Published online Jul 21, 2011. doi: 10.3748/wjg.v17.i27.3235
Revised: February 12, 2011
Accepted: February 19, 2011
Published online: July 21, 2011
AIM: To investigate the influence of irritable bowel syndrome (IBS)-like symptoms on treatment outcomes with pantoprazole in gastroesophageal reflux disease (GERD) in a real life setting.
METHODS: For this prospective, open-label, multinational, multicentre study, 1888 patients assessed by the investigators as suffering from GERD were recruited. The patients were additionally classified as with or without IBS-like symptoms at baseline. They were treated with pantoprazole 40 mg once daily and completed the Reflux Questionnaire™ (ReQuest™) short version daily. Response rates and symptom scores were compared after 4 and 8 wk of treatment for subgroups defined by the subclasses of GERD [erosive (ERD) and non-erosive reflux disease (NERD)] and the presence of IBS-like symptoms.
RESULTS: IBS-like symptoms were more prevalent in NERD than in ERD (18.3% vs 12.7%, P = 0.0015). Response rates after 4 and/or 8 wk of treatment were lower in patients with IBS-like symptoms than in patients without IBS-like symptoms in both ERD (Week 4: P < 0.0001, Week 8: P < 0.0339) and NERD (Week 8: P = 0.0088). At baseline, ReQuest™“lower abdominal complaints” symptom scores were highest in NERD patients with IBS-like symptoms. Additionally, these patients had the strongest symptom improvement after treatment compared with all other subgroups.
CONCLUSION: IBS-like symptoms influence treatment outcome and symptom burden in GERD and should be considered in management. Proton pump inhibitors can improve IBS-like symptoms, particularly in NERD.
- Citation: Mönnikes H, Heading RC, Schmitt H, Doerfler H. Influence of irritable bowel syndrome on treatment outcome in gastroesophageal reflux disease. World J Gastroenterol 2011; 17(27): 3235-3241
- URL: https://www.wjgnet.com/1007-9327/full/v17/i27/3235.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i27.3235
Complaints in the lower abdomen associated with altered stool habits were commonly considered the leading characteristic of irritable bowel syndrome (IBS). However, despite the overlap between gastroesophageal reflux disease (GERD) and IBS being recognised for more than 20 years[1-3], there is still much debate about the pathophysiology and clinical management of lower abdominal complaints in patients with GERD[4-7]. Two theoretical frameworks have been proposed to account for the high prevalence (up to 71%[4,8,9]) of IBS symptoms in GERD patients[8,10].
The first defines GERD and IBS as distinct disorders that share common underlying mechanisms [e.g. gastrointestinal (GI) dysmotility[9] or visceral hypersensitivity[7]] in symptom genesis. In contrast, the second theory integrates IBS-like symptoms into the spectrum of GERD complaints, and is supported by evidence that shows that IBS-like symptoms improve after the administration of proton pump inhibitors (PPIs) for the treatment of GERD[11-14].
Interestingly, the prevalence of IBS-like symptoms[15-17], symptom burden[15], and treatment response following PPI administration[18,19] differ among patients with erosive GERD (ERD) and non-erosive GERD (NERD). Furthermore, current data suggest that the presence of IBS-like symptoms unfavourably affects treatment outcome with PPIs in some patients with GERD[8,20].
Given that symptom resolution is the primary goal of treatment for both physicians and patients, identifying and understanding the spectrum of symptoms influencing the treatment outcome in patients with GERD seen in routine clinical practice is essential for providing optimal primary patient care. We therefore designed a study to closely resemble the conditions of ordinary clinical practice to investigate these issues of practical clinical concern in the management of GERD. The aim of the current paper is to evaluate the influence of the presence of IBS-like symptoms on treatment response to the PPI pantoprazole in patients with GERD (including both ERD and NERD) in a real-life setting.
This prospective, open-label, phase III study (BY1023/M3-341, ClinicalTrials.gov Identifier: NCT00312806) used a pragmatic trial design to assess the effectiveness of treatment with pantoprazole in managing GI symptoms in patients considered by physicians to have both GERD and IBS-like symptoms. A pragmatic trial design (as opposed to an explanatory trial) was chosen for this study to reflect variations among patients and doctors in real clinical settings, thus more accurately reflecting patients within the community in whom the treatment will be applied and optimising the applicability of the trial findings to those clinical settings[21,22]. The current study was conducted worldwide in 167 centres in 21 countries (Argentina, Australia, Austria, Belgium, Brazil, Canada, France, Germany, Hong Kong, India, Italy, Malaysia, Mexico, Poland, Singapore, South Africa, South Korea, Spain, Switzerland, Taiwan, and the United Kingdom) according to ICH-GCP guidelines. Ethics approval was obtained locally by all participating centres.
Patients aged ≥ 18 years (≥ 21 years in Argentina) were included if they were considered by the investigator to have symptoms of GERD and to likely comply with requirements for the completion of the ReQuest™. All patients provided written informed consent prior to participation.
