INTRODUCTION
Neurofibromatosis type 1 (NF1) or Von Recklinghau-sen’s disease is an autosomal dominant genetic disorder with an incidence of 1 in 2600-3000 individuals[1,2]. Neurofibromas are benign tumors arising from Schwann cells, caused by a mutation of the tumor suppressor gene NF1[3,4]. Diagnosis of NF1 is made on clinical criteria, originally described by the National Institutes of Health Consensus Development Conference in 1987[5]. The most typical features are café-au-lait macules and neurofibromas of the skin. Other organ systems can also be affected, including the cardiovascular system, eyes, bones and the gastrointestinal system. In this report we present a case of a patient with NF1 and recurrent abdominal complaints, caused by a neurofibroma in the cecal wall.
CASE REPORT
A 69-year-old woman with a history of Von Recklinghausen’s disease was presented to the gastroenterologist with weight loss (9 kg in 3 mo), dysphagia and anorexia for several weeks. She also suffered from intermittent central abdominal pain for more than 1 year. There was no history of nausea, vomiting or pyrosis. For many years she had constipation, without visible blood loss or melaena. She underwent an appendectomy and a laparoscopic cholecystectomy at the age of 20 and 60, respectively. Despite her NF1, which affected her skin and bones, no other medical history was known. She did not use any medication. Physical examination revealed no abnormalities of the abdomen, other than neurofibromas on her skin. Laboratory studies were normal.
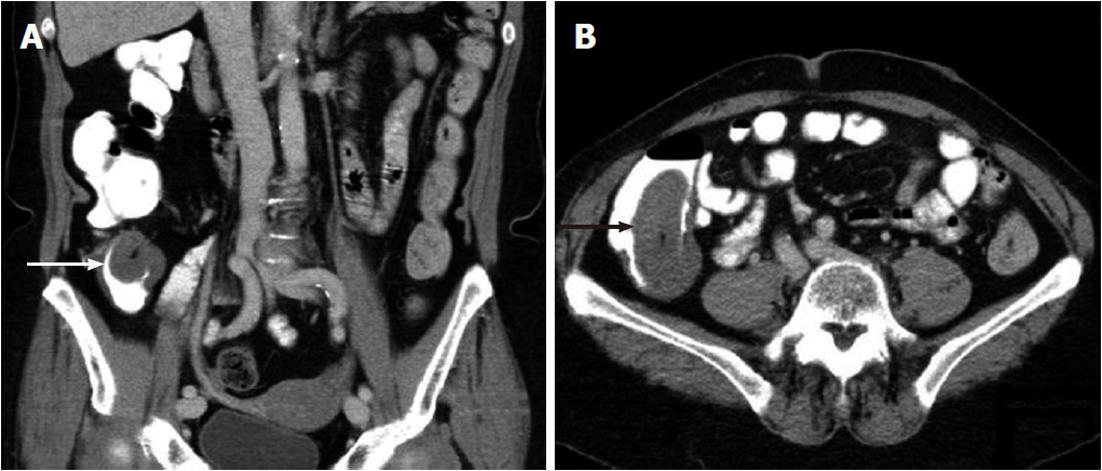
Since the most prominent complaints were dysphagia and weight loss, a gastroduodenoscopy was performed, which did not show any abnormalities of the esophagus, stomach or duodenum. An abdominal ultrasound, however, demonstrated a 3.4 cm large tumorous process in the right lower quadrant. A computed tomography-scan of the abdomen showed the same process, localized in the cecal wall, invaginating into the cecal lumen (Figure 1). There were no signs of bowel obstruction or metastasis in mesenterial lymph nodes or liver.
Figure 1 Coronary (A) and transversal coupe (B) of abdominal computed tomography in a patient with neurofibromatosis type 1 with a cecal mass (arrows).
Before a planned colonoscopy the clinical presentation deteriorated; our patient developed severe abdominal pain and a laparoscopic procedure was performed. Macroscopic inspection of the cecum revealed a palpable tumor inside the lumen. Further visual inspection of the abdominal cavity revealed no pathologic findings, such as mesenterial masses or liver metastasis. A laparoscopic right-sided hemicolectomy with an extracorporeal primary side-to-side anastomosis was performed. She recovered well and was discharged after five days. Soon her normal appetite returned, she regained her normal weight and had no more abdominal pain.
