Published online Jun 28, 2011. doi: 10.3748/wjg.v17.i24.2972
Revised: February 9, 2011
Accepted: February 16, 2011
Published online: June 28, 2011
Chronic intestinal pseudo-obstruction (CIPO) is a rare disease due to a severe gastrointestinal motility disorder which may mimic, on both clinical and radiological grounds, mechanical obstruction. We report a case of a 26-year-old woman who presented to our institution for plain abdominal radiography for referred long-lasting constipation with recurrent episodes of abdominal pain and distension. At X-ray, performed both in the upright and supine position, an isolated air-fluid level was depicted in the left flank, together with a number of radiological signs suggestive of pneumoperitoneum. First, subphrenic radiolucency could be observed in the upright film. Second, the intestinal wall of some jejunal loops appeared to be outlined in the right flank. Third, the inferior cardiac border was clearly depicted in the upright film. The patient however had no evidence of peritoneal signs but only hypoactive bowel movements. Unenhanced multi-detector computed tomography (MDCT) of the abdomen and pelvis was therefore performed. MDCT revealed abnormal air-driven distension of the small and large bowel, without evidence of extra-luminal air. All radiological signs of pneumoperitoneum turned out to be false-positive results. The patient was submitted to pan-colonoscopy and to anorectal manometry to rule out Hirshprung’s disease, and was finally discharged with a diagnosis of CIPO.
- Citation: Camera L, Calabrese M, Sarnelli G, Longobardi M, Rocco A, Cuomo R, Salvatore M. Pseudopneumoperitoneum in chronic intestinal pseudo-obstruction: A case report. World J Gastroenterol 2011; 17(24): 2972-2975
- URL: https://www.wjgnet.com/1007-9327/full/v17/i24/2972.htm
- DOI: https://dx.doi.org/10.3748/wjg.v17.i24.2972
Chronic intestinal pseudo-obstruction (CIPO) is a rare motility disorder of the gastrointestinal (GI) tract that is usually observed in a number of different neuropathies, mesenchymopathies or myopathies, but it can also be idiopathic[1]. It is characterized by failure of the GI tract to propel its content and may result in a clinical picture mimicking mechanical obstruction, with patients complaining of recurrent episodes of abdominal distension, with or without abdominal pain, nausea and vomiting[2].
The diagnosis of CIPO is mainly clinical and is usually postulated after exclusion of any organic lesion occluding the gut lumen at endoscopy, while it can be supported by radiographic documentation of dilated small and/or large bowel loops, without evidence of a definite transition zone. This, in adults, is now best accomplished by multi-detector computed tomography (MDCT), which can obviate the need for unnecessary laparotomy[3]. However, plain abdominal films are one of the most important examinations in the diagnosis of CIPO in which abnormal air-driven distension of both small and large bowel is usually depicted[4].
Here, we report a case of a 26-year-old woman who presented to our institution for plain abdominal radiography as part of clinical and radiological work-up for referred long-lasting constipation with recurrent episodes of abdominal pain and distension. At X-ray, an isolated air-fluid level could be observed in the left flank region, together with a number of radiological signs suggestive of pneumoperitoneum. These could be appreciated both in the upright and supine films, but turned out to be false-positive results, as an unenhanced MDCT scan failed to show evidence of extra-luminal air in the peritoneal cavity.