Patients were excluded if they: had a history of Zollinger-Ellison syndrome or other gastric hypersecretory condition; were suffering from acute peptic ulcer and/or ulcer complications, inflammatory bowel disease, or other severe concomitant diseases; or had acid lowering surgery or any other surgery of the esophagus and/or upper gastrointestinal tract (excluding polypectomy and cholecystectomy). Those who had used acid suppressing medication in the last 7-10 d prior to enrolment, or any medication for Helicobacter pylori eradication during the last 28 d prior to the study were also excluded, as were those who had received systemic glucocorticoids or non-steroidal anti-inflammatory drugs including COX 2 inhibitors more than 5 d on demand but not more than 3 consecutive days during the last 28 d (with the exception of regular intake of acetylsalicylic acid in dosages up to 163 mg/d). Medications for the relief of acid-related symptoms, and systemic glucocorticoids or non-steroidal anti-inflammatory drugs, were not permitted during the study.
At baseline, all patients underwent upper GI endoscopy to determine whether they had ERD or NERD; the grade of GERD was determined according to the LA classification for all patients[23]. During this visit, the investigator also enquired about the presence of symptoms that would be consistent with IBS and answered “yes”, “no”, or “I do not know” to the question: “Is it possible that this patient does not only suffer from GERD-related symptoms, but also from symptoms caused by irritable bowel syndrome (IBS)?”.
Enrolled patients were treated with the PPI pantoprazole-Na, 40 mg, provided as an oral enteric-coated tablet, to be taken one hour before breakfast once daily for eight weeks. During the eight-week period, three study visits were performed: visit 0 (V0, baseline), visit 1 (V1) after four weeks of treatment (Week 4), and visit 2 (V2) after eight weeks of treatment (Week 8).
Patients completed the ReQuest™ at baseline and then daily starting on Day 1 (the day after V0), and continuing until V2 on Day 56. The ReQuest™ is a fully validated and easy-to-handle self-administered symptom assessment tool reliable for the evaluation of treatment effects in ERD and NERD[11,24-27]. It comprises 67 items assigned to six dimensions of GERD: acid complaints (e.g. heartburn, acid regurgitation, and esophageal or upper abdominal burning); upper abdominal/stomach complaints (e.g. upper abdominal pressure, pain or burning, feeling or fullness or incomplete bowel evacuation, and upper or lower back pain); lower abdominal/digestive complaints (e.g. pressure, cramps or pain in the lower abdomen, flatulence, diarrhoea and constipation); nausea; sleep disturbances; and other complaints[28]. For each dimension, symptom intensity is assessed on a 100 mm visual analogue scale (VAS; ranging from “not at all” to “extremely severe”) and symptom frequency is measured using a 7-point Likert scale (ranging from “0” to “more than 10 times per day” or “continuously”). The ReQuest™ also includes a question about general well-being, evaluated using a VAS ranging from “wonderful” to “extremely poor”.
The dimensions of the ReQuest™ can be grouped into two subscales: ReQuest™-GI, which includes acid complaints, upper abdominal/stomach complaints, lower abdominal/digestive complaints, and nausea; and ReQuest™-WSO, comprising general well-being, sleep disturbances, and other complaints[28]. Each dimension is weighted, resulting in the following score ranges: (1) ReQuest™ total score: 0 to 46.28; (2) ReQuest™-GI: 0 to 30.77; and (3) ReQuest™-WSO: 0 to 15.51.
The score range of the two weighted individual dimensions of special interest, i.e. “acid complaints” and “lower abdominal complaints”, is 0 to 7.692. Patients were considered to have responded to treatment (responders) if their ReQuestTM-GI score was below 1.6[28] over three consecutive days prior to the two scheduled visits at Week 4 and Week 8.
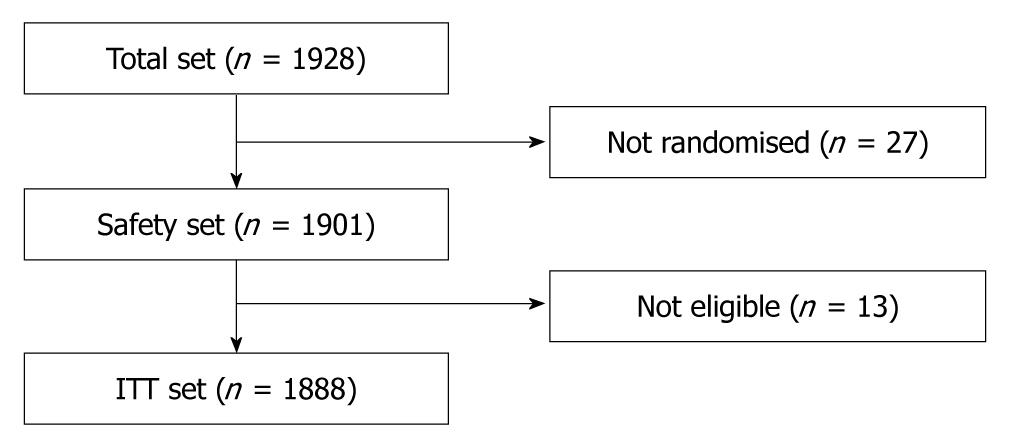
The sample size was calculated based on response rates seen in previous studies after 8 wk of treatment and envisaged a total of 2000 patients, approximately half with and half without esophagitis. A two-sided 95% confidence interval for a single proportion using the large sample normal approximation was expected to extend 0.019 from the observed proportion for an expected proportion of 0.100 in patients with esophagitis (sample size 1000) and 0.025 from the observed proportion for an expected proportion of 0.200 in patients without esophagitis (sample size 1000). Subsequently, a total of 1928 outpatients were screened, resulting in an intention-to-treat (ITT) population of 1888 patients.