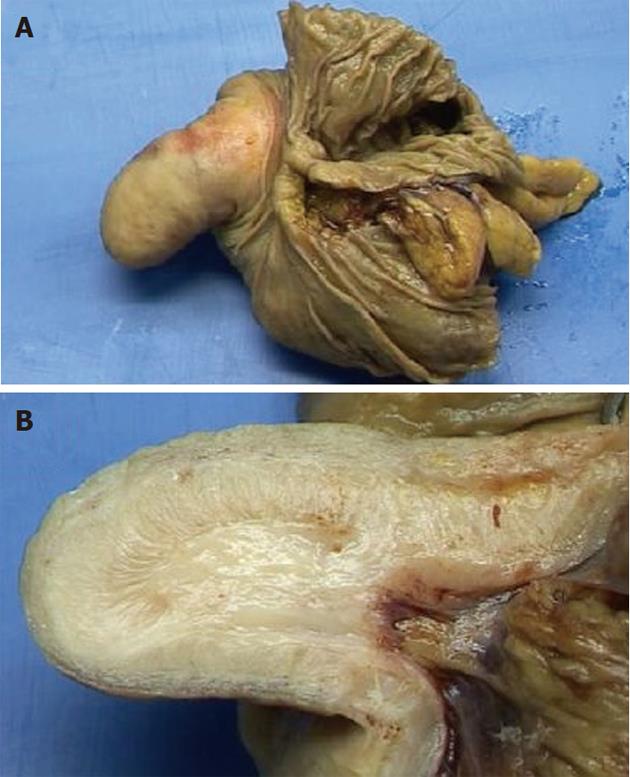
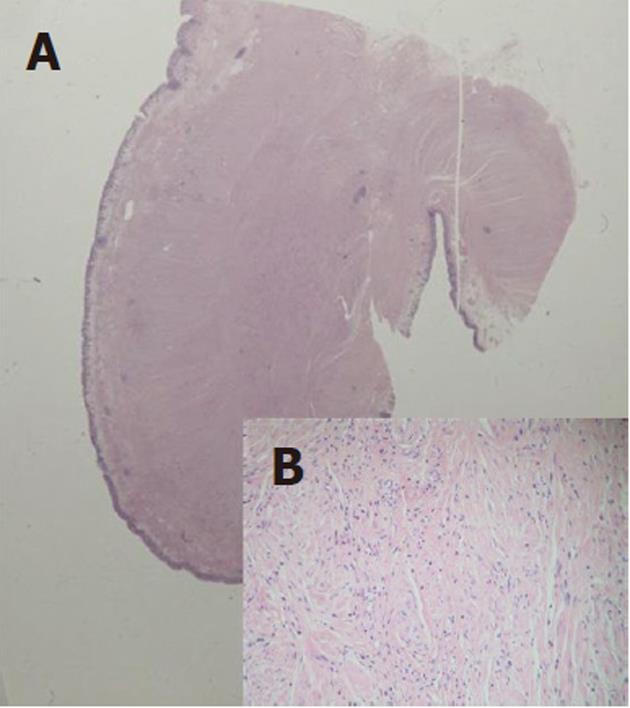
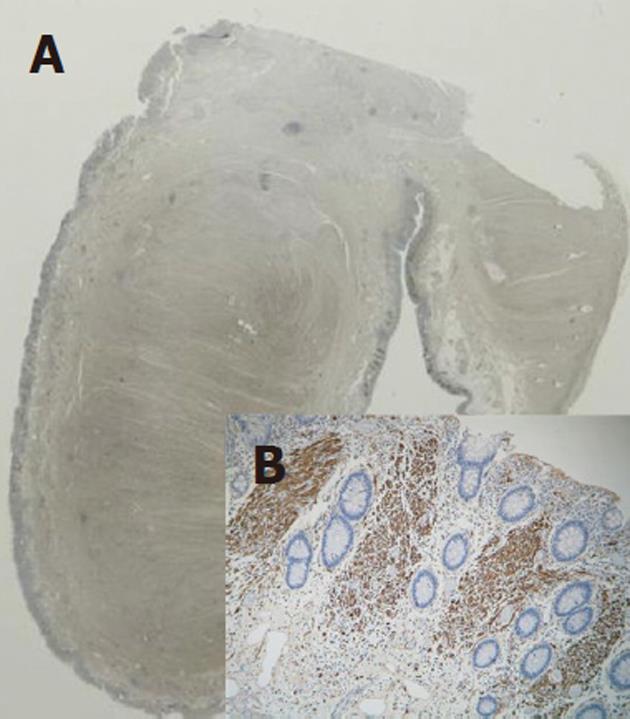
Pathologic study of the specimen revealed a polypous cecal tumor of 3 by 5.5 cm (Figure 2), with a submucosal and intramucosal growing pattern. The lesion contained foci of spindle cells with a bundle-like growing pattern. Ganglion cells were absent. The lesion was positive for CD34, SMA and S100, but negative for P53. The morphological and immunohistochemical characteristics were consistent with the diagnosis of neurofibroma type 1 (Figures 3 and 4). The tumor was negative for CD117 and DOG-1 thus excluding a diagnosis of gastrointestinal stromal tumors (GIST).