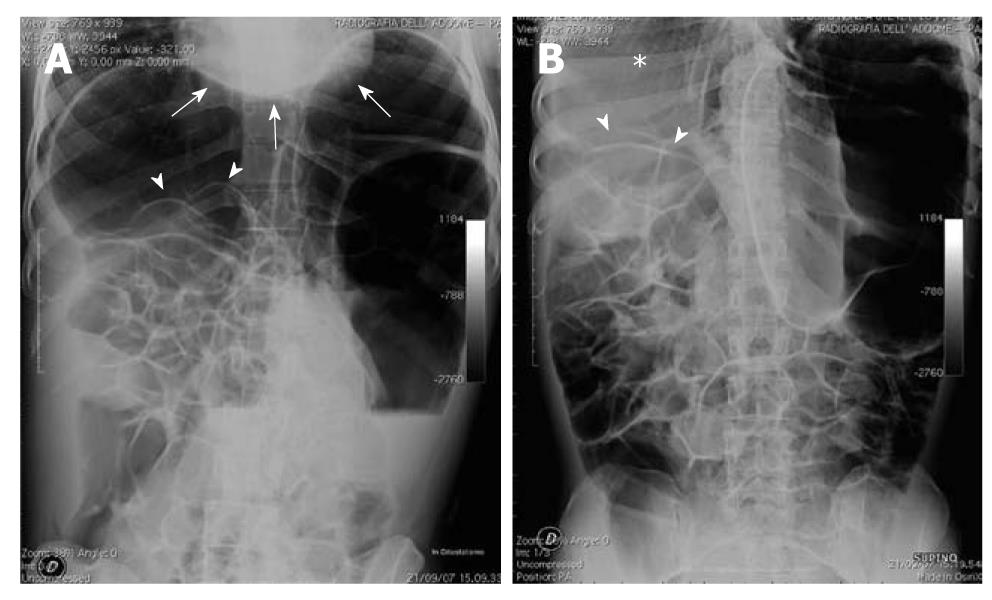
A 26-year-old woman with a history of recurrent episodes of abdominal pain and distension came to our institution to undergo plain abdominal radiography. Abdominal plain films were obtained both in the upright (Figure 1A) and supine (Figure 1B) position. The upright film showed an isolated air-fluid level in the left flank region, consistent with an obstruction of the descending colon, together with a number of X-ray findings suggestive of pneumoperitoneum. First, subphrenic radiolucencies were clearly depicted on both sides in the upright film. Second, the inferior cardiac border could be observed from the cardiac apex to the inferior vena cava. Third, the intestinal wall of some jejunal loops appeared to be outlined in the right flank (Figure 1A). This latter finding was also evident in the supine film, configuring the so-called bas-relief or Rigler’s sign together with the lack of normal hepatic shadow in the right subphrenic space, the so-called hyperlucent liver sign (Figure 1B). Based on these X-ray findings, the on-call radiologist immediately contacted the referring physician to communicate a diagnosis of pneumoperitoneum.
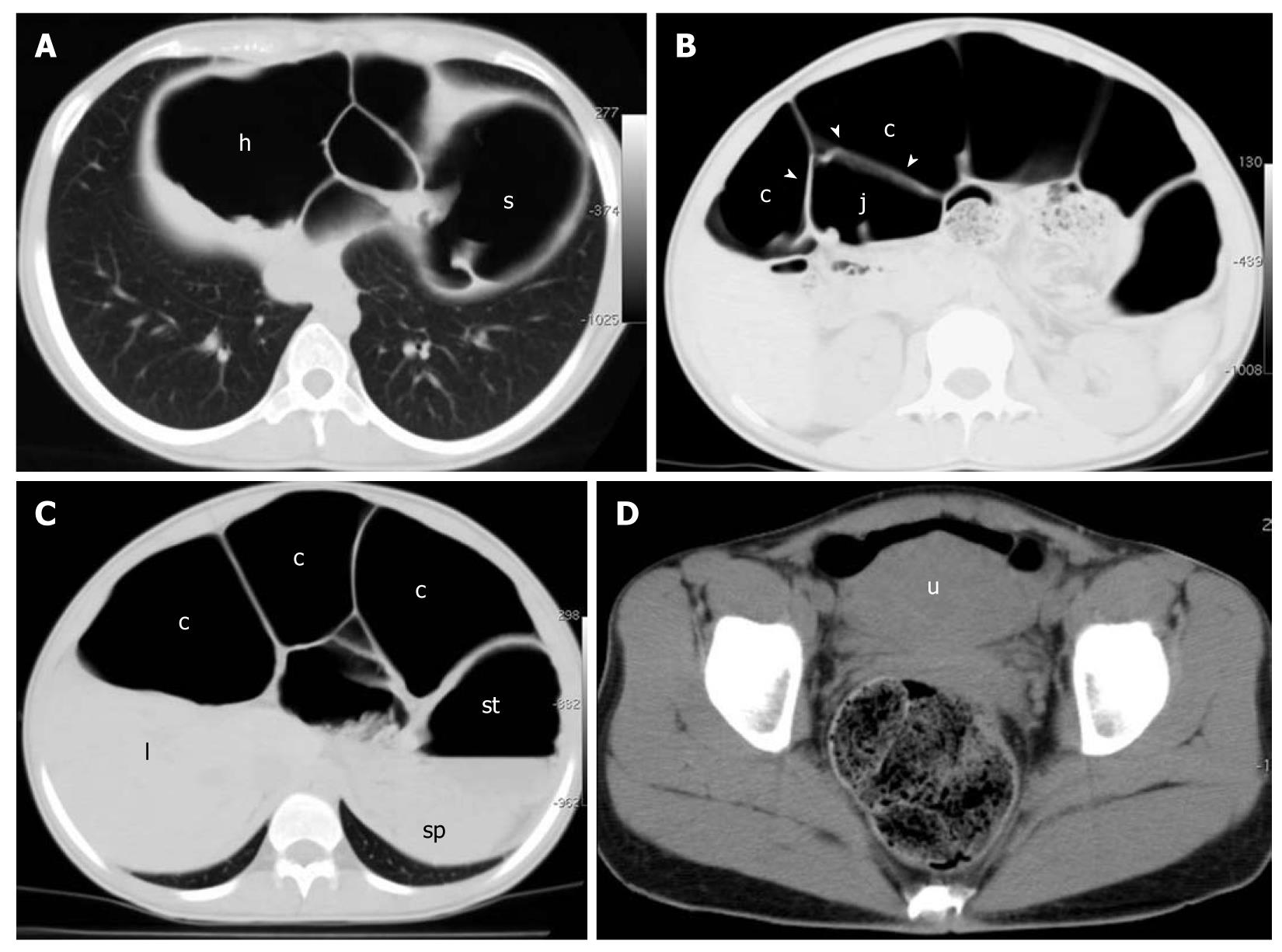
