 206.25 | 323.12 |
| 85+ | 341.65 | 129.97 | 224.60 | 414.00 | 175.46 | 282.10 |
In addition, we calculated the age-standardized mortality-incidence ratio (M/I ratio: ASR2/ASMR2) during different time periods. The M/I ratio decreased from 0.87 to 0.58 over a 6-year period. The worst ratio was recorded in 2005: 0.73 for males and 1.32 for females, followed by a steady decrease over the subsequent years with the M/I ratio falling to 0.53 for males and 0.73 for females in 2010 (Table 6).
GC is one of the most common cancers worldwide. There is substantial geographic variation regarding the incidence and mortality of GC. Studies specifically examining the population in high-risk areas should be very useful in potentially controlling this disease. Zhuanghe County, which is situated in the coastal area of the eastern Liaoning peninsula, is a rural area exhibiting a high GC mortality in north China. A series of epidemiological investigations and comprehensive preventive measures for GC have been conducted since 1984. Surveillance of cancer incidence and mortality rates has provided a guideline to identify the etiology and aid in the evaluation of the impact of intervention on the population. Our previous sampling data indicated the initial effects of GC intervention. However, the lack of an overall picture of GC remains due to the unavailability of cancer registry data covering the entire region prior to 2005. In this study, we reviewed the data regarding the incidence and mortality of GC in Zhuanghe County during the period of 2005-2010 based on the population-based registry in order to analyze the changing trends and to elucidate the underlying causes.
The results about the organ distribution of all cancers in Zhuanghe indicated that 80.74% of new cases originated from ten primary organ sites, the two major sites being lung (21.35%) and stomach (21.04%). Moreover, the ten major cancers accounted for 88.77% of all cancer-related deaths, with lung and stomach as the top two positions (29.81% and 19.13%). GC was the most common type of cancer in males and the second most common in females in the Zhuanghe region, and was the second leading cause of cancer death for both genders. All of the data indicated that GC remained a major health burden for the local population.
Globally, the incidence rate of GC is nearly twice as high in males as in females[1]; the male-to-female incidence ratio in Zhuanghe county was 2.80 (χ2 = 264.82, P < 0.001), and the mortality of GC in males was 2.30 times higher than in females (χ2 = 584.31, P < 0.001). There were gender differences in many types of cancer, which may be related to the different risk level for exposure to diet, smoking, drinking and occupation[18]. Investigation of genetic factors together with other intrinsic and extrinsic differences between the genders could potentially help reveal the relevant factors in oncogenesis, and lead to more effective prevention measures and disease control.
Regarding age-specific incidence and mortality, we found an overall increasing trend that corresponded with increasing age, peaking at age 80-84 years, and a declining trend for older men and women during this period. According to the data collected from 2001 to 2003, the peak in GC incidence and mortality occurred earlier[13] and the median and the average age were also increased. These differences were hypothesized to be related to preventive measures as well as the change of population composition such as population growth and aging.
In our study, we specifically analyzed the changing trends in GC rates in Zhuanghe, China, and found encouraging declines in both incidence and mortality. Between 2005 and 2010, GC incidence decreased with an APC of 4.82% in Zhuanghe. Moreover, a similar but more noticeable trend was observed in mortality (APC = -12.23%). The decreasing trends were in concordance with the results from various other reports in China. Wang et al[19] found that the estimated annual percentage change in GC incidence in Yangzhong was -2.96% in males and -2.86% in females. The APC change for GC incidence in Changle was reported to be -3.44% in men and -2.21% in women[20]. The report by Cui et al[21] demonstrated an APC of GC mortality in Kaifeng of approximately -2.92% in males and -3.37% in females. Although similar trends were observed, the amplitudes of the declines were not similar to those demonstrated by our data, which indicated a far more significant decrease among the comparable studies.
The descending trends of GC rates in other regions were mostly reported to be attributed to the “unplanned triumph” of improvement in sanitation, fresh fruit and vegetable consumption, and reduced H. pylori infection. It is commonly accepted that the incidence and mortality of GC in a region are related to both the economic status of the population and dietary habits[22-24]. In the past, residents in Zhuanghe had a low standard of living and were accustomed to eating highly salted food. However, currently, with economic development and increased knowledge regarding tumor prevention, residents have changed their dietary habits, and this potentially plays an important role in the descending trends of the disease. In 2010, Gross Domestic Product of Zhuanghe average per capita reached 54 348 RMB yuan - a 5.2-fold increase since 2000. Meanwhile, the rural health investment including environmental sanitation for water and housing has been increased by 23.8 times in the past decade[25], and the consequentially improved sanitary conditions may help reduce the prevalence of H. pylori infection, and the risk of GC development. Therefore, further research regarding preventive factors, such as eating habits, foods, prevalence of H. pylori infection, environmental factors, etc.[26-28] is warranted.