Response rates were calculated at Week 4 and Week 8, and baseline scores and the pre-post differences (baseline to Week 4 and Week 8) were determined for the individual dimensions “acid complaints” and “lower abdominal complaints” of the ReQuest™-GI. Subgroup analyses were performed based on the presence or absence of esophagitis (i.e. ERD or NERD), IBS-like symptoms, and the combination thereof. The comparison of the response rates between these subgroups was performed using Fisher’s exact test. The baseline scores were compared with the Wilcoxon rank sum test, the pre-post differences with the Wilcoxon signed rank test.
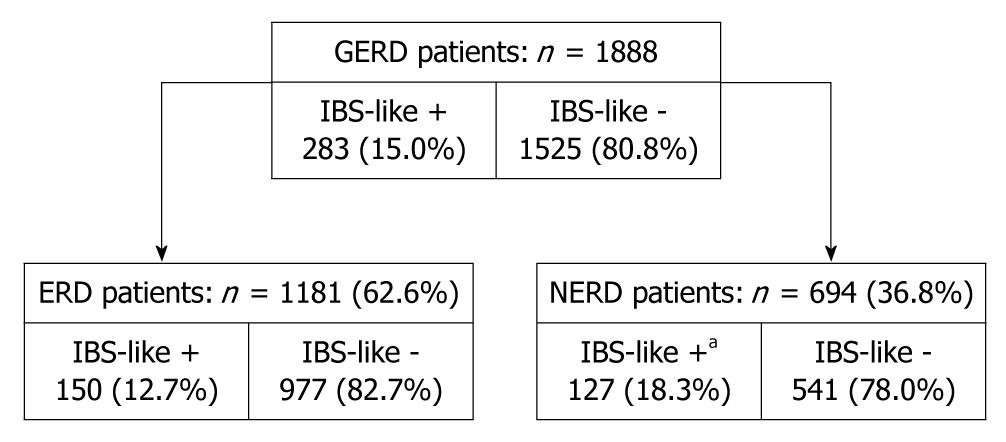
In total, 1928 outpatients were recruited in 167 centres in 21 countries worldwide; 27 patients were not randomised and 13 were not eligible for inclusion, resulting in an ITT population of 1888 patients with GERD (Figure 1). Table 1 presents patient demographic and baseline characteristics; percentages do not equal 100% due to missing values. In total, 694 patients (36.8%) were diagnosed with NERD and 1181 (62.6%) with ERD. Of the ERD patients, 680 (57.6%) had esophagitis grade A, 381 (32.3%) grade B, and 97 (8.2%) grade C. Esophagitis grade D was diagnosed in 23 ERD patients (1.9%). Of the 1888 GERD patients, 283 presented with IBS-like symptoms (15.0%) and 1525 presented without those symptoms (80.8%). IBS-like symptoms were significantly more frequent in NERD (18.3%) than in ERD patients (12.7%, P = 0.0015; Figure 2).