At physical examination, however, only a large abdominal distension with hypoactive bowel could be observed, but no peritoneal signs. It was therefore agreed upon to perform MDCT (Aquilion 4; Toshiba, Japan). This was performed with a detector configuration of 4 × 5 mm, table speed 30 mm/s, rotation time = 0.5 s, beam pitch = 0.75, 120 kVp, 250 mA. Only unenhanced acquisition was performed. The MDCT scan showed marked dilation of the large bowel, with both hepatic and splenic flexures displaced underneath the diaphragm (Figure 2A). Air-driven distension involved both small (Figure 2B) and large bowel (Figure 2C) loops. There was no evidence of any obstructive lesion and both the sigmoid colon and rectum were normally filled with feces (Figure 2D). No evidence of free air in the peritoneal cavity was found, therefore, a diagnosis of pneumoperitoneum could not be confirmed.
Further clinical, biochemical and instrumental investigation involving pan-colonoscopy and anorectal manometry revealed no underlying causes, and the patient was finally discharged with a diagnosis of CIPO.
Pneumoperitoneum is usually referred to as the presence of free air within the peritoneal cavity. Its radiological diagnosis usually relies on the evidence of typical subphrenic radiolucency in the posterior-anterior projection taken in the upright position[5]. As a result, the term pseudopneumoperitoneum is used when the subphrenic radiolucency does not correspond to free intraperitoneal air[6], but can be traced to either subphrenic fat pad[7] or basal lung atelectasis[8]. In these cases, the clarifying role of CT has been acknowledged[9].