Figure 2 Opened resection specimen (A) and cut surface of the polyp (B).
Figure 3 Overview of the polyp (A) and detail of the submucosal tumor (B), HE staining; original magnification, × 100.
Figure 4 Overview of the polyp (A) and detail of the submucosal tumor (B), S100 staining; original magnification, × 100.
DISCUSSION
NF1 can affect multiple organ systems, causing skin lesions, malignant peripheral nerve sheath tumors, intra-cranial tumors and cranial vascular deformities, optic pathway gliomas, bone deformities, heart problems, hypertension and abdominal tumors[1].
Five categories of abdominal neoplasms in association with NF1 have recently been described[6]. The first category is benign or malignant neurogenic tumors, with neurofibromas as the most common and often asymptomatic (65%) neoplasm, originating from the mesenteric plexus. Several cases with abdominal neurofibroma have been described[7-11]. Other neurogenic tumors are plexiform neurofibromas, malignant peripheral sheath tumors and ganglioneuromas[6]. The second category is neuroendocrine tumors as carcinoids, pheochromocytomas and paragangliomas. In particular ampulla of Vater carcinoids are associated with NF1[12,13]. The third category is GIST, which have been reported in up to one third of all patients with NF1[14,15]. The pathogenesis of GIST is different from sporadic tumors[3]. The fourth category is embryonal tumors, such as Wilms tumor, neuroblastoma and rhabdomyosarcoma. Finally, adenocarcinomas of the gastrointestinal tract have been detected in patients with NF1. Wood et al[16] (2005) reported a patient with NF1 and colon carcinoma and presented older reports suggesting an association between NF1 and colon carcinoma.
Gastrointestinal involvement of NF1 in patients is reported in 25% of all cases, almost always affecting the upper gastrointestinal tract. The jejunum and stomach are common sites of neurofibromas or associated tumors such as GISTs and ampulla of Vater carcinoids[12,13]. Oesophagus and colon are rarely involved[7]. We found 5 case reports and 1 patient in a series of 10 patients with a colonic neurofibroma[7-11,17]. The most common presenting signs are abdominal pain, gastrointestinal bleeding, obstruction and palpable masses. The presence of one or more intestinal neurofibromas, however, does not imply that a patient has NF1. Only in 15% of cases where intestinal neurofibromas were found was the patient was diagnosed with NF1[7].
Pathologic study of a neurofibroma in the gastrointestinal tract reveals a tumor consisting of a mixture of spindle cells with wavy nuclei and strands of collagen as well as Schwann cells, perineurial fibroblasts, endothelial cells and mast cells. Tumors positive for S100 are very suggestive for neurofibromas. These tumors must be distinguished from GISTs, schwannomas, perineuromas and leiomyomas[18].
In this report we present a case of a patient with NF1 and recurrent abdominal complaints caused by a large cecal neurofibroma. Gastrointestinal involvement of NF1 can be found in patients with NF1 and abdominal pain, particularly in the upper gastrointestinal tract, but also colonic localisation has to be considered. Evaluation by endoscopic assessment or radiological imaging of the gastrointestinal tract is advised. Also a higher incidence of gastrointestinal malignancies in patients with NF1 has to be considered.