| Age (yr), mean (SD) | 47 (14.3) |
| Height (cm), mean (SD) | 167.5 (9.6) |
| Weight (kg), mean (SD) | 74.2 (15.8) |
| BMI (kg/m2), mean (SD) | 26.4 (4.8) |
| Gender, n (%) | |
| Female | 978 (51.8) |
| Male | 910 (48.2) |
| Esophagitis, n (%) | |
| Non-erosive | 694 (36.8) |
| Grade A | 680 (36.0) |
| Grade B | 381 (20.2) |
| Grade C | 97 (5.1) |
| Grade D | 23 (1.2) |
| Ethnic origin, n (%) | |
| White | 1326 (70.2) |
| Asian | 352 (18.6) |
| Other | 167 (8.8) |
| Black | 43 (2.3) |
| Smoker, n (%) | |
| Never | 1179 (62.4) |
| Former | 360 (19.1) |
| Current | 349 (18.5) |
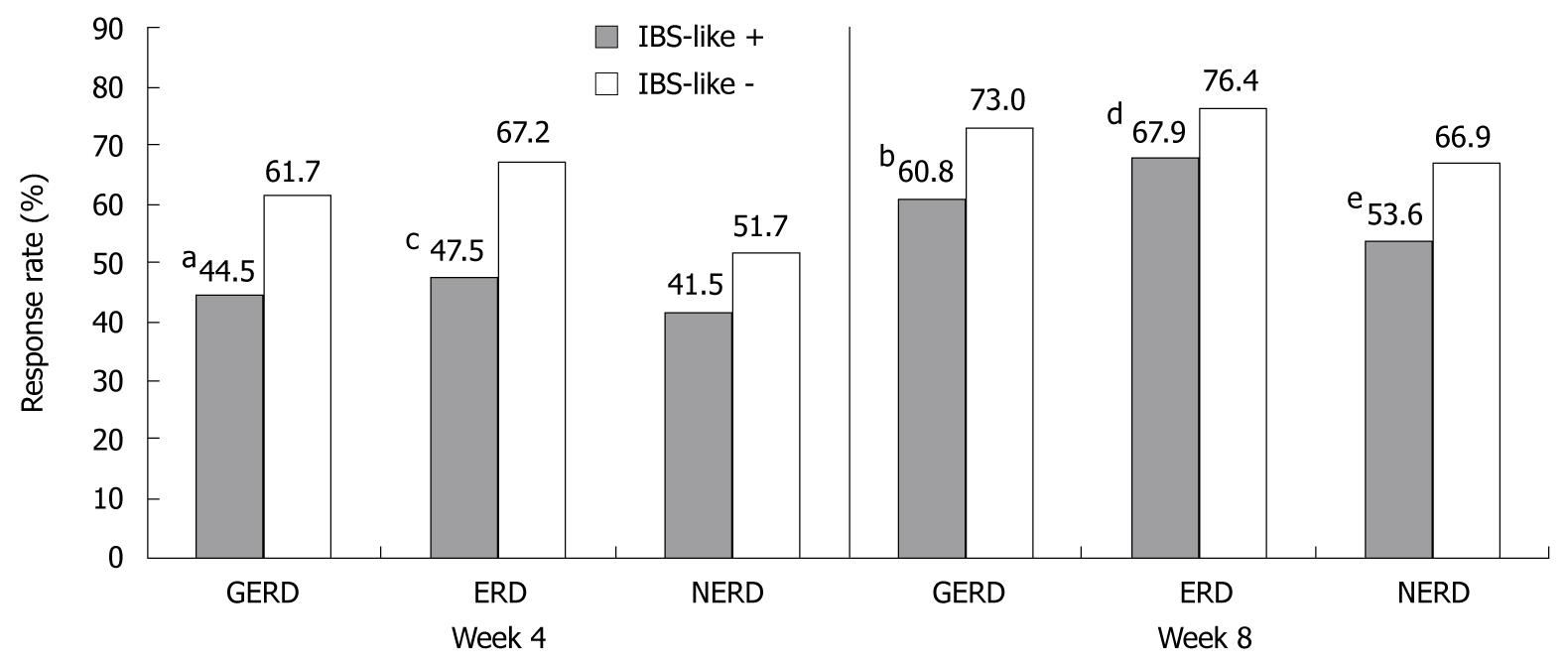
In total, 58.9% of patients with GERD responded to pantoprazole treatment at Week 4; this increased to 71.2% of patients at Week 8. Response rates were significantly higher for ERD patients than for NERD patients at both Week 4 (64.6% vs 49.2%, P < 0.0001) and Week 8 (75.5% vs 64.5%, P < 0.0001). Both patients with and without IBS-like symptoms responded to treatment at Weeks 4 and 8 (Figure 3); however, response rates in GERD patients without IBS symptoms were significantly higher than in those with IBS-like symptoms at both time points (both P < 0.0001; Figure 3). Similarly, for patients with either ERD (Week 4: P < 0.0001; Week 8: P < 0.0339) or NERD (Week 8: P = 0.0088) response rates were higher if IBS-like symptoms were absent than if they were present (Figure 3).