To the best of our knowledge, whereas the possible occurrence of pneumoperitoneum in CIPO has been described[10], the occurrence of pseudopneumoperitoneum in CIPO has not been reported to date. In our case, subphrenic radiolucency depicted in the upright film (Figure 1A) was due to hepatic and splenic colonic flexures abnormally dilated and displaced below the diaphragmatic shadows, as shown by CT (Figure 2A).
In the emergency setting, prompt recognition of radiological signs of pneumoperitoneum in the anterior-posterior projection taken in the supine position may be of diagnostic value because it allows a confident diagnosis of pneumoperitoneum whenever an L-L projection is not available or cannot be performed[11].
These radiological signs, which can be mostly traced to either the intestinal wall[12] or various peritoneal folds[13-15], outlined by the presence of free air within the peritoneal cavity, have been recently revised and classified into four major categories as bowel-related signs, right upper quadrant signs, peritoneal ligament signs, and other signs[16].
For at least one of these signs, namely the Rigler’s sign, the possible occurrence of false-positive cases is well acknowledged. Rigler’s sign can be simulated by two contiguous, moderately dilated and air-filled loops of bowel, whereby intraluminal air in one loop of bowel may appear to outline the wall of the adjacent loop[17]. These false-positives cases, however, have only been reported in the supine film where the sign itself was originally described[12]. To the best of our knowledge, the occurrence of a false-positive Rigler’s sign in the upright position has never been described. As shown by MDCT, the intestinal wall of some jejunal loops was in our case outlined by intraluminal air in the large bowel, which was abnormally dilated (Figure 2B). The anomalous dislocation of jejunal loops in the right flank was not further investigated, although it was likely due to concomitant malrotation.
Possible occurrence of false-positive results for the inferior cardiac border sign were also postulated in the original description. The inferior border of the heart becomes visible on supine radiography whenever it is outlined by air; either free air in the peritoneal cavity, such as in pneumoperitoneum, or air within the pleural and/or pericardial sac. Occasionally, gas-filled loops collected beneath the left hemi-diaphragm may simulate this sign[18]. As with Rigler’s sign, these false-positive signs are also expected to occur in the supine position and not in the upright. In our case, however, the sign could not be detected in the supine film because of suboptimal technical positioning (Figure 1B).
Finally, the hyperlucent liver sign which could be observed on the supine film (Figure 1B) also turned out to be a false-positive result because it was clearly due to the interposition of dilated, air-filled large bowel loops between the liver and the anterior abdominal wall, as shown by MDCT (Figure 2C). To the best of our knowledge, false-positive cases of hyperlucent liver sign have never been reported.
In the present case, MDCT not only ruled out the radiological diagnosis of pneumoperitoneum but it also excluded mechanical obstruction, and showed that the sigmoid colon and rectum were normally filled with feces, without evidence of a transition zone (Figure 2D). As this latter CT finding is rather atypical in patients with Hirschsprung’s disease[19], this was also excluded by anorectal manometry, which revealed a normal inhibitory rectoanal reflex[20]. The patient was therefore discharged with a diagnosis of CIPO.
We have described a case of pseudopneumoperitoneum in a patient with CIPO. All radiological findings of pneumoperitoneum that were clearly depicted in the upright and supine films turned out to be false-positive results, as shown by MDCT. To the best of our knowledge, such a case has not been reported to date.