In addition to the above causes for the decreasing trends in GC, prevention and control measures were also taken in Zhuanghe, and these measures also play an important role in the encouraging declines of GC incidence in our study. In Zhuanghe, comprehensive control and etiological intervention through mass behavior interference and chemoprophylaxis in the high-risk populations have been conducted in pilot villages for many years by a research group from the First Affiliated Hospital of China Medical University (FAHCMU). With professional guidance by the researchers, knowledge of prevention and treatment of GC was disseminated for general residents by means of broadcasting, video, brochures and face-to-face conversation. In addition, the targeted high-risk population was treated promptly with antibiotics, Chinese herbal medicine and nutritional therapy based on H. pylori detection and gastroscopic and pathological examinations[29]. Our previous pilot survey demonstrated that these strategies are feasible and cost-effective for the treatment of gastric premalignant lesions and carcinoma in early stages, and a decrease in the mortality rate was observed in the intervened population at the initial period of prevention. The average mortality rate in the intervention groups (34.97/105) during the post-intervention period (1997-2000) was significantly lower than (59.31/105) in the pre-intervention period (1996) (P < 0.05)[30]. In the present study, we focused on trends at the population level. Interestingly, the same downward trend seen in the intervention groups was observed in the entire population. This study demonstrates that the preventive activities potentially contributed to alleviating the adverse effects of GC on the health and life of patients, even in the population as a whole.
Despite declines in both incidence and mortality of GC, we noted a dissociation phenomenon, i.e., an APC decrease was greater for mortality compared with incidence. It was hypothesized that early diagnosis and early treatment would play an important role in the dissociation phenomenon between incidence and mortality. The data suggested the need for further promotion of GC screening to enable early diagnosis. In this study, we also analyzed the M/I ratio in Zhuanghe. The M/I ratio, which compares the number of deaths attributed to a specific cancer and the number of incident cases in the same time period, can be interpreted as an indirect indicator of general survival if registration is complete and there are no marked temporal changes in incidence rates[31]. The age-standardized M/I ratio steadily decreased in both genders, which indicated a prolonged survival; hence the decrease in mortality was not caused by the fall in incidence rate alone, but by other factors, including earlier diagnosis or improved treatment. Since 1997, more than 15 000 people have received GC screening by the research group from FAHCMU through a two-round GC screening strategy, and this large-scale population screening program extensively covered 70 villages of Zhuanghe region. Through unremitting efforts for years, the detection rate of early GC reached 60%-80% and has been increasing yearly. The GC patients screened with pathological confirmation will be sent to hospitals for treatment, and their postoperative five-year survival rate was above 90%[7]. Thus, such a population screening program may contribute to the above-mentioned dissociation phenomenon and prolonged survival of the patients. Furthermore, the age-standardized M/I ratio was lower in the male population, suggesting that the survival rate was higher in males than in female patients after treatment.
This study describes the changes in incidence and mortality rates in the entire population of Zhuanghe over the past 6 years, which may not fully reflect broader population trends; however, our observations of the short-term changes potentially form the basis for future analysis. In concert with our previous studies, we described a general picture of GC patterns and changing trends in Zhuanghe. In addition, despite a significant declining trend, the age-standardized incidence (ASR1: 26.84/105vs 17.06/105) and mortality (ASMR1: 14.92/105vs 11.67/105) remained higher than the national level in China[32,33]. Therefore, in future studies, continuous monitoring over a longer period of time is needed to not only identify whether the declining trends persist, but also to acquire a more comprehensive understanding of GC in this region. Accordingly, effective prevention and treatment strategies would be further developed, which will greatly benefit the residents in high-risk areas. Moreover, researches regarding the impact of genetics, the environment, and their interaction are warranted to fully elucidate the disease etiology.
Gastric cancer (GC) is one of the most common cancers worldwide. The geographical distribution of GC is characterized by wide regional disparity. Monitoring and studying the incidence as well as mortality at the population level in high-risk areas should be very helpful in controlling this disease in the future.
Surveillance of cancer incidence and mortality provides important epidemiological information, enabling development of cancer prevention and control strategies. Several population-based cancer registries provided data on cancer rates in China, however, most of which were established in the affluent big cities rather than in the poor rural counties. In this study, the data regarding the incidence and mortality of GC in Zhuanghe County, a rural area of China, were reviewed based on the population-based registry, which provided a general picture of the GC distribution in a rural high-risk area.