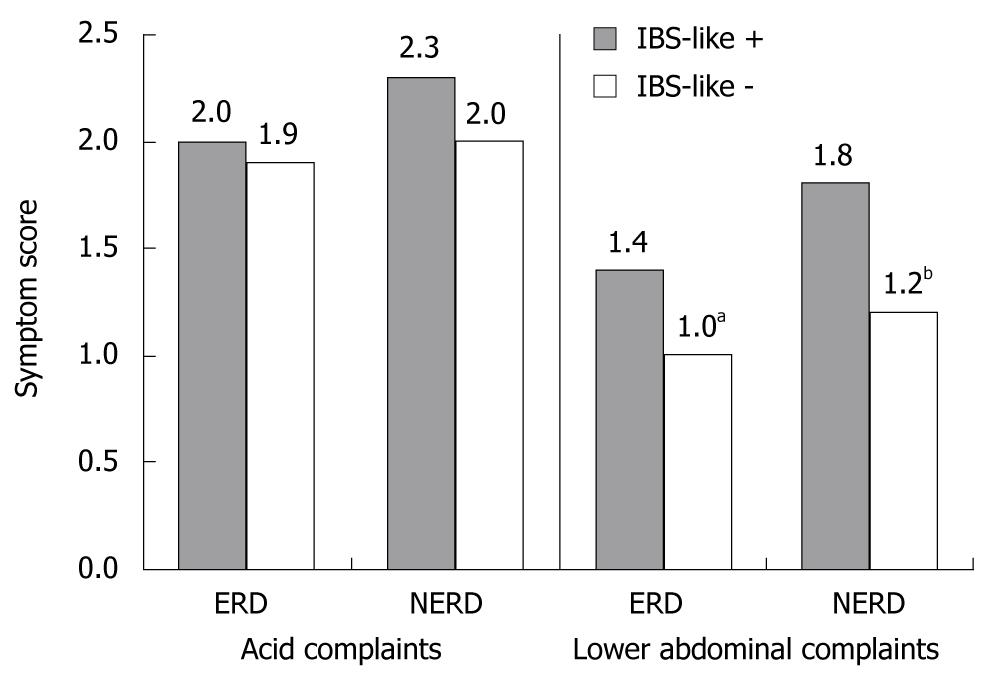
At baseline, the symptom scores for the ReQuest™ dimension “acid complaints” were 2.0 for both ERD and NERD (P = 0.6269). Scores remained similar irrespective of the presence of esophagitis or IBS-like symptoms (Figure 4). In contrast, baseline symptom scores for “lower abdominal complaints” were statistically significantly different in patients with ERD compared with those with NERD (1.1 vs 1.3, P = 0.0012). Furthermore, in both the ERD and NERD subgroups, patients with IBS-like symptoms had a significantly higher baseline score than those without IBS-like symptoms (both P < 0.0001, Figure 4).
There were no statistically significant differences in changes from baseline for the dimension “acid complaints” at Week 4 or Week 8 in ERD or NERD patients with IBS-like symptoms compared with those without IBS-like symptoms (Table 2). Similarly, for patients with ERD, pre-post differences in the dimension “lower abdominal complaints” did not statistically differ in those with IBS-like symptoms compared with those without IBS-like symptoms at either timepoint. In contrast, NERD patients with IBS-like symptoms showed significantly higher pre-post differences in the dimension “lower abdominal complaints” at Week 4 (P = 0.049) and Week 8 (P = 0.0092) than did NERD patients without IBS-like symptoms (Table 2). Furthermore, for both ERD and NERD patients a higher increase of the pre-post differences could be shown between Week 4 and Week 8 for patients with IBS-like symptoms.
Using a pragmatic trial design, we investigated the influence of IBS-like symptoms on treatment response to pantoprazole and symptom burden in patients with GERD in a real-life setting. To represent the situation in real life clinical practice, patients were identified as suffering from GERD solely by their symptomatology, i.e. without knowledge of presence/absence of esophageal lesions. All patients then underwent upper GI endoscopy at baseline to determine whether they had ERD or NERD and to grade GERD (LA classification). Consistent with a pragmatic design, the presence of IBS-like symptoms was determined by the investigator by answering “yes”, “no”, or “I do not know” to the question: “Is it possible that this patient does not only suffer from GERD-related symptoms, but also from symptoms caused by Irritable Bowel Syndrome (IBS)?”. This is reflective of real life clinical practice in many countries where general practitioners may not be familiar with the Rome III criteria and IBS is largely diagnosed based on patient history[29,30]. Similarly, so as to reflect ordinary practice, pragmatic trials do not usually monitor patient compliance with trial medication in the way that is necessary in most explanatory trials[31]. Consequently, we did not do so. Results demonstrated a significantly higher occurrence of IBS-like symptoms in patients with NERD than in those with ERD. The presence of IBS-like symptoms reduced response to PPI treatment in patients with GERD, irrespective of endoscopic diagnosis of ERD or NERD. However, IBS-like symptoms may also show substantial improvement with placebo, making the lack of a placebo arm a limitation of this study. Nonetheless, results are reflective of what may be expected in clinical practice.
The significantly higher occurrence of IBS-like symptoms in patients with NERD (18.3%) than in those with ERD (12.7%) observed in the current study has also been shown in the literature (ERD range: 12.0%-48.0%; NERD range: 21.2%-63.6%)[15,17], although inconsistently[32,33]. However, the prevalence of IBS-like symptoms reported in the literature was generally higher than that in our study, possibly because of differences in symptom reporting and patient groups. For example, prevalence in the current study was based on the investigator’s assessment of symptoms as opposed to prevalence derived from patient-reported symptoms in the literature. Furthermore, the current investigation was restricted to patients with GERD seeking help in a real life setting in contrast with population based studies presented in the literature[34].