Peer reviewer: Andrew Seng Boon Chua, MD, Department of Gastroenterology, Gastro Centre Ipoh, 1, lorong Rani, 31, lebuhraya Tmn Ipoh, Ipoh Garden South, IPOH 30350, Malaysia
S- Editor Tian L L- Editor Kerr C E- Editor Zheng XM
| 1. | De Giorgio R, Sarnelli G, Corinaldesi R, Stanghellini V. Advances in our understanding of the pathology of chronic intestinal pseudo-obstruction. Gut. 2004;53:1549-1552. |
| 2. | Stanghellini V, Cogliandro RF, De Giorgio R, Barbara G, Morselli-Labate AM, Cogliandro L, Corinaldesi R. Natural history of chronic idiopathic intestinal pseudo-obstruction in adults: a single center study. Clin Gastroenterol Hepatol. 2005;3:449-458. |
| 3. | Merlin A, Soyer P, Boudiaf M, Hamzi L, Rymer R. Chronic intestinal pseudo-obstruction in adult patients: multidetector row helical CT features. Eur Radiol. 2008;18:1587-1595. |
| 4. | Antonucci A, Fronzoni L, Cogliandro L, Cogliandro RF, Caputo C, De Giorgio R, Pallotti F, Barbara G, Corinaldesi R, Stanghellini V. Chronic intestinal pseudo-obstruction. World J Gastroenterol. 2008;14:2953-2961. |
| 5. | Miller RE. The radiological evaluation of intraperitoneal gas (pneumoperitoneum). CRC Crit Rev Clin Radiol Nucl Med. 1973;4:61-85. |
| 6. | Mokrohisky JF. Pseudopneumoperitoneum; simulated free air in the peritoneal cavity. Am J Roentgenol Radium Ther Nucl Med. 1958;79:293-300. |
| 7. | Fisher MS. The simulation of pneumoperitoneum by basal atelectasis. Br J Radiol. 1968;41:701. |
| 8. | Fataar S, Schulman A. Pseudopneumoperitoneum due to subphrenic fat. AJR Am J Roentgenol. 1981;137:391-392. |
| 9. | Nseif M, Berger A, Bely N, Zinzindohoue F, Cellier C, Frija G, Cugnenc P. False radiologic pneumoperitoneum. The value of emergency abdominal computed tomography. J Chir (Paris). 1997;134:329-331. |
| 10. | Kim HW, Chon NR, Kim YS, Kim JH, Park H. A case of spontaneous pneumoperitoneum associated with idiopathic intestinal pseudoobstruction. Korean J Gastroenterol. 2009;54:395-398. |
| 11. | Levine MS, Scheiner JD, Rubesin SE, Laufer I, Herlinger H. Diagnosis of pneumoperitoneum on supine abdominal radiographs. AJR Am J Roentgenol. 1991;156:731-735. |
| 12. | Rigler LG. Spontaneous pneumoperitoneum: A roentgenologic sign found in the supine position. Radiology. 1941;37:604-607. |
| 13. | Weiner CI, Diaconis JN, Dennis JM. The “inverted V”: a new sign of pneumoperitoneum. Radiology. 1973;107:47-48. |
| 14. | Cho KC, Baker SR. Visualization of the extrahepatic segment of the ligamentum teres: a sign of free air on plain radiographs. Radiology. 1997;202:651-654. |
| 15. | Grassi R, Catalano O, Pinto A, Fanucci A, Rotondo A, Di Mizio R. Case report: identification of the transverse mesocolon and root of small bowel mesentery; a new sign of pneumoperitoneum. Br J Radiol. 1996;69:774-776. |
| 16. | Chiu YH, Chen JD, Tiu CM, Chou YH, Yen DH, Huang CI, Chang CY. Reappraisal of radiographic signs of pneumoperitoneum at emergency department. Am J Emerg Med. 2009;27:320-327. |
| 18. | Klein DL. Visibility of the inferior heart border in pneumoperitoneum. AJR Am J Roentgenol. 1981;137:622-623. |
| 19. | Kim HJ, Kim AY, Lee CW, Yu CS, Kim JS, Kim PN, Lee MG, Ha HK. Hirschsprung disease and hypoganglionosis in adults: radiologic findings and differentiation. Radiology. 2008;247:428-434. |
| 20. | Morais MB, Sdepanian VL, Tahan S, Goshima S, Soares AC, Motta ME, Fagundes Neto U. Effectiveness of anorectal manometry using the balloon method to identify the inhibitory recto-anal reflex for diagnosis of Hirschsprung’s disease. Rev Assoc Med Bras. 2005;51:313-317. |