The distribution of GC has substantial geographic variation, thus, studies concerning the population in high-risk areas should be more meaningful in potentially controlling this disease. The present study, for the first time, examined all-cancers distribution and temporal trends of GC in Zhuanghe and explored the possible influencing factors. Based on the findings in the registry studies, the control strategies of GC could be further developed in local areas, which may be also instructive and meaningful to cancer prevention of other similar areas in China.
There is a significant global variation in the distribution of GC. The findings of the study would be helpful for the development of general and specific cancer prevention and control strategies to benefit the residents in the high- risk areas both locally and nationally.
Age-standardized incidence rates and age-standardized mortality rates are used to compare the incidence or mortality rates of places without being skewed by the difference in age distributions from place to place.
The authors studied the patterns and time trends of gastric cancer in terms of incidence and mortality in Zhuanghe region at population level and investigated the influencing factors of the changing trends. Findings from this study showed a downward trend of both incidence and mortality that may be due to the raised economic level along with implementation of prevention and control measures. It enriched epidemiological data of GC and offered reference to the other high-risk areas of China to control the disease based on population-level evidences.
Peer reviewer: Ki-Baik Hahm, MD, PhD, Professor, Gachon Graduate School of Medicine, Department of Gastroenterology, Lee Gil Ya Cancer and Diabetes Institute, Lab of Translational Medicine, 7-45 Songdo-dong, Yeonsu-gu, Incheon 406-840, South Korea
S- Editor Lv S L- Editor Ma JY E- Editor Li JY
| 1. | Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69-90. [PubMed] |
| 2. | Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893-2917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11128] [Cited by in RCA: 11836] [Article Influence: 845.4] [Reference Citation Analysis (4)] |
| 3. | Yeh JM, Goldie SJ, Kuntz KM, Ezzati M. Effects of Helicobacter pylori infection and smoking on gastric cancer incidence in China: a population-level analysis of trends and projections. Cancer Causes Control. 2009;20:2021-2029. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Yang L. Incidence and mortality of gastric cancer in China. World J Gastroenterol. 2006;12:17-20. [PubMed] |
| 5. | Wen Z, Wang Q, Huang H, Liu YH, Sun GP, Li D, Pan BC, Yuan Y. Progress on the Work of Early Detection and Treatment for Gastric Cancer in Zhuanghe, Liaoning Province. Zhongguo Zhongliu. 2009;18:735-737. |
| 6. | Sun ZX, Bai XW, Lin HZ. Epidemiological investigation of natural population in high- and low-risk areas of gastric cancer. Zhongguo Yike Daxve Xvebao. 1988;17:23-25. |
| 7. | Yuan Y, Zhang YC. A report of prevention and control scene for gastric cancer in Zhuanghe region, Liaoning Province. Zhongguo Zhongliu. 2009;18:14-17. |
| 8. | Yuan Y, Lin H, Zhang Y. [Study on the mutagenicity of salted pork from high risk area of stomach cancer and its relation to pathological changes of gastric mucosa]. Zhonghua Zhongliu Zazhi. 1996;18:270-272. [PubMed] |
| 9. | Gong YH, Wang Y, Yuan Y. Distribution of Helicobacter pylori in north China. World J Gastroenterol. 2005;11:3523-3527. [PubMed] |
| 10. | Liu J, Sun LP, Gong YH, Yuan Y. Risk factors of precancerous gastric lesions in a population at high risk of gastric cancer. Chin J Cancer Res. 2010;22:267-273. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Liu HJ, Guo XL, Dong M, Wang L, Yuan Y. Association between pepsinogen C gene polymorphism and genetic predisposition to gastric cancer. World J Gastroenterol. 2003;9:50-53. [PubMed] |
| 12. | Sun LP, Guo XL, Zhang Y, Chen W, Bai XL, Liu J, Yuan Y. Impact of pepsinogen C polymorphism on individual susceptibility to gastric cancer and its precancerous conditions in a Northeast Chinese population. J Cancer Res Clin Oncol. 2009;135:1033-1039. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Xiao W, Zhang WG, Wang RR, Liu HY, Sun LH. Analysis of incidence and mortality of gastric cancer in sample areas of Zhuanghe. Zhongguo Weisheng Tongji. 2005;22:119-120. |