We demonstrated a statistically significantly lower treatment response to pantoprazole therapy in GERD patients with IBS-like symptoms than in GERD patients without these symptoms. This difference occurred in both ERD and NERD, although in the latter group statistical significance was only found after 8 wk of treatment. The response rates observed in the real life setting of this study were similar to those reported in the literature and were consistent with lowered treatment responses in patients with NERD than in those with ERD[19]. They were also consistent with data from the literature showing that the presence of IBS-like symptoms unfavourably affects the treatment response to PPIs, although data remain limited, especially in subpopulations of patients with ERD and NERD[8,15]. In the current study, the calculated response rates were based on the symptom burden assessed using the ReQuest™, whereas previous studies defined response solely based on a reduction of symptom burden[20,32,35], thus lacking a valid definition of a response threshold. Nonetheless, findings based on these two approaches are likely to be comparable.
In accordance with a previous analysis of baseline symptom burden in GERD patients[33], baseline “acid complaints” symptom scores were similar in ERD and NERD patients and in patients with and without IBS-like symptoms in the current study. Furthermore, the observed similar pre-post differences in “acid complaints” in the two GERD subgroups were expected based on previous studies using the ReQuest™, which have demonstrated similar improvements of acid-related symptoms during PPI therapy in both ERD and NERD patients[11,24,25]. This effect was independent of IBS status, which is in line with existing data[32].
In this real life setting, “lower abdominal complaints” scores at baseline were significantly higher in NERD than in ERD patients, supporting previous results from Neumann et al (2008), which showed that NERD patients suffered more frequently from IBS symptoms than did patients with ERD or Barrett’s esophagus in a small patient population[15]. Both studies contrast with earlier evaluations of the ReQuest™ database, which revealed no baseline score differences between ERD and NERD[33]. The ReQuest™ database contains data from 23 clinical studies with symptom assessment based on the ReQuest™, thus representing a selected patient population, which may account for the differences in results compared with the current study conducted under real life conditions, in which patients were included based only on their GERD symptomatology.
We also found that patients with IBS-like symptoms had significantly higher baseline scores for “lower abdominal complaints” than patients without IBS-like symptoms in both GERD subclasses, a finding concordant with previous studies[20,32]. Baseline symptom score differences between IBS+ and IBS- patients were even more pronounced than those between ERD and NERD. These results show that the investigator assessment of the presence of IBS-like symptoms was congruent with patient symptom assessment via the ReQuest™.
Lower abdominal symptoms improved with pantoprazole treatment in both ERD and NERD patients. This finding corresponds with earlier findings in therapeutic studies using PPIs as GERD treatment[28]. Interestingly, of the four subgroups, patients with NERD and IBS-like symptoms had the highest “lower abdominal complaints” symptom score at baseline and the largest clinical improvement following PPI therapy after 4 and 8 wk.
Although typical GERD symptoms, i.e. acid complaints, improved with pantoprazole therapy at 4 wk in this study, treatment response rates continued to increase from Week 4 to Week 8, suggesting that continued elevation of response rates may result from a reduction of other symptoms. These results support the concept that GERD is more than heartburn and IBS-like symptoms can be a part of the GERD symptom spectrum.
The proportion of patients with ERD in the current study was higher than what might be expected based on the literature. However, because our patients were a mix of primary and secondary care cases and came from many different countries, there is no good basis for estimating what the ERD:NERD ratio should be in this study. We can therefore only speculate on the possible explanations for the observed ratio. Symptom-based diagnosis of GERD is most reliable when heartburn and/or regurgitation are the patient’s dominant or only symptoms. When abdominal symptoms such as dyspepsia or IBS, which are more prevalent in NERD than in ERD, are also present, physicians may be less confident about making a diagnosis of GERD. Enrolment into the trial was based on “patients considered to have symptoms of GERD”; thus, recruitment may have been inadvertently biased against enrolling patients with NERD, thereby affecting the ERD:NERD ratio. Nonetheless, this possibility should not affect the validity of the conclusions as the results relate to patients in whom physicians are prepared to make the GERD diagnosis on the basis of symptoms.
In conclusion, IBS-like symptoms have a distinct influence on the response of GERD patients to treatment with the PPI pantoprazole. The presence of IBS-like symptoms reduces response rates and appears to be higher in patients with NERD than in those with ERD. The exact underlying mechanisms for this remain to be elucidated. These findings are of particular interest for the medical community as the symptom based identification of GERD is reflective of the real life situation in daily practice. The results suggest the need to enhance the awareness of physicians for the possible co-morbid occurrence of IBS symptoms in GERD to improve diagnosis and treatment of individuals bothered by this intricate complex of symptoms.
The overlap of symptomatology between gastroesophageal reflux disease (GERD) and irritable bowel syndrome (IBS) has been increasingly recognised, and one theory integrates IBS-like symptoms into the spectrum of GERD complaints. The presence of IBS-like symptoms may unfavourably affect treatment outcome in some patients with GERD, thus highlighting the importance of identifying and understanding the spectrum of symptoms influencing the treatment outcome in GERD patients in ordinary clinical practice.
Research suggests that IBS is common in patients with GERD (both ERD and NERD), although these data are from a small study of outpatients (n = 71) from only one clinic. In the current study, the authors further evaluate the interrelationship between IBS-like symptoms and GERD in a large (n = 1888), prospective, multicentre study of outpatients in a real-life setting, to help understand the spectrum of symptoms influencing the treatment outcomes for improved patient management in practice.
In a recent publication by Neumann et al (2008), IBS symptoms were common in GERD and found to be slightly more prevalent in NERD than in ERD; however, differences were not statistically significant, which may have resulted from the small sample size. The study is the largest to date to evaluate the presence of IBS-like symptoms in both ERD and NERD patients, and to establish the impact these symptoms may have on treatment response in GERD patients.
By understanding the impact of IBS-like symptoms on response to proton pump inhibitor (PPI) treatment in patients with GERD, physicians can better predict treatment response in their patients.
ReQuest™: a fully validated, reliable, self-administered symptom assessment tool for the evaluation of treatment effects in ERD and NERD. It comprises six dimensions of GERD: acid complaints, upper abdominal/stomach complaints, lower abdominal/digestive complaints, nausea, sleep disturbances, and other complaints, which are assessed for symptom intensity and symptom frequency. The ReQuest™ also includes a question about general well-being.
The authors investigated the influence of IBS-like symptoms on treatment outcomes with pantoprazole in GERD in a real life setting. The authors concluded that the presence of IBS-like symptoms influences treatment outcome and symptom burden in GERD. They also supported the theory incorporating IBS-like symptoms into the spectrum of GERD by demonstrating good PPI response. Overall, this topic would raise quite an interest with readers. In view of the rarity of studies of IBS in GERD with a pragmatic attitude, this manuscript could possibly get frequent citations by other researchers.
Peer reviewer: Myung-Gyu Choi, MD, Professor of Medicine, Division of Gastroenterology, Department of Internal Medicine, Seoul St. Mary’s Hospital, The Catholic University of Korea, 505, Banpo-Dong, Seocho-Gu, Seoul 137-040, South Korea
S- Editor Tian L L- Editor O’Neill M E- Editor Ma WH
| 1. | Talley NJ, Boyce P, Jones M. Identification of distinct upper and lower gastrointestinal symptom groupings in an urban population. Gut. 1998;42:690-695. |
| 2. | Kennedy TM, Jones RH, Hungin AP, O’flanagan H, Kelly P. Irritable bowel syndrome, gastro-oesophageal reflux, and bronchial hyper-responsiveness in the general population. Gut. 1998;43:770-774. |
| 3. | Smart HL, Nicholson DA, Atkinson M. Gastro-oesophageal reflux in the irritable bowel syndrome. Gut. 1986;27:1127-1131. |
| 4. | Nastaskin I, Mehdikhani E, Conklin J, Park S, Pimentel M. Studying the overlap between IBS and GERD: a systematic review of the literature. Dig Dis Sci. 2006;51:2113-2120. |
| 5. | Quigley E, Heading R, Monnikes H. Exploring the spectrum of GERD: myths and realities. Ann Gastroenterol. 2007;20:155-163. |
| 6. | Frissora CL, Koch KL. Symptom overlap and comorbidity of irritable bowel syndrome with other conditions. Curr Gastroenterol Rep. 2005;7:264-271. |
| 7. | Talley NJ. Overlapping abdominal symptoms: why do GERD and IBS often coexist? Drugs Today (Barc). 2006;42 Suppl B:3-8. |
| 8. | Dickman R, Feroze H, Fass R. Gastroesophageal reflux disease and irritable bowel syndrome: a common overlap syndrome. Curr Gastroenterol Rep. 2006;8:261-265. |
| 9. | Pimentel M, Rossi F, Chow EJ, Ofman J, Fullerton S, Hassard P, Lin HC. Increased prevalence of irritable bowel syndrome in patients with gastroesophageal reflux. J Clin Gastroenterol. 2002;34:221-224. |
| 10. | Gasiorowska A, Poh CH, Fass R. Gastroesophageal reflux disease (GERD) and irritable bowel syndrome (IBS)--is it one disease or an overlap of two disorders? Dig Dis Sci. 2009;54:1829-1834. |
| 11. | Bardhan KD, Stanghellini V, Armstrong D, Berghöfer P, Gatz G, Mönnikes H. International validation of ReQuest in patients with endoscopy-negative gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2004;20:891-898. |