| 14. | Bai LG, Li YH. Analysis of gastric cancer incidence during 1998-2004 in Zhuanghe country. Zhongguo Weisheng Tongji. 2005;22:223. |
| 15. | Jensen OM, Storm HH. Cancer registration: principles and methods. Reporting of results. IARC Sci Publ. 1991;108-125. [PubMed] |
| 16. | Hankey BF, Ries LA, Kosary CL, Feuer EJ, Merrill RM, Clegg LX, Edwards BK. Partitioning linear trends in age-adjusted rates. Cancer Causes Control. 2000;11:31-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 62] [Reference Citation Analysis (1)] |
| 17. | Siesling S, van Dijck JA, Visser O, Coebergh JW. Trends in incidence of and mortality from cancer in The Netherlands in the period 1989-1998. Eur J Cancer. 2003;39:2521-2530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 53] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Rutegård M, Shore R, Lu Y, Lagergren P, Lindblad M. Sex differences in the incidence of gastrointestinal adenocarcinoma in Sweden 1970-2006. Eur J Cancer. 2010;46:1093-1100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 19. | Wang JM, Xu B, Hsieh CC, Jiang QW. Longitudinal trends of stomach cancer and esophageal cancer in Yangzhong County: a high-incidence rural area of China. Eur J Gastroenterol Hepatol. 2005;17:1339-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Tian J, Chen JS. Time trends of incidence of digestive system cancers in changle of China during 1988-2002. World J Gastroenterol. 2006;12:4569-4571. [PubMed] |
| 21. | Cui YL, Fu L, Wang WL, Geng ZX, Ma S, Li HB, Lu WQ. An Analysis on Mortality of Gastric Cancer from 1988 to 2005 in Kaifeng, Henan Province. Zhongguo Zhongliu. 2009;18:373-374. |
| 22. | Bertuccio P, Chatenoud L, Levi F, Praud D, Ferlay J, Negri E, Malvezzi M, La Vecchia C. Recent patterns in gastric cancer: a global overview. Int J Cancer. 2009;125:666-673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 446] [Cited by in RCA: 484] [Article Influence: 30.3] [Reference Citation Analysis (1)] |
| 23. | Baastrup R, Sørensen M, Hansen J, Hansen RD, Würtzen H, Winther JF. Social inequality and incidence of and survival from cancers of the oesophagus, stomach and pancreas in a population-based study in Denmark, 1994-2003. Eur J Cancer. 2008;44:1962-1977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Key TJ, Allen NE, Spencer EA, Travis RC. The effect of diet on risk of cancer. Lancet. 2002;360:861-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 325] [Cited by in RCA: 301] [Article Influence: 13.1] [Reference Citation Analysis (0)] |
| 25. | Gao L. Dalian Statistical Yearbook. Beijing: China Statistics Press 2010; 728. |
| 26. | González CA, López-Carrillo L. Helicobacter pylori, nutrition and smoking interactions: their impact in gastric carcinogenesis. Scand J Gastroenterol. 2010;45:6-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Machida-Montani A, Sasazuki S, Inoue M, Natsukawa S, Shaura K, Koizumi Y, Kasuga Y, Hanaoka T, Tsugane S. Association of Helicobacter pylori infection and environmental factors in non-cardia gastric cancer in Japan. Gastric Cancer. 2004;7:46-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 118] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 28. | Kim HJ, Kim MK, Chang WK, Choi HS, Choi BY, Lee SS. Effect of nutrient intake and Helicobacter pylori infection on gastric cancer in Korea: a case-control study. Nutr Cancer. 2005;52:138-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 29. | Yuan Y, Zhou BS, Gao H, Qu FX, Wang XJ. Implement of comprehensive intervention strategy for high risk population in high risk area with gastric cancer. Zhongguo Zhongliu. 2000;9:118-119. |
| 30. | Guo HQ, Guan P, Shi HL, Zhang X, Zhou BS, Yuan Y. Prospective cohort study of comprehensive prevention to gastric cancer. World J Gastroenterol. 2003;9:432-436. [PubMed] |
| 31. | Bhurgri Y, Bhurgri A, Hasan SH. Comparability and Quality Control in Cancer Registration; Karachi (data monitoring 1995-2001). J Pak Med Assoc. 2002;52:301-307. [PubMed] |
| 32. | Li GL, Chen WQ. Representativeness of population-based cancer registration in China--comparison of urban and rural areas. Asian Pac J Cancer Prev. 2009;10:559-564. [PubMed] |
| 33. | Chen WQ, Zhang SW, Zheng RS, Li GL, Zou XN, Zhao P. A Report of Cancer Incidence and Mortality from 38 Cancer Registries in China, 2007. Zhongguo Zhongliu. 2011;20:162-169. |