| 12. | Glatzel D, Abdel-Qader M, Gatz G, Pfaffenberger B. Pantoprazole 40 mg is as effective as esomeprazole 40 mg to relieve symptoms of gastroesophageal reflux disease after 4 weeks of treatment and superior regarding the prevention of symptomatic relapse. Digestion. 2007;75 Suppl 1:69-78. |
| 13. | Mönnikes H, Pfaffenberger B, Gatz G, Hein J, Bardhan KD. Novel measurement of rapid treatment success with ReQuest: first and sustained symptom relief as outcome parameters in patients with endoscopy-negative GERD receiving 20 mg pantoprazole or 20 mg esomeprazole. Digestion. 2007;75 Suppl 1:62-68. |
| 14. | Stanghellini V. ReQuest: new dimensions in the assessment and management of GERD. Drugs Today (Barc). 2005;41 Suppl B:7-11. |
| 15. | Neumann H, Monkemuller K, Kandulski A, Malfertheiner P. Dyspepsia and IBS symptoms in patients with NERD, ERD and Barrett’s esophagus. Dig Dis. 2008;26:243-247. |
| 16. | Winter JW, Heading RC. The nonerosive reflux disease-gastroesophageal reflux disease controversy. Curr Opin Gastroenterol. 2008;24:509-515. |
| 17. | Wu JC, Cheung CM, Wong VW, Sung JJ. Distinct clinical characteristics between patients with nonerosive reflux disease and those with reflux esophagitis. Clin Gastroenterol Hepatol. 2007;5:690-695. |
| 18. | Mönnikes H, Doerfler H, Schmitt H, Berghoefer P, Heading R. Is the Response of GERD Patients to PPI Therapy Affected By the Presence of IBS-Like Symptoms? Gastroenterology. 2008;134:A126. |
| 19. | Fass R, Shapiro M, Dekel R, Sewell J. Systematic review: proton-pump inhibitor failure in gastro-oesophageal reflux disease--where next? Aliment Pharmacol Ther. 2005;22:79-94. |
| 20. | Zimmerman J, Hershcovici T. Bowel symptoms in nonerosive gastroesophageal reflux disease: nature, prevalence, and relation to acid reflux. J Clin Gastroenterol. 2008;42:261-265. |
| 22. | Treweek S, Zwarenstein M. Making trials matter: pragmatic and explanatory trials and the problem of applicability. Trials. 2009;10:37. |
| 23. | Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, Johnson F, Hongo M, Richter JE, Spechler SJ. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172-180. |
| 24. | Bardhan KD, Stanghellini V, Armstrong D, Berghöfer P, Gatz G, Mönnikes H. Evaluation of GERD symptoms during therapy. Part I. Development of the new GERD questionnaire ReQuest. Digestion. 2004;69:229-237. |
| 25. | Mönnikes H, Bardhan KD, Stanghellini V, Berghöfer P, Bethke TD, Armstrong D. Evaluation of GERD symptoms during therapy. Part II. Psychometric evaluation and validation of the new questionnaire ReQuest in erosive GERD. Digestion. 2004;69:238-244. |
| 26. | Stanghellini V, Armstrong D, Mönnikes H, Bardhan KD. Systematic review: do we need a new gastro-oesophageal reflux disease questionnaire? Aliment Pharmacol Ther. 2004;19:463-479. |
| 27. | Armstrong D, Mönnikes H, Bardhan KD, Stanghellini V. The construction of a new evaluative GERD questionnaire - methods and state of the art. Digestion. 2004;70:71-78. |
| 28. | Bardhan KD, Berghöfer P. Look--but also listen! ReQuest: an essay on a new validated scale to assess the outcome of GERD treatment. Digestion. 2007;75 Suppl 1:87-100. |
| 29. | Franke A, Singer MV, Dumitraşcu DL. How general practitioners manage patients with irritable bowel syndrome. Data from a German urban area. Rom J Intern Med. 2009;47:47-53. |
| 30. | Bellini M, Tosetti C, Costa F, Biagi S, Stasi C, Del Punta A, Monicelli P, Mumolo MG, Ricchiuti A, Bruzzi P. The general practitioner’s approach to irritable bowel syndrome: from intention to practice. Dig Liver Dis. 2005;37:934-939. |
| 31. | Godwin M, Ruhland L, Casson I, MacDonald S, Delva D, Birtwhistle R, Lam M, Seguin R. Pragmatic controlled clinical trials in primary care: the struggle between external and internal validity. BMC Med Res Methodol. 2003;3:28. |
| 32. | Nojkov B, Rubenstein JH, Adlis SA, Shaw MJ, Saad R, Rai J, Weinman B, Chey WD. The influence of co-morbid IBS and psychological distress on outcomes and quality of life following PPI therapy in patients with gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2008;27:473-482. |
| 33. | Fass R, Stanghellini V, Monnikes H, Bardhan K, Berghöfer P, Sander P, Armstrong D. Baseline analysis of symptom spectrum in GERD clinical trial patients: results from the ReQuest™ database. Gastroenterology. 2006;130:A629. |
| 34. | Jung HK, Halder S, McNally M, Locke GR, Schleck CD, Zinsmeister AR, Talley NJ. Overlap of gastro-oesophageal reflux disease and irritable bowel syndrome: prevalence and risk factors in the general population. Aliment Pharmacol Ther. 2007;26:453-461. |